[box type=”bio”] Learning Point of the Article: [/box]
Clinical diagnosis of Ledderhose disease can be made on examination of the patient; we advise the use of MRI to identify the extent of the tumor and its excision to be done in a wide margin to prevent recurrence of the tumor.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 84-86 | Santhosh Srinivasan S, U Thygarajan, D Gokul Raj, M. Susruthan. DOI: 10.13107/jocr.2250-0685.1384
Authors: Santhosh Srinivasan S[1], U Thygarajan[1], D Gokul Raj[1], M. Susruthan[1]
[1]Department of Orthopedics, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. Santhosh Srinivasan,
Department of Orthopedics, Sri Ramachandra Medical College, Porur, Chennai, Tamil Nadu, India.
E-mail: santh5550@gmail.com
Abstract
Introduction: Ledderhose’s disease, also known asplantar fibromatosis, is a rare benign nodular hyperplasia of the plantar aponeurosis. The disease is locally aggressive and can be managed very well conservatively. In patients who present with severe pain on weight-bearing might require surgical excision.
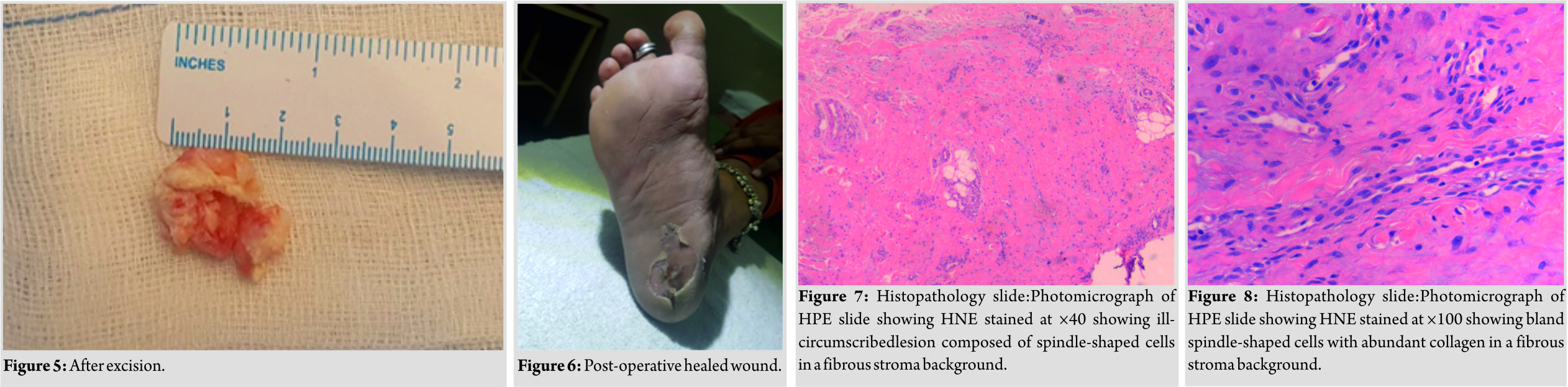
Case Report: We would like to report about a case of 40-year-old female with bilateral Ledderhose’s disease. She was treated conservatively to no avail. On surgical excision of the fibrosis tissue, the patient gives complete relief of symptoms. In this paper, we would to discuss both the conservative and surgical methods adopted to prevent post-operative complications.
Conclusion: Ledderhose disease is a rare benign aggressive disease which presents as nodules over the sole of the foot. The disease is usually manageable conservatively. Wide margin surgical excision of the nodule in severe cases will provide pain-free mobilization and prevent recurrence.
Keywords: Heel pain, Ledderhose’s disease, Plantar fibromatosis, Swelling.
Introduction
Plantar fibromatosis or Ledderhose’s disease is a benign condition of unknown etiology that was named after George Ledderhose who first described it in 1894. The disease sare characterized by localized aggressive proliferation of the connective tissue which produces collagen fibers, leading to the formation of lump or nodules over the sole of the foot. The nodule is usually slow growing and does not metastasize [1, 2]. Similar pattern of disease is noted in Dupuytren’s disease (DD)of the hand in which the palmar aponeurosis is affected. This similarity of the disease has led to Ledderhose disease to be even known as DD of the foot. The incidence of Ledderhose disease is nearly 15% in patients with Dupuytren’s [3]. Various etiological factors have been associated with plantar fibromatosis such as alcohol dependence, diabetic mellitus, liver dysfunction, use of anticonvulsants, and genetic factors. The diseases are also associated with Dupuytren’s contracture and penile fibromatosis or Peyronie’s disease [2]. The incidence of plantar fibromatosis is rare in the Indian subcontinent although previous literature explains in detail regarding the management of DD. There happens to be lesser literature for Ledderhose disease and its management. We report a case of a 29-year-old young female patient who developed bilateral foot Ledderhose disease and will discuss in detail the anatomy and various treatment options available for the same.
