[box type=”bio”] Learning Point of the Article: [/box]
Differentials of widespread osteolytic lesion, how to differentiate it and how to manage it.
Case Report | Volume 10 | Issue 2 | JOCR March – April 2020 | Page 50-53 | Shaligram Purohit, Shubhanshu Bhaladhare, Nandan Marathe, Swapneel Shah, Aditya Raj. DOI: 10.13107/jocr.2020.v10.i02.1692
Authors: Shaligram Purohit[1], Shubhanshu Bhaladhare[1], Nandan Marathe[1], Swapneel Shah[1], Aditya Raj[1]
[1]Department of Orthopaedics, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Shubhanshu Bhaladhare,
Department of Orthopaedics, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, Maharashtra, India.
E-mail: Shubhanshu.bhaladhare@gmail.com
Abstract
Introduction: Prostate cancer is one of the leading causes of death due to carcinoma in developed countries due to metastasis. Most of the patient at the time of diagnosis has shown metastasis. Metastasis to bone leads to various skeletal-related events such as fracture and neural compression leading to increase morbidity in such patients. An early diagnosis leads to favorable outcomes. Skeletal metastasis is usually presented as osteoblastic localized lesion in the spine or pelvis. Here, we like to present a case of prostatic metastasis in a patient with widespread metastasis making the diagnosis in such condition a challenging issue.
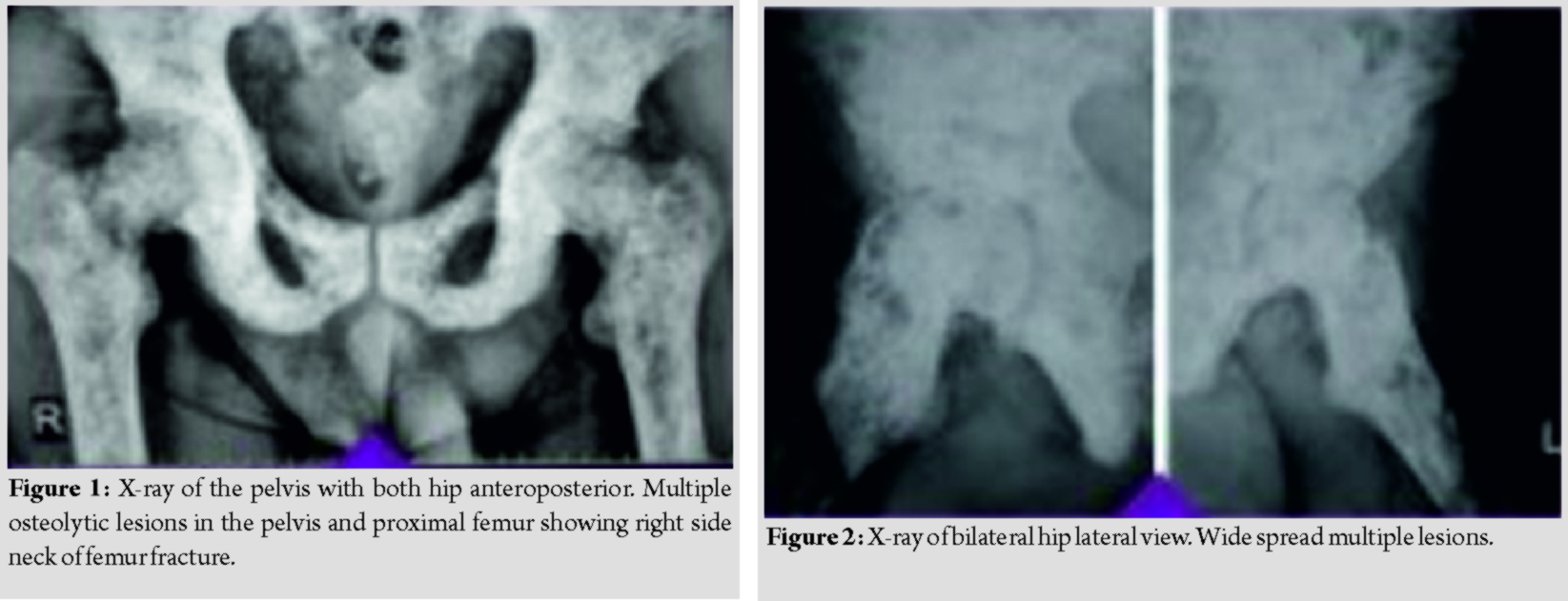
Case Report: A 61-year-old male comes with a complaint of right hip pain who has been diagnosed in some other clinic as a case of osteopoikilosis after an X-ray of the pelvis with both hips. However, on the further skeletal analysis found to involve most of the skeletal system with the diffuse osteolytic lesion. A bone scan, lab investigations helped in the arrival of diagnosis of atypical prostatic metastasis.
