[box type=”bio”] Learning Point of the Article: [/box]
This case illustrates a patient treated with suture buttons, which provide an alternative option in treating PTFJ dislocations with a reported decreased likelihood of hardware removal and faster return to work.
Case Report | Volume 8 | Issue 5 | JOCR September – October 2018 | Page 82-85| Kelechi R Okoroha, Michael C Mahan, Robert Matar, Lafi S Khalil, Jordan Paul Brand, Stuart T Guthrie. DOI: 10.13107/jocr.2250-0685.1224
Authors: Kelechi R Okoroha[1], Michael C Mahan[1], Robert Matar[2], Lafi S Khalil[1], Jordan Paul Brand[3], Stuart T Guthrie[1]
[1]Department of Orthopaedic, Henry Ford Hospital, 2799 W. Grand Blvd, Detroit, MI 48202, United States.
[2]College of Medicine, Central Michigan University, 1280 East Campus Drive, Mount Pleasant, MI 48859. United States.
[3]Department of Orthopaedic Surgery, Yale University, 800 Howard Ave, New Haven, CT 06510. United States.
Address of Correspondence:
Dr. Kelechi R Okoroha,
2799 W. Grand Blvd, Detroit, MI 48202. United States.
E-mail: krokoroha@gmail.com
Abstract
Introduction: Dislocations of the proximal tibiofibular joint (PTFJ) are a relatively rare orthopedic injury. They are often repaired with open reduction internal fixation utilizing a transfixation screw. Limited data are available concerning alternative repair methods.
Case Report: This report details a 46-year-old male who presented with an open Type IIIA comminuted mid-shaft tibia and segmental fibula fractures after being struck by a car traveling 70mph. Computed tomography confirmed comminuted and displaced tibia and fibula fractures with PTFJ dislocation as well as air tracking through the anterior compartment of the leg communicating with the knee joint. He underwent open reduction internal fixation with intramedullary nailing of his tibial shaft fracture and PTFJ syndesmosis repair with two suture buttons. X-ray at post-operative follow-up 2 years later showed complete healing without evidence of failure or hardware loosening.
Conclusion: This case illustrates a patient treated with suture buttons, which provides an alternative option in treating PTFJ dislocations with a reported decreased likelihood of hardware removal and faster return to work.
Keywords: Proximal tibiofibular, suture button, trauma, surgery.
Introduction
Proximal tibiofibular joint (PTFJ) dislocations are a relatively rare injury, occurring most commonly in sports injuries or high-velocity accidents[1]. They accompany other lower extremity injuries in a vast majority of cases but are frequently overlooked in the diagnostic work-up[2, 3]. Failure to recognize and treat PTFJ instability may cause long-term disability or failed intervention of ipsilateral leg injuries. Addressing PTFJ instability may reduce the progression of chronic dislocation and nerve palsy/pain, which would require further surgical management[2, 4]. Non-surgical management with immobilization has been described, as well as surgical management with open reduction internal fixation and tendon grafting or biceps rerouting[2, 4]. Literature concerning this topic is limited, and there does not appear to be a widely accepted consensus on optimal treatment modalities. There have been several case studies utilizing syndesmotic screw transfixation for repair[1, 2]. However, the accommodating nature of the PTFJ during ankle rotation must be considered when deciding on screw fixation [5]. The use of suture buttons for distal tibiofibular injuries has demonstrated similar efficacy to screw fixation at long-term follow-up without the potential adverse events associated with screw fixation, such as increased risk for hardware removal and surgical site infections [6, 7]. In this report, we present a rare case of open tibia fracture with air extension into the knee joint through a disrupted syndesmosis and dislocated PTFJ. This report overviews the diagnosis, management, and successful follow-up of this injury. To the best of our knowledge, there are currently no existing reports in the literature that describes PTFJ dislocation repaired with suture buttons or the injury as a pathway for contamination of the knee joint.
