[box type=”bio”] Learning Point of the Article: [/box]
TAT rupture and CNC findings are rare diseases. In case of TAT X-ray of the foot to exclude tarsal coalition is recommended. Then TAT ruptures treatment is paramount. If this problem is solved and the patient is still in pain, a further treatment of the coalition can be discussed.
Case Report | Volume 8 | Issue 5 | JOCR September – October 2018 | Page 3-6| Josephine Berger-Groch, Johannes M Rueger, Alexander S Spiro. DOI: 10.13107/jocr.DOI:2250-0685.1182
Authors: Josephine Berger-Groch[1], Johannes M Rueger[1], Alexander S Spiro[2]
[1]Department of Trauma-, Hand-, and Reconstructive Surgery, University Medical Center Hamburg-Eppendorf, Martinistreet 52, 20246 Hamburg, Germany.
[2]Department of Pediatric Orthopedics, Children’s Hospital Altona, Bleickenallee 38, 22763 Hamburg, Germany.
Address of Correspondence:
Dr. Josephine Berger-Groch,
Department of Trauma-, Hand-, and Reconstructive Surgery, University Medical Center Hamburg-Eppendorf, Martinistr 52, 20246 Hamburg, Germany.
E-mail: j.berger@uke.de
Abstract
Introduction: Tibialis anterior tendon (TAT) rupture and cuboid-navicular coalition (CNC) are rare, to the best of our knowledge, only 238 cases of TAT rupture and 34 cases of CNC are described in the past century.
Case Report: A 47-year-old man came with a sudden onset of foot pain including drop foot to our department. We diagnosed a TAT rupture, which was fixed through suture. The pathologist testified degenerative changes in the tendon. In addition, a CNC was diagnosed. No extra treatment was necessary for the CNC. At the 6-year follow-up examination, the patient had no pain and went back to normal day activities (AOFAS 95/100 points).
Conclusion: We presume that, in our case, the long-term stress at the TAT through the foot deformity, caused by the CNC, may have supported the tendon rupture. CNC normally is symptom free. Therapy of a painful CNC should start with a conservative therapy. When this fails, an operation can be considered.
Keywords: Bunnell, Calcaneonavicular coalition, Foot deformity, Foot drop, Peroneal spasm, Talocalcaneal coalition.
Introduction
The tibialis anterior tendon (TAT) rupture was first described by Brüning, in 1905 [1]. Tibialis anterior (TA) tendon rupture is a relatively rare injury that has been documented primarily in case reports and small case series [2]. About 80% of the TAT ruptures are spontaneous and 20% are traumatic [3]. The closed TAT rupture mostly occurs in male patients between 60 and 70 years. The main cause is degeneration of the tendon through repeating microtrauma at the retinaculum inferior, steroids, inflammatory arthritis, goat, diabetes, infection, ischemia, or hyperparathyroidism [4]. A tarsal coalition is a connection between tarsal bones. The incidence is ~1% and the appearance of a bilateral coalition is believed to be 50% or more [5]. The most commonly seen coalitions in the foot are talocalcanar and calcaneonavicular (≥90%). The cuboid-navicular coalition (CNC) is the least reported one. Besides the congenital coalition, an acquired coalition is discussed (trauma, infection, arthritis, and tumor), but this is much more uncommon [6]. The abnormal articulation between the bones can lead to deformation of the foot with degeneration, stiffness, and pain. Asymptomatic coalitions in the adult can become symptomatic after a trauma [7]. Microfractures and bone remodeling of the coalitions have been identified to be one cause of pain activator [8].