Conclusion: Prostate cancer is less likely to present as widespread osteolytic lesions. A very few case reports have been found in the literature regarding such presentation. This case demonstrates how to differentiate between metastasis and other common condition showing such presentation leading to an early diagnosis and thus improving the overall mortality and morbidity of the patients.
Keywords: Prostate cell carcinoma, small cell carcinoma, osteopoikilosis, multiple myeloma, metastasis, osteolytic lesions.
Introduction
Prostate cancer is one of the most common tumor seen in an adult male in developed countries while the fifth most common in developing countries [1]. Histologically, the prostatic neoplasm presents as adenocarcinoma, however histologically other types such as small cell carcinoma, basal cell carcinoma, and squamous cell carcinoma (SCC), and uroepithelial tumors also been described [2]. Small cell carcinoma of prostrate like small cell carcinoma of lungs is a neuroendocrine tumors and is one of the rare tumors. SCC is an aggressive tumor compared to adenocarcinoma of the prostate and usually presents as androgen-independent tumor [3]. Unlike adenocarcinoma of the prostate, patients of SCC of the prostate are symptomatic. Difficulty in voiding and symptoms due to metastasis such as bone pain, pathological fracture, spinal compression, and other neurological symptoms are some of the common presentations [4]. Metastasis from prostate neoplasm has a high affinity for bone (83%) compared to other sites such as a liver (66%)and lymph node (63%) [3]. Metastasis from the prostate is osteoblastic compared to other tumors [5]. Osteolytic lesions following metastasis from the prostate are very rare. We like to present a case report of widespread skeletal metastasis following secondary to prostate small cell carcinoma.
Case Report