Case Report
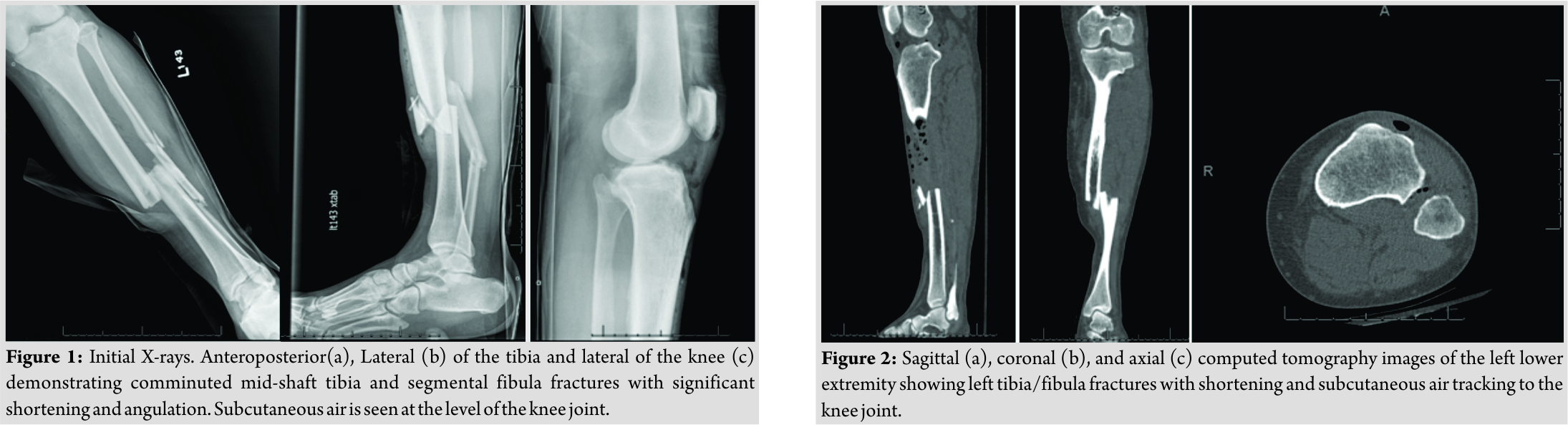
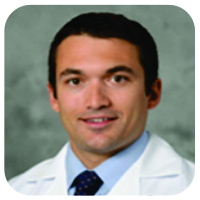
A 46-year-old male construction worker presented to the trauma bay after he was hit by a car traveling approximately 70 miles/h. The patient was stable at the time of orthopedic evaluation. Physical examination revealed tenderness along the mid-shaft of the left tibia and fibula with a 0.5-cm poke hole anteromedially and a superficial abrasion on the lateral knee. The extremity was neurovascularly intact. Radiographs (Fig. 1) and computed tomography (Fig. 2) revealed a comminuted left mid-shaft tibia and segmental fibula fractures with gas tracking throughout most of the anterior compartment, extending to the thigh and into the knee joint. In the trauma bay, the wound was irrigated with normal saline, the patient received antibiotics and tetanus vaccine, and fracture reduction followed by splinting was performed at the bedside. After informed consent was obtained, the patient underwent irrigation and debridement and open reduction and intramedullary nailing of the tibia. The PTFJ was noted to be unstable intraoperatively when manual lateral stress to the fibular head produced excessive translation laterally. Repair of the PTFJ was achieved with two suture buttons for stabilization. After surgery, the patient was placed in a knee immobilizer, started on low-molecular-weight heparin for deep vein thrombosis prophylaxis, and began physical therapy before he was discharged home on the post-operative day 3.
