[box type=”bio”] Learning Point of the Article: [/box]
Intraosseous arteriovenous is a rare condition which can mimic osteomyelitis/tumor. This is a case report demonstrates that without hesitation it can be treated by extended curettage with good functional results.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 43-46 | M Aravindasamy, J K Giriraj Harshavardhan. DOI: 10.13107/jocr.2019.v09i05.1526
Authors: M Aravindasamy[1], J K Giriraj Harshavardhan[1]
[1]Department of Orthopaedic Surgery, Sri Ramachandra Medical College and Research Institute, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. M Aravindasamy,
Department of Orthopaedic Surgery, Sri Ramachandra Medical College and Research Institute, Sri Ramachandra Institute of Higher Education and Research, Chennai – 600 116, Tamil Nadu, India.
E-mail: aravindshallz@gmail.com
Abstract
Introduction: Introduction: Primary intraosseous arteriovenous malformations (AVMs) are rare and have only been occasionally reported. We herein report a histologically proven case of primary intraosseous AVM in the distal humerus which mimicked an osteomyelitis on radiography.
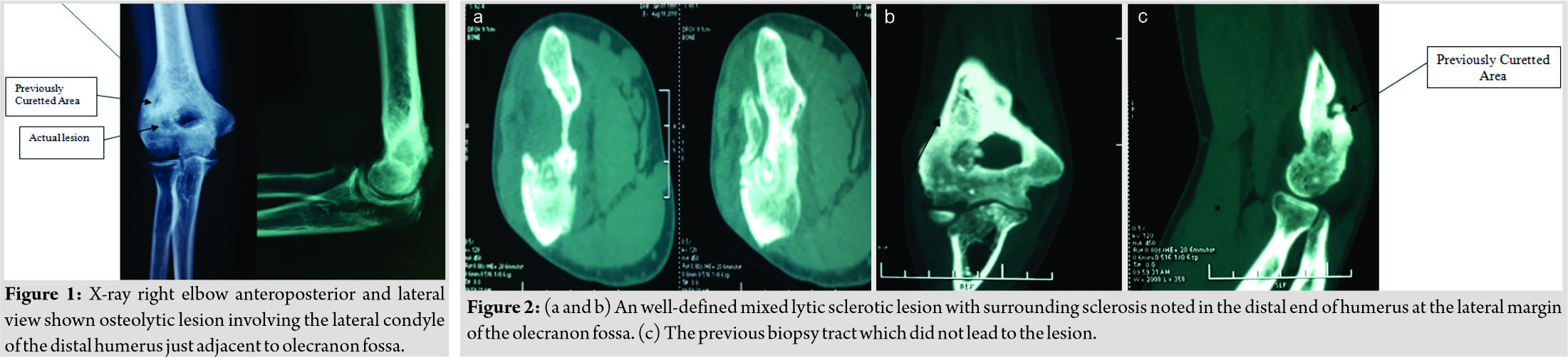
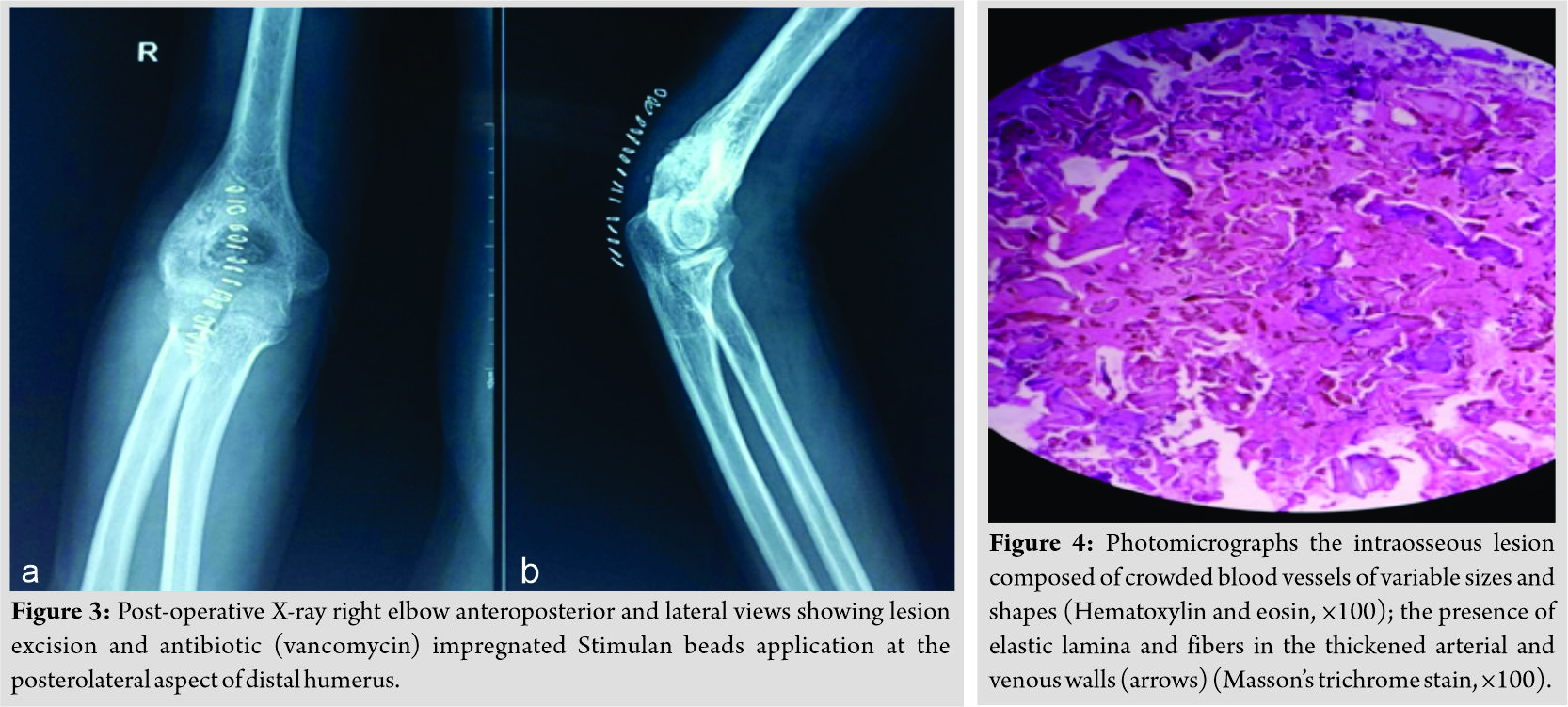
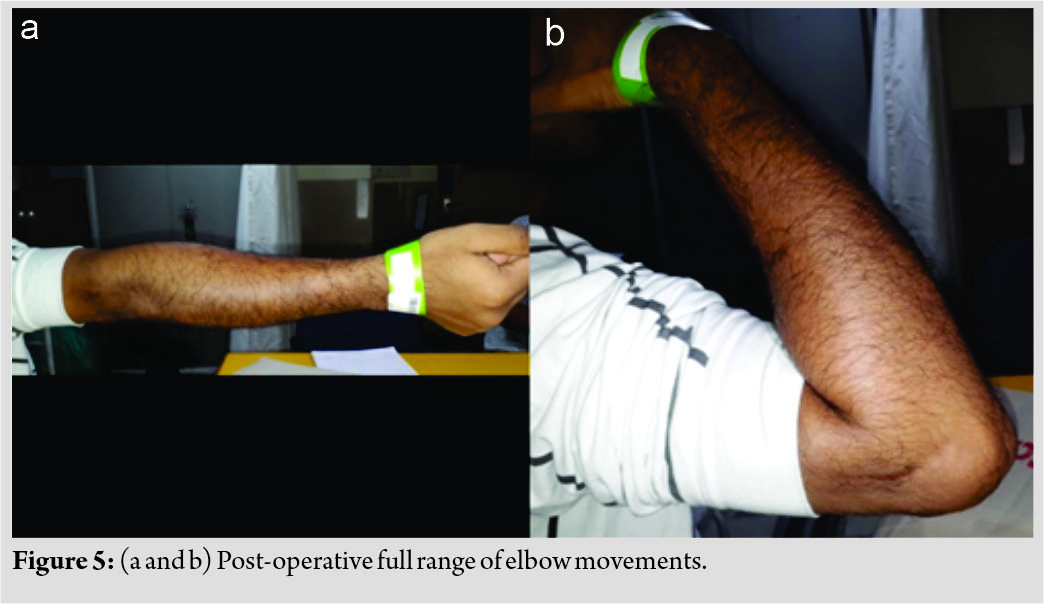
Case Report: A 27-year-old male presented with complaints of the right elbow pain and stiffness for the past 3 years. He had initially taken treatment at an outside hospital where he was suspected to have right distal humerus osteomyelitis and underwent curettage and biopsy in June 2017. He presented to us in August 2018 with persistent pain even following the first surgery. Repeat radiographs and computed tomography of the right elbow showed features of osteolytic lesion involving the right lateral humeral condyle just adjacent to olecranon fossa (Fig. 1 and 2). Through posterior triceps, splitting approach para-olecranon lesion was resected by intralesional method (burring), and vancomycin-impregnated calcium sulfate (Stimulan) beads were packed in the defect as infection was suspected (Fig. 3). Clinical improvement and restoration of full range of elbow motion were observed on follow-up. Biopsy report surprisingly suggested arteriovenous malformation.
