[box type=”bio”] Learning Point of the Article: [/box]
Desmoid fibromatosis should be included as differentials while evaluating lesions of the neck even in elderly males and a radiological diagnosis of neurocysticercosis in such lesions always warrants further evaluation with histopathology.
Case Report | Volume 10 | Issue 2 | JOCR March – April 2020 | Page 92-96| Praveen Ravi, S. Sundar Suriyakumar. DOI: 10.13107/jocr.2020.v10.i02.1714
Authors: Praveen Ravi[1], S. Sundar Suriyakumar[1]
[1]Department of Orthopedics, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. S Sundar Suriyakumar,
Assistant professor, Department of orthopedics, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai – 600116. India.
E-mail: drssundhar@gmail.com
Abstract
Introduction: Musculoskeletal fibromatoses represent a wide spectrum of fibroblastic and myofibroblastic neoplasms with similar pathologic appearances and variable clinical behavior. These lesions are categorized by location (superficial or deep). Deep fibromatosis in adults is divided into desmoid and abdominal wall type. Desmoid-type fibromatosis typically manifests as a deeply seated but poorly circumscribed soft-tissue mass. Slow insidious growth is common, and lesions are usually painless. It occurs most frequently in patients in the 2nd–4th decades of life, with a peak incidence between the ages of 25 and 35 years. Overall, the disease has a female predilection.