Operative details
The patient was taken to the operating room with a plan for irrigation and debridement, intramedullary nailing of the tibia and PTFJ reduction and fixation. The patient was placed in a supine position, and the extremity was prepped and draped in a sterile fashion. The open wound was noted medially, and an ellipse-type incision was made to remove the surrounding devitalized skin and provide access to the fracture site. Further dissection revealed the saphenous vein and nerve deep into the wound. These structures were carefully retracted and protected. A curette was used to debride the bone ends, and the wound was subsequently irrigated with 9L of normal saline. The tibia was provisionally realigned using point-to-point clamps. An intramedullary nail was then placed using a suprapatellar approach. The quadricep tendon was found to be intact, and a longitudinal incision was made to obtain access to the joint. A protection sleeve was placed to the proximal tibia, and the guidewire was placed under C-arm guidance. After the guidewire position was confirmed to be adequate, a ball-tipped guidewire with a small distal bend was placed into the canal and extended to the fracture site. Reduction was performed with longitudinal traction andpoint-to-point clamps previously placed at the fracture site. After obtaining satisfactory alignment, the guidewire was further extended to a site just proximal to the physeal scar. An 8-mm cutting reamer was then used to ream the canal, followed by sequential reaming to the appropriately sized nail. The intramedullary nail was then opened and inserted to the proper depth under C-arm guidance. Anteroposterior and lateral films were once again acquired to confirm reduction. Three proximal and 2 distal locking screws were then placed. After the intramedullary nail was secured, the ankle was stressed under fluoroscopic guidance, revealing a stable distal syndesmosis and ankle joint. However, on stressing the proximal syndesmosis with a lateral stress, the proximal fibula demonstrated significant lateral translation and the PTFJ was found to be unstable. A lazy-S incision was made over the proximal fibula and dissection was made down to the PTFJ and proximal fibula, with care taken to avoid injury to the common fibular nerve. The tibiofibular interface was cleaned and a K-wire was placed to achieve proper preliminary alignment. Reduction was confirmed using anteroposterior and lateral images. Two suture buttons were placed through the proximal fibula to the tibia, and the PTFJ was noted to be stable under stress per fluoroscopic evaluation. Images were compared to the contralateral extremity, and reduction was determined to be adequate. All incisions were irrigated with normal saline, a drain was placed in the subcutaneous layer, and the deep, subcutaneous, and skin layers of all incisions were closed. A wound vacuum-assisted closure was placed over the previously ellipsed area of skin at the open portion of the fracture. The patient was then admitted to the hospital and placed in a total range of motion knee immobilizer that was unlocked 0–90°. His compartments were monitored closely postoperatively. He was instructed not to bear weight on the left lower extremity and placed on low-molecular-weight heparin for deep vein thrombosis prophylaxis, and physical therapy was started during hospitalization. He was discharged on the post-operative day 3. He began 25% weight bearing at 6 weeks. Imaging studies immediately postoperatively (Fig. 3) and at 6 months follow-up revealed stable fixation and adequate healing. At 6months, the patient had returned to work, was able to walk without support, and was using a wheelchair only for transporting long distances. At the patient’s 2-year post-operative follow-up appointment, imaging studies demonstrated complete healing of the left mid-tibial and fibular diaphysis with a well-seated intramedullary nail and syndesmotic buttons proximally without evidence of hardware loosening (Fig. 4). At this time, the patient had continued working, walked without support, had a full range of motion, and was neurovascularly intact.
Discussion
In the case of our patient, a 46-year-old male sustaining comminuted tibial and fibular diaphyseal fractures with a PTFJ dislocation andsuture button fixation achieved successful stability of the PTFJ without evidence of hardware failure at 2-year follow-up. PTFJ dislocations seen in association with tibial shaft fractures have been described [2, 8]. PTFJ dislocations are a relatively rare injury and are typically repaired with syndesmotic transfixation screws or tendon reconstruction when they do occur. However, these methodologies have been associated with long-term consequences. Tendon hamstring autografting is known to cause donor site morbidity and potential weakness [9]. In their systematic review, Kruckeberg et al. found a variable return to sport rate using biceps femoris tendon rerouting, with half of the patients returning by 4 months while others required 17 months[10]. Transfixation screw stabilization may be complicated by decreased function and ankle pain due to a less forgiving construct during ankle rotation [5]. Therefore, transfixation screw stabilization often requires subsequent hardware removal, carrying with it the inherent risks of surgery, including surgical site infection and damage to neurovascular structures[2, 11]. Here, a novel method of repair using sutures buttons offers promising results. While there does not appear to be literature concerning the use of suture buttons in PTFJ stabilization, there are several studies exploring the biomechanics, efficacy, and long-term results of suture button repair in ankle syndesmosis disruption. Several biomechanical studies have demonstrated adequate ankle syndesmosis fixation and healing with suture button repair [12, 13, 14]. In addition, there have been many studies demonstrating in vivo efficacy of suture button repair for ankle injuries [11, 15]. In one prospective randomized study, malreduction rates were slightly increased with trans-syndesmotic screw fixation in comparison to suture button[15]. Another comparative study showed a superior range of motion with dorsiflexion and plantar flexion at 6- and 12-month follow-up in patients who received suture button repair for ankle syndesmosis injuries [11]. In addition, this study demonstrated the decreased incidence of symptomatic hardware requiring removal with button sutures, which may have significant economic benefits [11]. This type of fixation may also offer a quicker return to work and activity [6].
