[box type=”bio”] Learning Point of the Article: [/box]
Fracture secondary to trivial trauma should be evaluated for pathological fracture.
Case Report | Volume 8 | Issue 5 | JOCR September – October 2018 | Page 54-56| Suresh Pillai. DOI: 10.13107/jocr.2250-0685.1210
Authors: Suresh Pillai[1]
[1]Department of Spine, Aster MIMS Hospital, Govindapurasam, Calicut, Kerala, India.
Address of Correspondence:
Dr. Suresh Pillai, PREETHI, Opposite Kseb, Court Junction, Mavelikkara, Alapuzha, Kerala, India.
E-mail: sureshorth@gmail.com
Abstract
Introduction: Pathological fractures resulting from trivial trauma may be overlooked, especially, when it is after a road traffic accident.
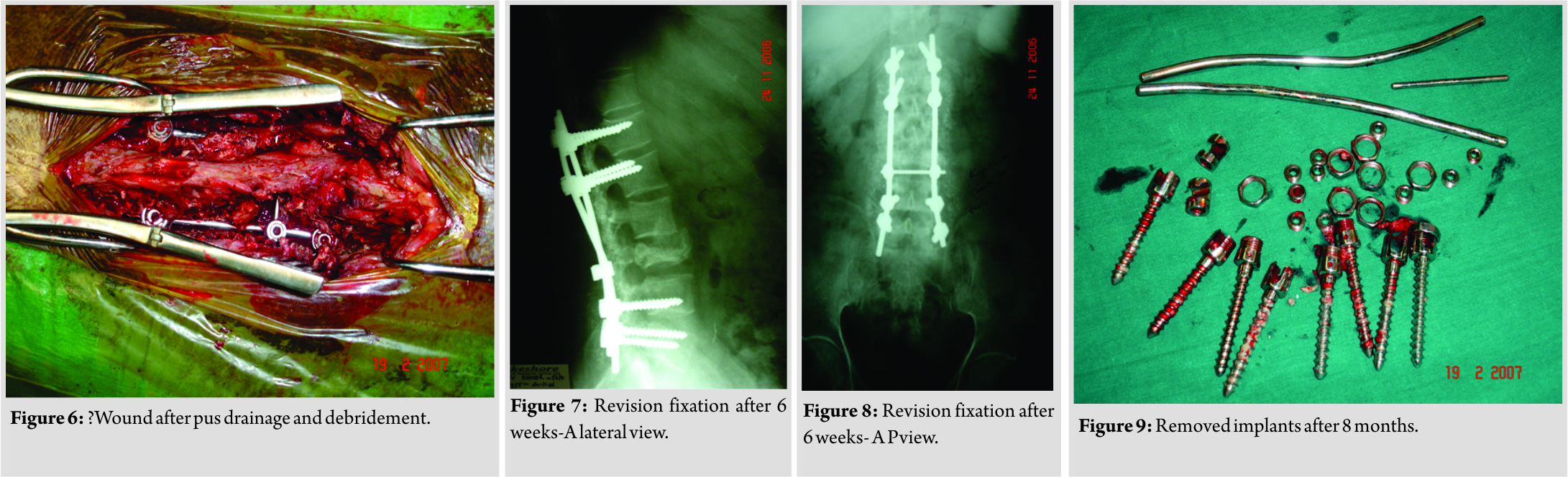
Case Report: A 56-year-old male was operated elsewhere for burst fracture L3 vertebra following a trivial road traffic accident. Due to the persistence of symptoms, he was reevaluated. Magnetic resonance imaging revealed infection at the operated site. The implants were removed, pus drained, and a transpedicular biopsy was taken from L3 vertebral body along with bone marrow aspirate from the iliac crest, suspecting a pathological fracture. He was diagnosed to have multiple myeloma and was treated in consultation with medical oncology department. His spine was stabilized 6 weeks later when the infection healed. He was further treated at the medical oncology department for multiple myeloma. Then, he developed infection again and underwent implant removal and wound debridement. 3 weeks later, he developed electrolyte imbalance and infection and succumbed to the disease.
Conclusion: Pathological fracture should be suspected in fractures resulting from trivial trauma. Multiple myeloma patients have a higher chance of infection with MRSA. With chemotherapy, the immunity goes further down resulting in florid infection.
Keywords: Pathological fracture, Multiple myeloma, MRSA, Implant loosening.
Introduction
Fractures following trivial trauma should be evaluated for pathological fractures. It is better to avoid the removal of posterior elements of the spine in cases of burst fractures to avoid conversion of 180° instability to 360° instability. Here is a report of such a wrongly treated case of multiple myeloma in a 56-year-old man.