Case Report
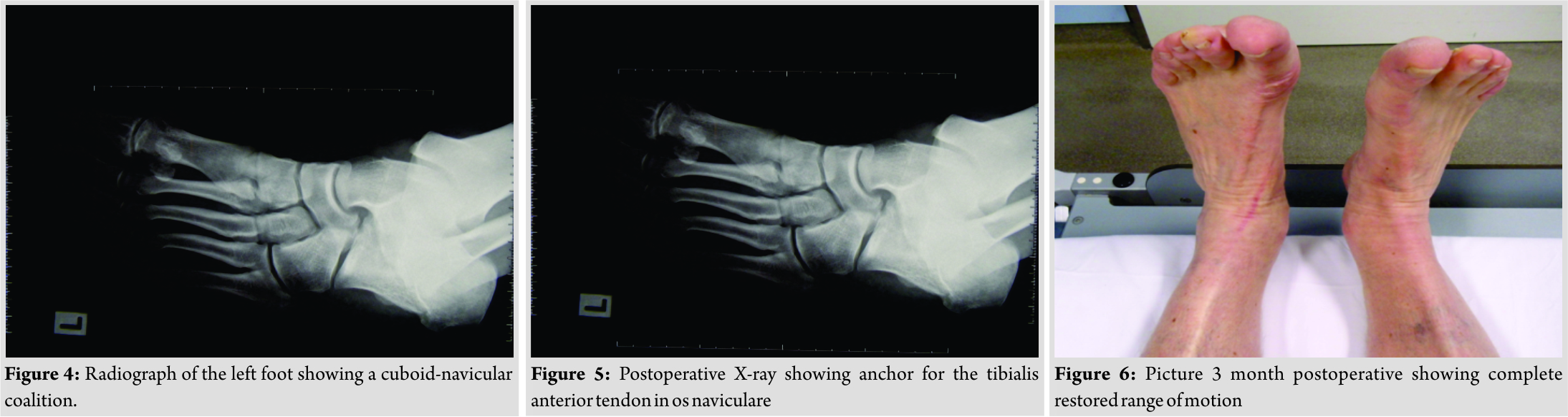
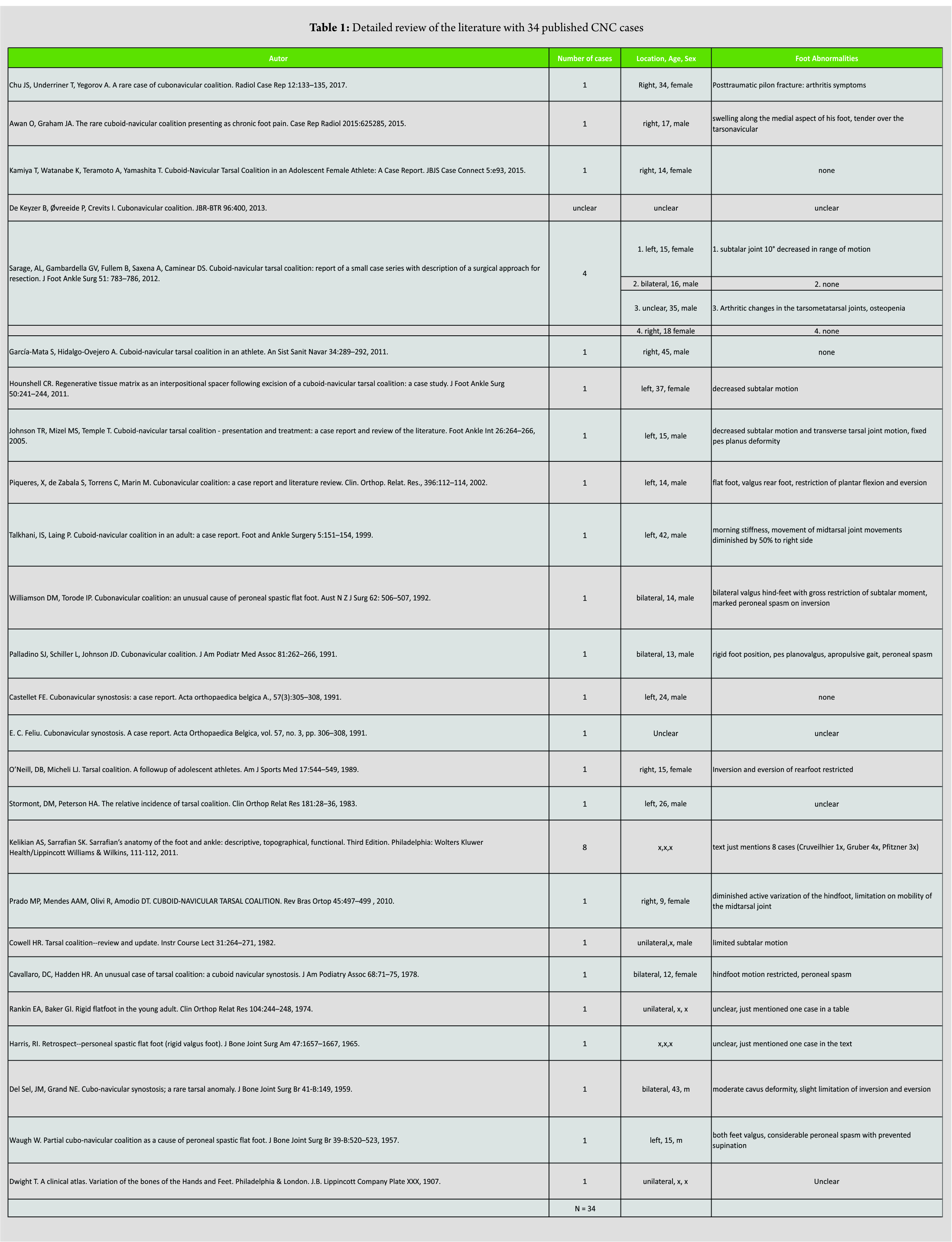
A 47-year-old male athletic patient was transferred from his local orthopedic surgeon to our department. After a firm footstep, he has heard a snap sound and afterward was unable to lift up his left foot while playing tennis. The patient has no medical history and no regular medication. At admission, the patient reported an unclear constant pain at the medial side of the left ankle for 6 weeks. On clinical examination, a swollen left ankle with pain at the dorsodistal lower leg was recognized. The skin was intact; there were no numbness and a normal perfusion. Dorsiflexion of the left ankle was reduced to 2/5 grade of muscle strength. The patient had a pes valgus and a slight pes abductus. While checking out the radiographs of both feet, we recognized a CNC on the left side and the frequently seen coalition between calcaneus and navicular bone on the right side.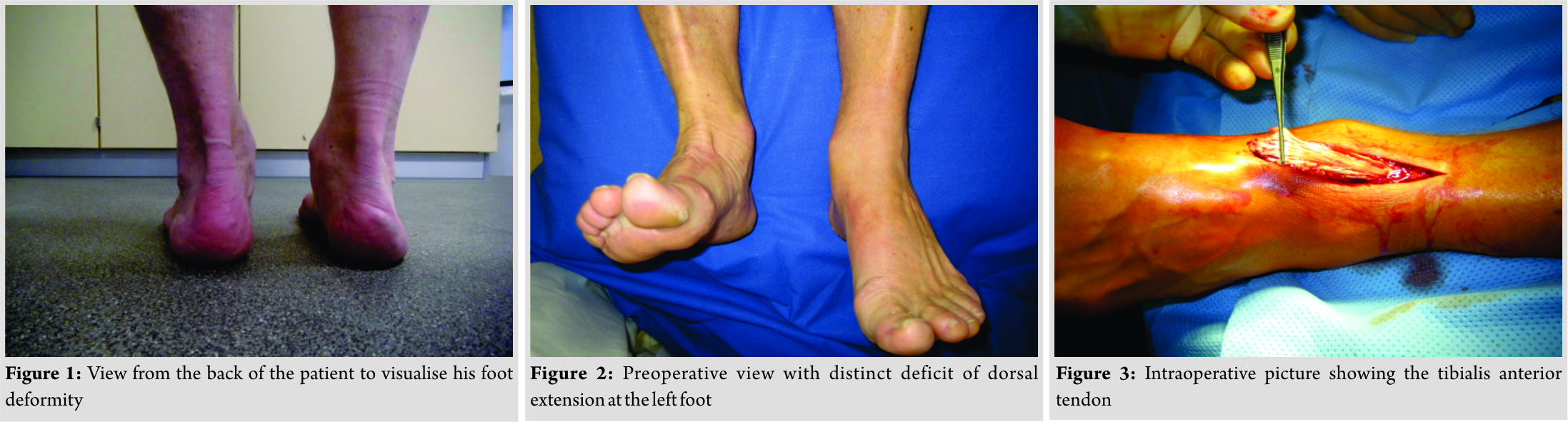
Discussion
The dorsiflexion of the foot is based on the power of the M tibialis anterior by 80% [9]. The most common area of TAT rupture is close to the retinaculum inferior. A reason could be the blood supply of the tendon. In the middle part of the anterior tendon, half exist an avascular zone 5–16 mm above the tendon insertion [10]. For active patients, a surgical treatment is recommended in case of a TAT rupture. Otherwise, persistent pain and pes planus are possible long-term problems [11]. Just bedridden patients, low demand patients, or patients with contraindications for an operation should be treated with a cast for 6 weeks [2]. However, the biggest comparing therapy – study about TAT ruptures was not able to find a difference between operative and conservative treatment [4]. The kind of operation depends on the location of the tendon rupture. A distal rupture can be fixed with a screw, while proximal lesions can be reconstructed with a direct tendon suture (Bunnell/Kessler). Different surgical procedures were used to treat delayed diagnosed ruptures: Z-plasty, different tendon transfers, and graftings. The different authors report good results. No technique can be favored as all published data are case presentations.