Conclusion
This case demonstrates a high-energy trauma with an associated PTFJ that was managed successfully with intramedullary nailing and suture button fixation of the syndesmosis. Suture button fixation in proximal or distal syndesmotic disruptions offers anatomic reduction of the joint with less ridged fixation, offering more normal limb biomechanics and lower incidence of hardware removal. Future studies should investigate PTFJ injury further to provide optimal management and alternative options.
Clinical Message
PTFJ dislocation repair with suture button fixation of the syndesmosis allows successful anatomic reduction of the joint with less ridged fixation, offering more normal limb biomechanics and lower incidence of hardware removal.
References
1. Herzog GA, Serrano-Riera R, Sagi HC. Traumatic proximal tibiofibular dislocation: A marker of severely traumatized extremities. J Orthop Trauma 2015;29:456-9.
2. Haupt S, Frima H, Sommer C. Proximal tibiofibular joint dislocation associated with tibial shaft fractures-7 cases. Injury 2016;47:950-3.
3. Hirschmann MT, Mauch C, Mueller C, Mueller W, Friederich NF. Lateral ankle fracture with missed proximal tibiofibular joint instability (Maisonneuve injury). Knee Surg Sports Traumatol Arthrosc 2008;16:952-6.
4. Aladin A, Lam KS, Szypryt EP. The importance of early diagnosis in the management of proximal tibiofibular dislocation: A 9-and 5-year follow-up of a bilateral case. Knee 2002;9:233-6.
5. Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 1974;101:186-91.
6. Schepers T. Acute distal tibiofibular syndesmosis injury: A systematic review of suture-button versus syndesmotic screw repair. Int Orthop 2012;36:1199-206.
7. Rigby RB, Cottom JM. Does the arthrex tightrope® provide maintenance of the distal tibiofibular syndesmosis? A 2-year follow-up of 64 tightropes(R) in 37 patients. J Foot Ankle Surg 2013;52:563-7.
8. Johnson BA, Amancharla MR, Merk BR. Dislocation of the proximal tibiofibular joint in association with a tibial shaft fracture: Two case reports and a literature review. Am J Orthop (Belle Mead NJ) 2007;36:439-41.
9. Maffulli N, Spiezia F, Oliva F, Testa V, Capasso G, Denaro V, et al. Gracilis autograft for recurrent posttraumatic instability of the superior tibiofibular joint. Am J Sports Med 2010;38:2294-8.
10. Kruckeberg BM, Cinque ME, Moatshe G, Marchetti D, DePhillipo NN, Chahla J, et al. Proximal tibiofibular joint instability and treatment approaches: A systematic review of the literature. Arthroscopy 2017;33:1743-51.
11. Seyhan M, Donmez F, Mahirogullari M, Cakmak S, Mutlu S, Guler O, et al. Comparison of screw fixation with elastic fixation methods in the treatment of syndesmosis injuries in ankle fractures. Injury 2015;46:S19-23.
12. Miller RS, Weinhold PS, Dahners LE. Comparison of tricortical screw fixation versus a modified suture construct for fixation of ankle syndesmosis injury: A biomechanical study. J Orthop Trauma 1999;13:39-42.
13. Klitzman R, Zhao H, Zhang LQ, Strohmeyer G, Vora A. Suture-button versus screw fixation of the syndesmosis: A biomechanical analysis. Foot Ankle Int 2010;31:69-75.
14. Ebramzadeh E, Knutsen AR, Sangiorgio SN, Brambila M, Harris TG. Biomechanical comparison of syndesmotic injury fixation methods using a cadaveric model. Foot Ankle Int 2013;34:1710-7.
15. Kortekangas T, Savola O, Flinkkilä T, Lepojärvi S, Nortunen S, Ohtonen P, et al. A prospective randomised study comparing tightrope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury 2015;46:1119-26.
 |
 |
 |
 |
 |
 |
| Dr. Kelechi Okoroha | Dr. Kelechi Okoroha | Dr. Robert Matar | Dr. Lafi S Khalil | Dr. Jordan Paul Brand | Dr. Stuart T Guthrie |
| How to Cite This Article: Okoroha KR, Mahan M C, Matar R, Khalil L S, Brand J P, Guthrie S T. Proximal Tibiofibular Dislocation Repaired with Syndesmotic Suture Buttons: A Case Report. Journal of Orthopaedic Case Reports 2018 Sep-Oct; 8(5): 82-85. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com