Conclusion: Osteolytic lesion was localized in the lateral margin of the olecranon fossa (Fig. 2a and b). To reach the lesion during surgery was a major challenge as localization of the lesion was missed out by the previous surgery. The occurrence of such a condition is rare and it may take even years to correctly diagnose the disease.
Keywords: Arteriovenous malformation, distal humerus, intralesional extended curettage.
Introduction
Primary intraosseous arteriovenous malformations (AVMs) are rare, accounting for <1% of all primary intraosseous lesions. They are quite variable in their gross and microscopic presentation, yet all can be traced to anomalous development of the primitive vascular system. They may be totally asymptomatic, cosmetically disfiguring, painful, or on rare occasions, cause high-output cardiac failure. Surgical treatment is often unrewarding with recurrence not uncommon. Intra-arterial embolization has shown promising results. Peripheral symptomatic AVMs are uncommon lesion. Arrest or misdirection of the normal developmental pattern occurring at any stage can give rise to anomalous circulatory structures which can be closely correlated clinically and pathologically to the time of the insult. More than one-half of the reported cases of congenital AVMs involve the extremities. Approximately one-third of these occur in the upper extremity versus two-thirds in the lower extremity. While both soft tissue and intraosseous AVMs have identical origins, their clinical presentation and radiographic findings are quite different [1]. The diagnosis and locating the responsible lesion can be challenging and the lesion is often missed or misdiagnosed. We present a rare case of distal humerus AVMs mimicking osteomyelitis/tumor.
Case Report
A 27-year-old male came with complaints of the right elbow pain and stiffness for 3 years. The patient was apparently normal 3 years back. He started developing pain over the left elbow following a trivial trauma which was gradually progressive. The pain was dull aching and aggravated on lifting heavy weights and relieved partially by medications. The patient initially took treatment at outside hospital where he was suspected to have right distal humerus osteomyelitis and underwent curettage and biopsy in June 2017. The curettage was attempted through a lateral approach. As the lesion was in the para-olecranon region, it was probably not reached during the attempted curettage (Fig. 2c), and hence, he had persistent pain even after the surgery.
He presented to us about 1 year later (August 2018) with persistent of symptoms. Examination of the right elbow showed – healed longitudinal surgical scar of length 6 cm present over the lateral aspect of the distal humerus and elbow suggestive of a previous lateral approach, Swelling was present. Tenderness was present over the right elbow and distal humerus. Range of movement of the right elbow was 10–90° (active and passive) further restricted due to pain. Forearm rotations were full. There was no distal neurovascular deficit.
X-ray and computed tomography right elbow showed features of osteolytic lesion involving right lateral humeral condyle just adjacent to olecranon fossa (Fig. 2a and b). On September 05, 2018, through posterior triceps splitting approach lesion, we visualized the olecranon fossa. Preoperatively, olecranon fossa was not breached, and hence, at lateral margin of olecranon fossa was burred to reach the lesion. A bit of red tissue like granulation tissue was identified and curetted out. After extended curettage of lesion with burr, the defect was packed with bone substitute vancomycin-impregnated calcium sulfate (Stimulan) beads as we suspected infection (Fig. 3). Surprisingly, the biopsy was reported as an intraosseous arteriovenous malformation (Fig. 4). Culture of the tissue showed no growth, following surgery, the patient had excellent relief of pain. Postoperatively, the patient was followed up at 1 month, 3 months, 6 months, and 1 year and he gradually recovered full range of elbow motion with incorporation of bone graft substitutes (Fig. 5).