Case Report
A 29-year-old female patient presented to our outpatient department with a 15 years history of painful swelling over the sole both foots (R>L). The patient gives an alleged history that she was apparently normal 15 years ago when she developed a small nodular swelling over the sole of her foot. The swelling was gradually progressive and was multiple in number over her right foot. The swelling was painful and prevented the patient from weight-bearing and even walking for small distances was affected. There was no associated trauma. The patient gives no history of diabetic mellitus and epilepsy. There was no significant familial history of the disease. On examination of the patient, the feet were in plantigrade and no deformities were noted. The right foot revealed multiple nodular swellings which was tender to touch and firm in consistency with no local warmth. The skin over the swelling appeared normal. The biggest nodule measured about 2 cm in diameter. No neurovascular deficits were noted. Range of motion at the ankle and foot was within normal range. Examination of the left foot revealed a smaller nodule measuring 1 cm in diameter with local tenderness. The patient has no similar swelling elsewhere in her body. X-rays revealed no significant pathology (Fig. 1). Magnetic resonance imaging (MRI) was done to evaluate further (Fig. 2). MRI revealed a nodule in both the plantar aponeuroses. A diagnosis of bilateral foot plantar fasciitis was made and the patient was started on conservative management in the form of analgesic and anti-inflammatory drugs, physiotherapy (stretching exercise), cryotherapy, and footwear with soft insole were advised. The patient showed better results regarding pain on the left foot. 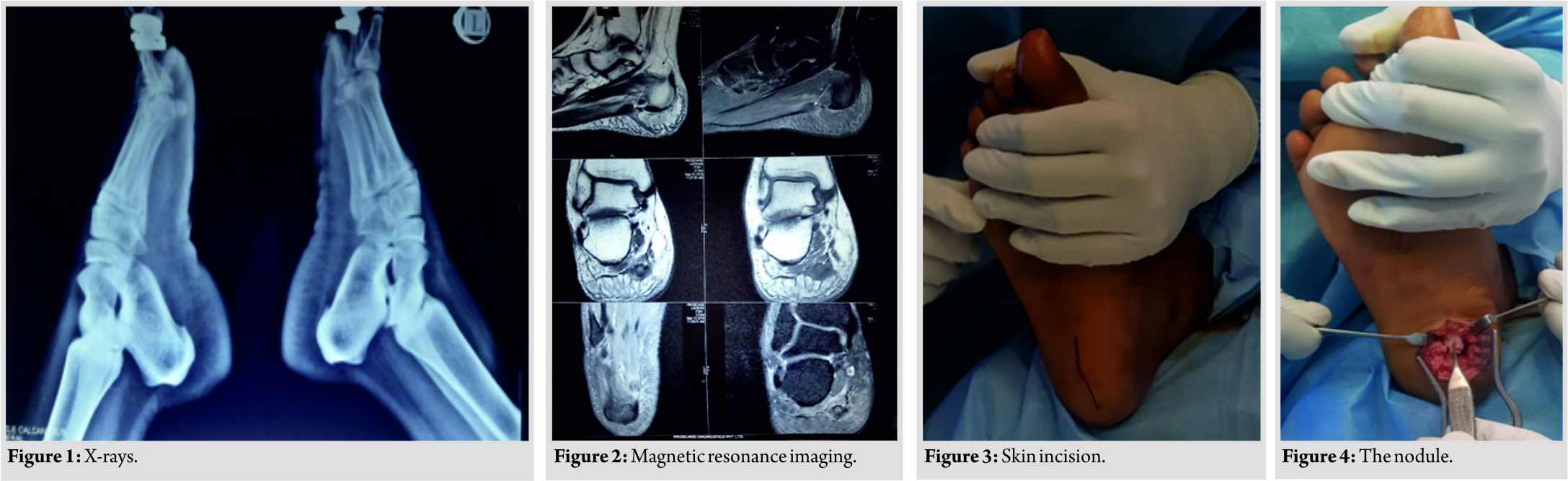
Discussion
Ledderhose disease or plantar fibromatosis is a benign aggressive infiltrative lesion which causes the plantar aponeurosis to be replaced with fibrous tissue. The importance of plantar fibromatosis in our population is to be noted as the people prefer to be walk with barefoot. The presence of nodule which tends to cause pain on weight-bearing and can to loss of the function is an indication for excision of the nodule. Skoog suggested microtrauma as a cause for plantar fibromatosis [5]. The disease is also associated with palmar fibromatosis, Peyronie’s disease, and keloids, and the presence of nodules elsewhere in the body is to be noted. Various authors have reported that epilepsy and frozen shoulder have been associated with plantar fibromatosis [6]. The disease is commonly seen in young adults and usually presents bilaterally and is commonly asymptomatic [7]. The patients have a familial history of nodules and the disease usually shows regression with age and, hence, is observed [8, 9]. Clinical diagnosis is made based on the symptom of the patient. MRI of the foot provides a non-invasive diagnostic tool and will aid in surgical planning for excision of the nodule [10]. In patients presenting with no or mild pain can be managed very well conservatively in the form of padded shoes with soft insole or tailored insoles which will redistribute the weight from the prominent nodules [1]. Inpatients who present with pain and bigger nodules will require radical excision of the nodule for pain relief [1, 11]. The rate of recurrence can be decreased with the help of adjuvant radiotherapy, but caution is advised as it is often associated with side effects [12, 2].