A detailed review of the literature showed only 34 published CNC cases (Table 1). The diagnosis of coalition is usually made by plain radiographs. The 45° medial oblique view is the best view to show a CNC [5]. Looking at the literature, 1/3 of patients coming with a painful coalition have a foot abnormality. Most frequently valgus deformity reduced mobility in the subtalar joint and peroneal spasm is found [12]. Waugh described a case with a peroneal spasm in a boy with a CNC and recommended to look carefully for coalitions in patients of a spastic flat foot [13]. Because the CNC preserves the Chopart and Lisfranc joint, chronic pain symptoms are much more uncommon then in other types of coalitions [14]. The treatment of a symptomatic CNC should start with a conservative therapy including rest, anti-inflammatory medication, and orthotic device. If no pain relief is noticed, surgery can be considered as follows:
• Simple resection of the bar
• Resection of the coalition and interposition of adipose graft or other types of interpositional spacer
• Triple arthrodesis [15].
Conclusion
We presume that, in our case, the long-term stress at the TAT through the foot deformity, caused by the CNC, may have supported the tendon rupture. CNCs normally are symptom free. Therapy of a painful CNC should start with a conservative therapy. When this fails, an operation can be considered.
Clinical Message
In conclusion, TAT rupture and CNC findings are rare diseases. A patient with both should be treated first for the TAT rupture. If this problem is solved and the patient is still in pain, a further treatment of the coalition can be discussed.
References
1. Brüning E. Zwei seltene Fälle subkutaner Sehnenzerreißung. Münch Med Wochenschr. 1928;52.
2. Sammarco VJ, Sammarco GJ, Henning C, Chaim S. Surgical repair of acute and chronic tibialis anterior tendon ruptures. J Bone Joint Surg Am. 2009;91:325–32.
3. Pagenstert G, Leumann A, Frigg A, Valderrabano V. [Achilles tendon ruptures and tibialis anterior tendon ruptures]. Orthopade. 2010;39:1135–47.
4. Markarian GG, Kelikian AS, Brage M, Trainor T, Dias L. Anterior tibialis tendon ruptures: an outcome analysis of operative versus nonoperative treatment. Foot Ankle Int. 1998;19:792–802.
5. Zaw H, Calder JDF. Tarsal coalitions. Foot Ankle Clin. 2010;15:349–64.
6. Hamel J. [Diagnosis and treatment of tarsal coalitions and synostoses in children and adolescents]. Orthopade. 2013;42:442–8.
7. Thorpe SW, Wukich DK. Tarsal coalitions in the adult population: does treatment differ from the adolescent? Foot Ankle Clin. 2012;17:195–204.
8. Kumai T, Takakura Y, Akiyama K, Higashiyama I, Tamai S. Histopathological study of nonosseous tarsal coalition. Foot Ankle Int. 1998;19:525–31.
9. Scheller AD, Kasser JR, Quigley TB. Tendon injuries about the ankle. Orthop Clin North Am. 1980;11:801–11.
10. Petersen W, Stein V, Tillmann B. Blood supply of the tibialis anterior tendon. Arch Orthop Trauma Surg. 1999;119:371–5.
11. Harkin E, Pinzur M, Schiff A. Treatment of Acute and Chronic Tibialis Anterior Tendon Rupture and Tendinopathy. Foot Ankle Clin. 2017;22:819–31.
12. Harris RI. Retrospect–personeal spastic flat foot (rigid valgus foot). J Bone Joint Surg Am. 1965;47:1657–67.
13. WAUGH W. Partial cubo-navicular coalition as a cause of peroneal spastic flat foot. J Bone Joint Surg Br. 1957;39-B:520–3.
14. García-Mata S, Hidalgo-Ovejero A. Cuboid-navicular tarsal coalition in an athlete. An Sist Sanit Navar. 2011;34:289–92.
15. Sarage AL, Gambardella GV, Fullem B, Saxena A, Caminear DS. Cuboid-navicular tarsal coalition: report of a small case series with description of a surgical approach for resection. J Foot Ankle Surg. 2012;51:783–6.
 |
 |
 |
| Dr. Josephine Berger-Groch | Dr. Johannes M Rueger | Dr. Johannes M Rueger |
| How to Cite This Article: Berger-Groch J, Rueger J M, Spiro A S. Rare Combination of a Cuboid-navicular Tarsal Coalition with a Closed Tibialis Anterior Tendon Rupture: A Case Report and Review of the Literature. Journal of Orthopaedic Case Reports 2018. Sep-Oct ; 8(5):3-6. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com