Discussion
Vascular anomalies are classified as hemangiomas and vascular malformations. The most commonly used system for biological classifications of vascular anomalies is that by Mulliken and Glowacki. This system categorizes vascular anomalies into either tumors (principally hemangiomas) or malformations, based on clinical and histological findings. Vascular malformations may present at birth and enlarge proportionately with the growth of the child. They are the result of errors in morphogenesis and are divided into subtypes such as capillary, venous, lymphatic, arterial, and combined forms, based on the constituent vessels involved. Malformations may be further subcategorized based on flow characteristics. High-flow lesions consist of any malformation with an arterial component (e.g., AVMs and arteriovenous fistulas).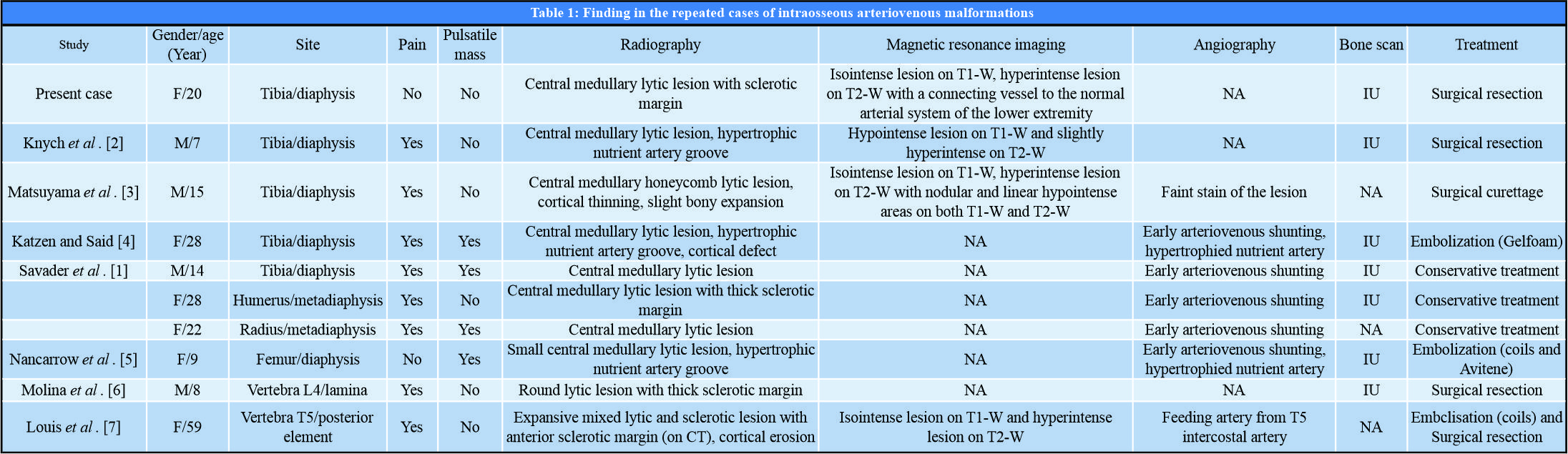
Conclusion
The diagnosis of arteriovenous malformation is challenging and often misdiagnosed. Extended curettage of the lesion can be done without hesitation to ablate the lesion. Due to the non-specific nature of the presenting symptoms, the condition is often detected late sometimes after years. Proper pre-operative planning, approach, and histology led us to the diagnosis of arteriovenous malformation.
Clinical Message
Osteolytic lesion was localized in the lateral margin of the olecranon fossa. To reach the lesion during surgery was a major challenge as localization of the lesion was missed out by the previous surgery. The occurrence of such a condition is rare and it may take even years to correctly diagnose the disease.
References
1. Savader SJ, Savader BL, Otero RR. Intraosseous arteriovenous malformations mimicking malignant disease. Acta Radiol 1988;29:109-14.
2. Knych SA, Goldberg MJ, Wolfe HJ. Intraosseous arteriovenous malformation in a pediatric patient. Clin Orthop Relat Res 1992;276:307-12.
3. Matsuyama A, Aoki T, Hisaoka M, Yokoyama K, Hashimoto H. A case of intraosseous arteriovenous malformation with unusual radiological presentation of low blood flow. Pathol Res Pract 2008;204:423-6.
4. Katzen BT, Said S. Arteriovenous malformation of bone: An experience with therapeutic embolization. AJR Am J Roentgenol 1981;136:427-9.
5. Nancarrow PA, Lock JE, Fellows KE. Embolization of an intraosseous arteriovenous malformation. AJR Am J Roentgenol 1986;146:785-6.
6. Molina A, Martin C, Muñoz I, Aguilar L, Serrano S, Ballester J, et al. Spinal intraosseous arteriovenous malformation as a cause of juvenile scoliosis. A case report. Spine (Phila Pa 1976) 1997;22:221-4.
7. Louis RG Jr., Yen CP, Mohila CA, Mandell JW, Sheehan J. A rare intraosseous arteriovenous malformation of the spine. J Neurosurg Spine 2011;15:336-9.
8. Wang HH, Yeh TT, Lin YC, Huang GS. Imaging features of an intraosseous arteriovenous malformation in the tibia. Singapore Med J 2015;56:e21-5.
 |
 |
| Dr. M Aravindasamy | Dr. J K Giriraj Harshavardhan |
| How to Cite This Article: Aravindasamy M, Giriraj Harshavardhan J K . A rare case of distal humerus intraosseous arteriovenous malformation. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 43-46. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com