Conclusion
Ledderhose disease diagnosis can be made based on clinical symptoms alone. We advise the use of MRI which will help in identifying the extent and aggressive nature of the nodule. The surgical excision of the nodule is done to relieve symptoms and prevent progression of the disease. The tumor must be excised into to along with a margin of normal tissue to prevent local recurrence.
Clinical Message
Clinical diagnosis of Ledderhose disease can be made on examination of the patient; we advise the use of MRI to identify the extent of the tumor and its excision to be done in a wide margin to prevent recurrence of the tumor.
References
1. Banerjee S, Muhammad M, Nath C, Pal DK. Plantar fibromatosis: A case report. Foot Ankle Online J 2009;2:3.
2. de Bree E, Zoetmulder FA, Keus RB, Peterse HL, van Coevorden F. Incidence and treatment of recurrent plantar fibromatosis by surgery and postoperative radiotherapy. Am J Surg 2004;187:33-8.
3. Trybus M, Bednarek M, Budzyński P, Gniadek M, Lorkowski J. Concomitance of ledderhose’s disease with dupuytren’s contracture. Own experience. PrzeglLek 2012;69:663-6.
4. Curtin JW. Fibromatosis of the plantar fascia; Surgical technique and design of skin incision. J Bone Joint Surg Am 1965;47:1605-8.
5. Skoog T. Depuytren’s contraction: With special reference to aetiology and improved surgical treatment. Its occurrence in epileptics. Note on knuckle pads. ActaChirScandSuppl 1948;96:150-9.
6. Allen RA, Woolner LB, Ghormley RK. Soft-tissue tumors of the sole; Withspecialreference to plantar fibromatosis. J Bone Joint Surg Am 1955;37-A:14-26.
7. Jacob CI, Kumm RC. Benign anteromedial plantar nodules of childhood: A distinct form of plantar fibromatosis. PediatrDermatol 2000;17:472-4.
8. Godette GA, O’Sullivan M, Menelaus MB. Plantar fibromatosis of the heel in children: A report of 14 cases. J PediatrOrthop 1997;17:16-7.
9. Pijnenburg MW, Thomasse JE, Odink RJ, Hoekstra HJ. Plantar fibromatosis in infants. Ned TijdschrGeneeskd 1998;142:2638-40.
10. Halefoğlu AM. The use of magnetic resonance imaging in the diagnosis of plantar fibromatosis: A case report. ActaOrthopTraumatolTurc 2005;39:176-9.
11. Dürr HR, Krödel A, Trouillier H, Lienemann A, Refior HJ. Fibromatosis of the plantar fascia: Diagnosis and indications for surgical treatment. Foot Ankle Int 1999;20:13-7.
12. Landers PA, Yu GV, White JM, Farrer AK. Recurrent plantar fibromatosis. J Foot Ankle Surg 1993;32:85-93.
 |
 |
| Dr. Santhosh Srinivasan S | Dr. D Gokul Raj |
| How to Cite This Article: Srinivasan S S, Thygarajan U, Gokul R D. Ledderhose Disease: Pathophysiology Diagnosis and Management. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9(2): 84-86. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com