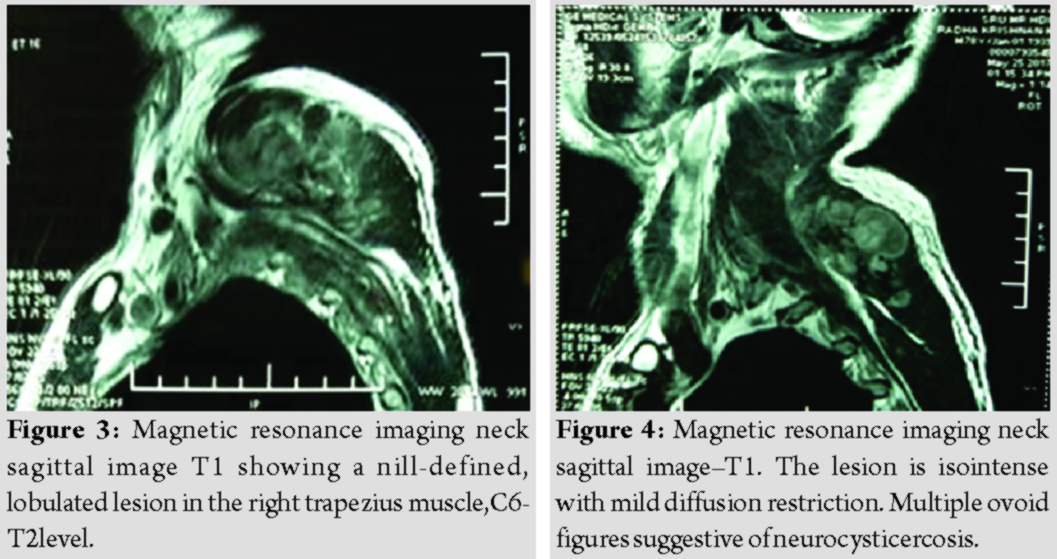
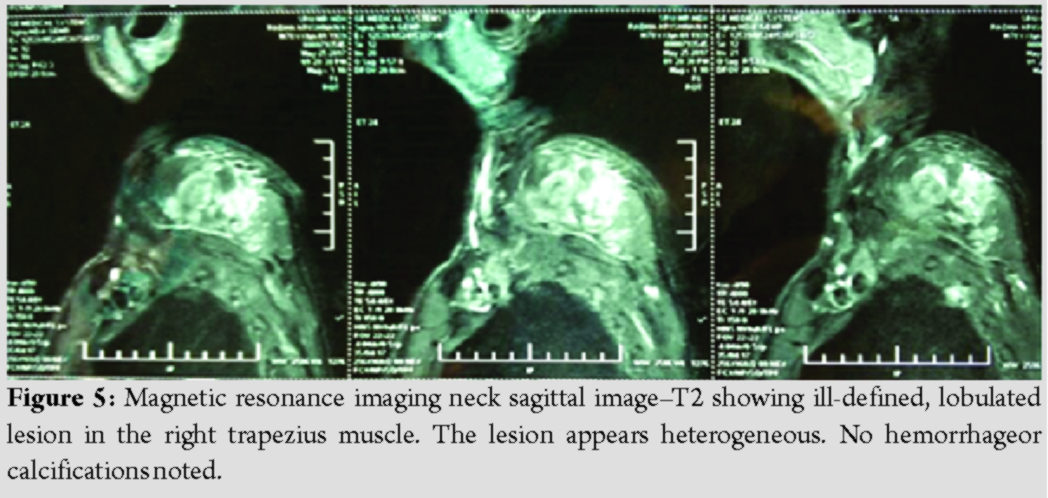
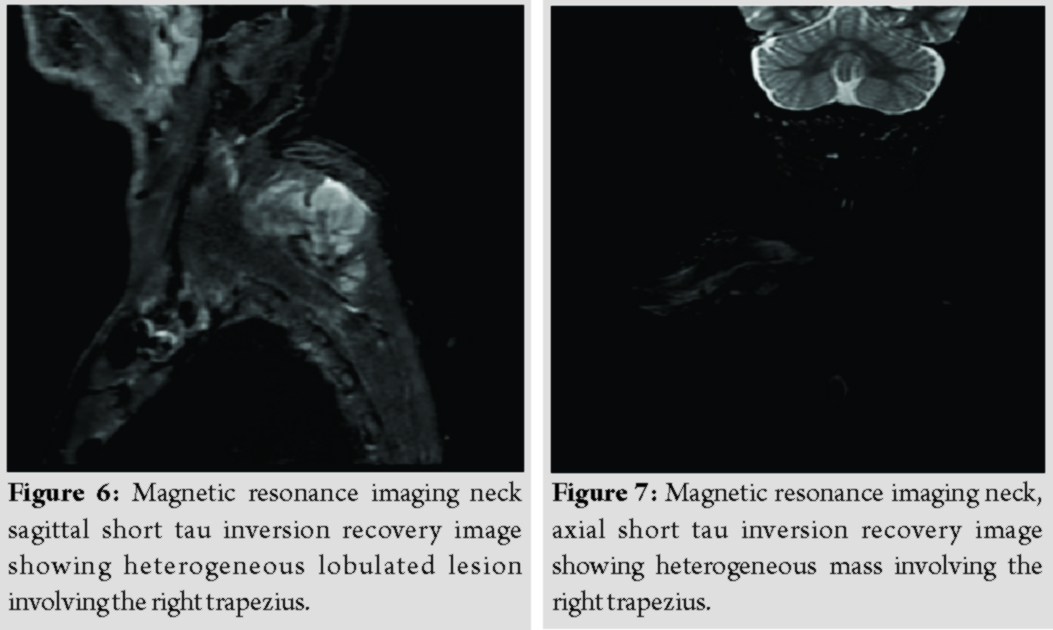
Case Report: Herein, we present the case of a 78-year-old man who developed a gradually progressive painless swelling over the right side of the neck over a period of 6 months. The patient was planned for a magnetic resonance imaging scan which showed ill-defined lobulated mass in the right trapezius of size 4 × 7 × 5.4 cm, which was heterogeneous in T2, isointense in T1, multiple ovoid calcifications, and was suspected with cysticercosis or fibroma. Open biopsy was done a week later which was suggestive of fibromatosis. The patient underwent definitive resection of the tumor 1 week later and the tumor was found to be restricted to the muscular plane. Histology was consistent with fibromatosis, the specimen being positive for vimentin, beta-catenin, and smooth muscle actin. The patient was on serial follow-ups and the last follow-up, 3 year later did not show any signs of recurrence of the tumor.
Conclusion: This case report is being presented to highlight the radiological differential of cysticercosis in a patient with muscular fibroma, extremely rare presentation of fibromatosis of the trapezius in the 7th decade.
Keywords: Trapezius fibromatosis, cysticercosis, elderly.