A 61-year-old unmarried male came with the complaints of right hip pain with the inability to bear weight on the right lower limb for 1 month. There was no history of trauma or other systemic symptoms. He had consulted the local practitioner, who advised an X-ray, which was reported as osteopoikilosis (spotted bone disease) by the radiologist. He was asked to take bed rest and analgesics but the pain persisted.
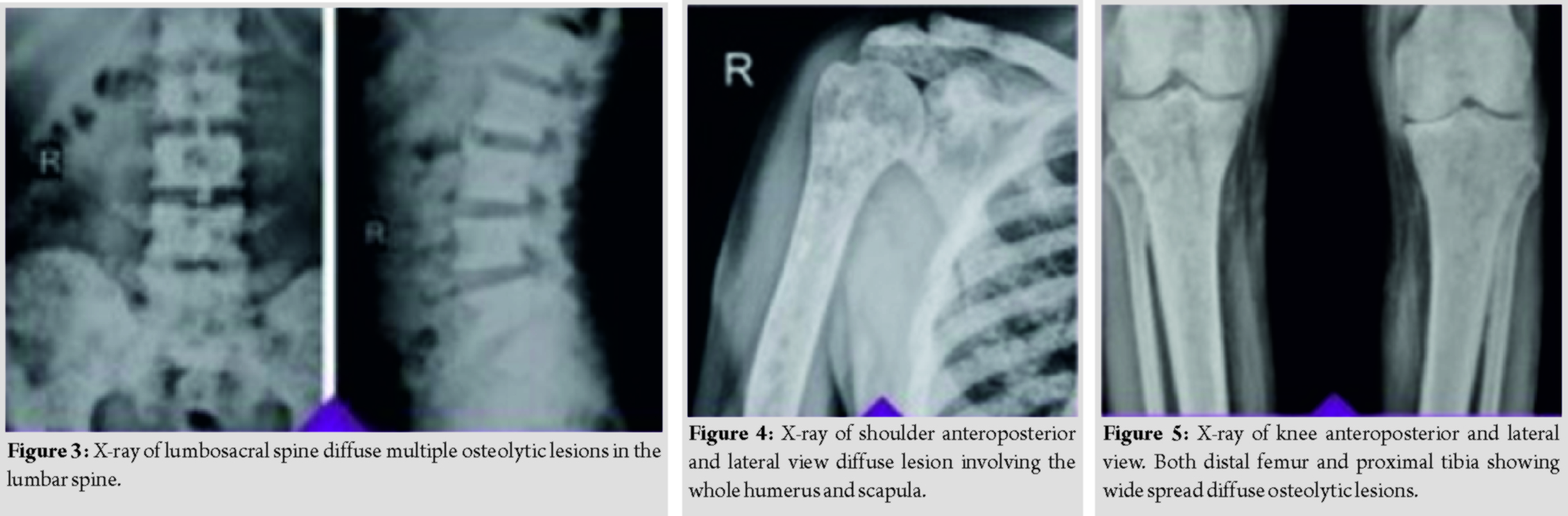
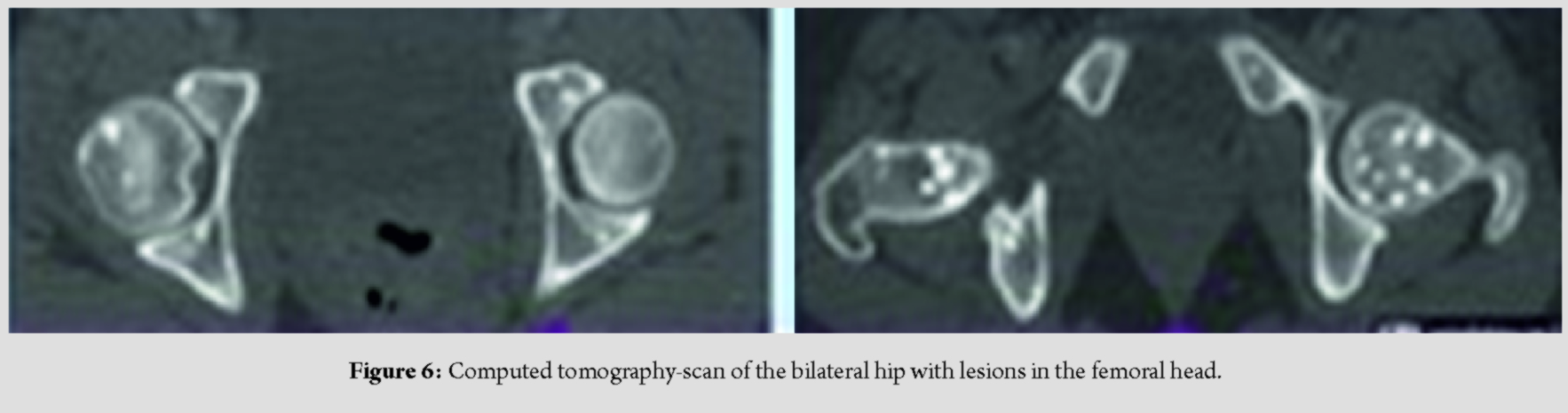
The patient then visited our tertiary center where the thorough skeletal survey was done, which showed involvement of pelvis (Fig. 1 and 2), spine (Fig. 3), and appendicular skeleton(Fig. 4 and 5) as well. The lesions were osteolytic, small, multiple, of varied sizes involving the whole of the involved bone, rather symmetrically (Fig. 6).
The X-ray with which the patient presented showed superior cortical breach in the femoral neck, but on traction X-ray, the pathological trans-cervical neck femur fracture was noted (Fig. 1). Differential diagnoses considered were metastasis, osteopoikilosis, and multiple myeloma.
Further laboratory investigations were suggestive of high alkaline phosphatase level (1933 U/L) while normal calcium, phosphorus, Vitamin D, and parathyroid hormone level. Further investigation prostate-specific antigen (PSA) was normal, 24h urinary Bence-Jones proteins negative, and bone biopsy shows immune-histochemistry positive for prostatic metastasis. A transurethral biopsy of the prostate came negative while a per-rectal biopsy of the prostate came positive for small cell carcinoma. The bone scan pattern was of super-scan while computed tomography scan showed carcinoma of the prostate with an invasion of the seminal vesicles and extension along the floor and left lateral wall of the urinary bladder leading to urethral obstruction and bilateral hydronephrosis.
The final diagnosis was extensive skeletal metastasis with primary from the prostate.
Management
In view of multiple metastatic involvements, life expectancy of the patient was limited; hence, palliative treatment in the form of cemented bipolar hemiarthroplasty was done for better ambulation and pain relief. Unfortunately, the patient died of pulmonary sepsis after 2 months.