Case Report
A 56-year-old gentleman presented with severe back pain throughout day and night and was unable to walk. He sustained burst fracture at L3 vertebra following a trivial fall in a road traffic accident. He was operated for the same elsewhere with pedicle screw fixation one level above and below the fracture(Fig. 1). The posterior elements of L3 were also found to be removed during the primary operation 70 days back. On examination, the patient had severe local tenderness at the operated site. X-ray showed fracture fixation. Erythrocyte sedimentation rate was 70 mm/1st h. C-reactive protein was 100.Due to his rest pain and night pain, a pathological fracture was suspected. Magnetic resonance imaging (MRI) of the spine (Fig. 2,3) and X-ray of the skull showed punched out lesions(Fig. 4).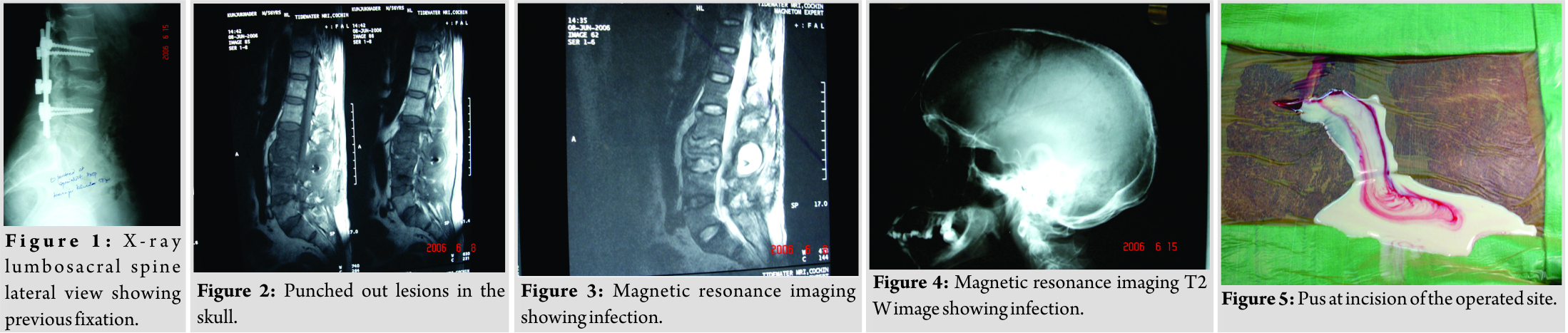
Discussion
Pathological fractures happen secondary to trivial trauma. Hence, in all cases of trauma, the possibility of pathological fracture should be kept in mind. When the cell-mediated immunity goes down, the chances of infection flare up[2, 5, 4, 8].This is, especially, true in multiple myeloma where these patients are prone to infections with MRSA. The posterior elements of the spine should not be removed in cases of burst fractures to avoid conversion of a 180° instability to a 360° instability. In a burst fracture, it is wiser not to remove the posterior elements to avoid a 360° instability. When the posterior elements are removed, the anterior column should be recreated as 80% of the weight is borne through the vertebral bodies. In the lumbar spine burst fractures, two-level fixation above and at least one-level below the fracture is recommended. In acute infection, the implants may have to be removed in cases of pyogenic infection or when the implant is loose. In chronic cases when the screw path is fully studded with granulation tissue, the implant would be loose and needs removal. Chemotherapy may be difficult in the presence of infection. Hence, medical treatment may be delayed and the disease may progress during this time.
Conclusion
Pathological fracture should be suspected in fractures resulting from trivial trauma. Multiple myeloma patients have a higher chance of infection with MRSA. With chemotherapy, the immunity goes further down resulting in florid infection. Avoid removal of posterior elements of the spine in cases of burst fractures to avoid conversion of a 180° instability to a 360° instability.
Clinical Message
Pathological fracture should be suspected in fractures resulting from trivial trauma. Avoid removal of posterior elements of the spine in cases of burst fractures.
References
1. Clark CE, Shufflebarger HL. Late-developing infection in instrumented idiopathic scoliosis. Spine 1999;24:1909-12.
2. de Boer AS, Mintjes-de Groot AJ, Severijnen AJ, van den Berg JM, van Pelt W. Risk assessment for surgical-site infections in orthopedic patients. Infect Control Hosp Epidemiol 1999;20:402-7.
3. Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg1997;86:975-80.
4. Massie JB, Heller JG, Abitbol JJ, McPherson D, Garfin SR. Postoperative posterior spinal wound infections. Clin OrthopRelat Res 1992;284:99-108.
5. Rechtine GR, Bono PL, Cahill D, Bolesta MJ, Chrin AM. Postoperative wound infection after instrumentation of thoracic and lumbar fractures. J Orthop Trauma 2001;15:566-9.
6. Richards BS. Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am 1995;77:524-9.
7. Viola RW, King HA, Adler SM, Wilson CB. Delayed infection after elective spinal instrumentation and fusion: A retrospective analysis of eight cases. Spine 1997;22:2444-51.
8. Barie PS, Eachempati SR. Surgical site infections. Surg Clin North Am 2005;85:1115-35.
9. Abbey DM, Turner DM, Warson JS, Wirt TC, Scalley RD. Treatment of postoperative wound infections following spinal fusion with instrumentation. J Spinal Disord 1995;8:278-83.
 |
| Dr. Suresh Pillai |
| How to Cite This Article: Pillai S. Postoperative Spine Infection – Postoperative MRSA Infection in a Wrongly Diagnosed Case of Spine Trauma. Journal of Orthopaedic Case Reports 2018 Sep-Oct; 8(5): 54-56. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com