Discussion
The skeletal system is one of the most common sites for metastasis in the case of prostate cancer(66%) [6]. Metastasis from the prostate is usually osteoblastic; however, osteolytic metastasis from prostate cancer though rare is reported in the literature. Lumbar spine and pelvis are some of the most common areas of prostate cancer spread [6]. Detection of skeletal metastasis is essential for staging, choice of therapy, and prognostication. Early diagnosis and staging improve the overall mortality rate of the patient. Diffuse metastases of prostate give a clinical picture which can be confused with multiple myeloma, osteopoikilosis. Multiple myelomas typically show a widespread diffuse osteolytic type of skeletal metastasis [7]. It is noteworthy that focal lytic lesions that give the classic radiographic appearance of multiple discrete, lytic, punched‐out, round lesions in multiple myeloma, and diffusely metastatic prostate cancer must be at least 5 mm in size to be considered as true abnormalities [8]. Other lab parameters such as serum electrophoresis, Bence-Jones proteins help in ruling out the disease. Furthermore, the bone scan in the multiple myelomas shows a cold scans which helps in the differentiation of multiple myeloma with other conditions. Osteopoikilosis also known as spotted bone disease is a rare hereditary autosomal dominant trait present in families or sometimes sporadically. There are no specific clinical features and patients are usually asymptomatic and no treatment is required for the same. Diagnosis is made by incidental typical radiological findings in patients seeking treatment for other medical problems such as fractures, dislocation, or osteoarthritis. The main pathophysiology here is an abnormality in the endochondral bone maturation process and collagen regulation, which leads to the formation of trabeculae along the lines of stress. As opposed to metastatic osteoblastic lesions, it has symmetrical distribution, the propensity for epiphyseal and metaphyseal involvement, and the uniform size of the foci along with normal alkaline and acid phosphatase and a bone scan of normal appearance with axial skeletal involvement[9, 10, 11]. In an elderly male with multiple osteolytic lesions a high-grade suspicion of metastasis from the prostate is to be made. Although the PSA level in our patient was normal, it is one of the best screening tools for prostate cancer. A normal PSA level in a prostatic malignancy is suggestive of atypical carcinoma of neuroendocrine origin mostly small cell carcinoma. Bone metastases can grow rapidly in prostate cancer. Bisphosphonates or denosumab effectively delay these complications and should be a part of the standard armamentarium in progressing metastatic patients. Lifestyle adjustments, including weight-bearing exercises, and appropriate calcium-Vitamin D intake, should be recommended to every metastatic prostate cancer patient [12, 13].
Conclusion
We like to conclude by saying that though high PSA level is indicative of metastasis from the prostate it is not always true. A patient with multiple osteolytic lesions should be considered for atypical prostate carcinoma even if the PSA level is not that much raised. This will helps in an early institution of treatment and reduces further morbidity and mortality.
Clinical Message
Although widespread metastatic osteoblastic lesion is the characteristic feature of prostate carcinoma, it is always associated with the rise in PSA. We are here by describing a case report of widespread multiple osteolytic lesions due to carcinoma prostate without rise in PSA and its review of the literature.
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108.
2. InamuraK. Prostatic cancers: Understanding their molecular pathology and the 2016 WHO classification.Oncotarget2018;9:14723-37.
3. ShahRB, MehraR, ChinnaiyanAM, ShenR, GhoshD, ZhouM, et al. Androgen-independent prostate cancer is a heterogeneous group of diseases: Lessons from a rapid autopsy program.Cancer Res2004;64:9209-16.
4. BormanP, OzoranK, AydoğS, CoşkunS. Osteopoikilosis: Report of a clinical case and review of the literature.Joint Bone Spine2002;69:230-3.
5. ClainA. Secondary malignant disease of bone.Br J Cancer1965;19:15-29.
6. SaitohH, HidaM, ShimboT, NakamuraK, YamagataJ, SatohT. Metastatic patterns of prostatic cancer. Correlation between sites and number of organs involved.Cancer1984;54:3078-84.
7. RoodmanGD. Mechanisms of bone metastasis.N Engl J Med2004;350:1655-64.
8. IdowuBM. Prostate carcinoma presenting with diffuse osteolytic metastases and supraclavicular lymphadenopathy mimicking multiple myeloma.Clin Case Rep2018;6:253-7.
9. Khot R, Sikarwar JS, Gupta RP, Sharma GL. Osteopoikilosis: A case report. Indian J Radiol Imaging 2005;15:453-4.
10. Daya K, Subhash C. Osteopoikilosis: A case report with review of literature. J Orthop Traumatol Rehabil 2013;6:84.
11. Küçükçakir N, Inceoğlu LA, Raif SL. Osteopoikilosis a case report. Turk J Phys Med Rehab 2015;61:375-9.
12. BhattarR, MaheshwariA, YadavSS, TomarV.Unusual presentation of prostate carcinoma: A case report.J Clin Diagn Res2017;11:PD06-7.
13. GartrellBA, ColemanR, EfstathiouE, FizaziK, LogothetisCJ, SmithMR, et al.Metastatic prostate cancer and the bone: Significance and therapeutic options.Eur Urol2015;68:850-8.
 |
 |
 |
 |
 |
| Dr. Shaligram Purohit | Dr. Shubhanshu Bhaladhare | Dr. Nandan Marathe | Dr. Swapneel Shah | Dr. Aditya Raj |
| How to Cite This Article: Purohit S, Bhaladhare S, Marathe N, Shah S, Raj A. Small Cell Prostate Cancer with Atypical Presentation – A Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2020 Mar-Apr;10(2): 50-53. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com