Introduction
Musculoskeletal fibromatoses represent a wide spectrum of fibroblastic and myofibroblastic neoplasms with similar pathologic appearances and variable clinical behavior. These lesions are categorized by location (superficial or deep). Deep fibromatosis in adults is divided into desmoid and abdominal wall type. Desmoid-type fibromatosis typically manifests as a deeply seated but poorly circumscribed soft-tissue mass. Slow insidious growth is common, and lesions are usually painless. It occurs most frequently in patients in the 2nd–4th decades of life, with a peak incidence between the ages of 25 and 35 years [1, 2]. Overall, the disease has a female predilection. The most commonly encountered locations of desmoid-type fibromatosis are shoulder or upper arm (28% of cases), chest wall or paraspinal region (17%), thigh (12%), neck (8%), knee (7%), pelvis or buttock (6%), lower leg (5%), forearm or hand (5%), and head (2%) [1, 2]. Shoulder and neck lesions are most frequent about the scapula, deltoid, axilla, and supraclavicular regions. Lesions affecting younger patients (<30 years old) and involving the head and neck have more aggressive behavior than those found in other sites and age groups. Such lesions have increased local recurrence rates [3]. There are no specific symptoms re¬lated to the tumor and it is mostly painless and shows swelling at the early stage. As the tumor progresses, variable symptoms such as pain, bowel obstruction, urinary obstruction, and limitation of range of joint movement develop depending on the location of the tumor [4]. In this case report, we present a rare case of a desmoidtumor developing in the trapezius in the elderly age group.
Case Report
A 78-year-old gentleman, who was a farmer by occupation, currently retired, hailing from Tamil Nadu, presented with a 6-month history of a swelling over the right side of the neck. The swelling was gradual in onset, progressive in its size over the course of 6 months. The patient also developed dull aching pain over the swelling for the past 2 months.There were no radiation of the pain, associated weakness of the extremities, or any sensory deficits. There was no history of trauma in the recent past or any other constitutional symptoms.The patient is not a diabetic. He is a K/c/o hypertension, COPD, and BPH for which he has been on treatment. On examination, there was a globular swelling of size 10 × 8 cm which was palpable over the right shoulder. The mass was seen extending superiorly, 8 cm below the mastoid tip to until the spine of scapula, mediolaterally from the midline, up to the medial border of scapula. On palpation, there was no local warmth or tenderness, globular swelling was felt which was firm in consistency with well-defined margins. The skin over the swelling was pinchable. The swelling was mobile in the coronal plane. There was no associated weakness or sensory deficits in the right upper limb. Movements of the shoulder were also unaffected.
Investigations
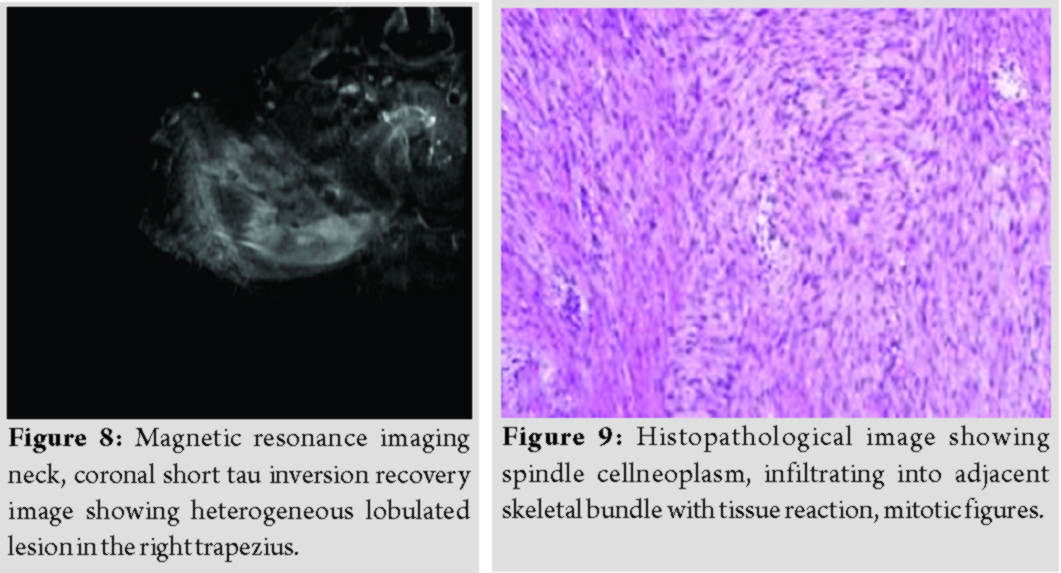
X-rays of the neck were suggestive of a soft-tissue mass in the inferior aspect of the neck with multiple ovoid calcifications (Fig. 1 and 2). 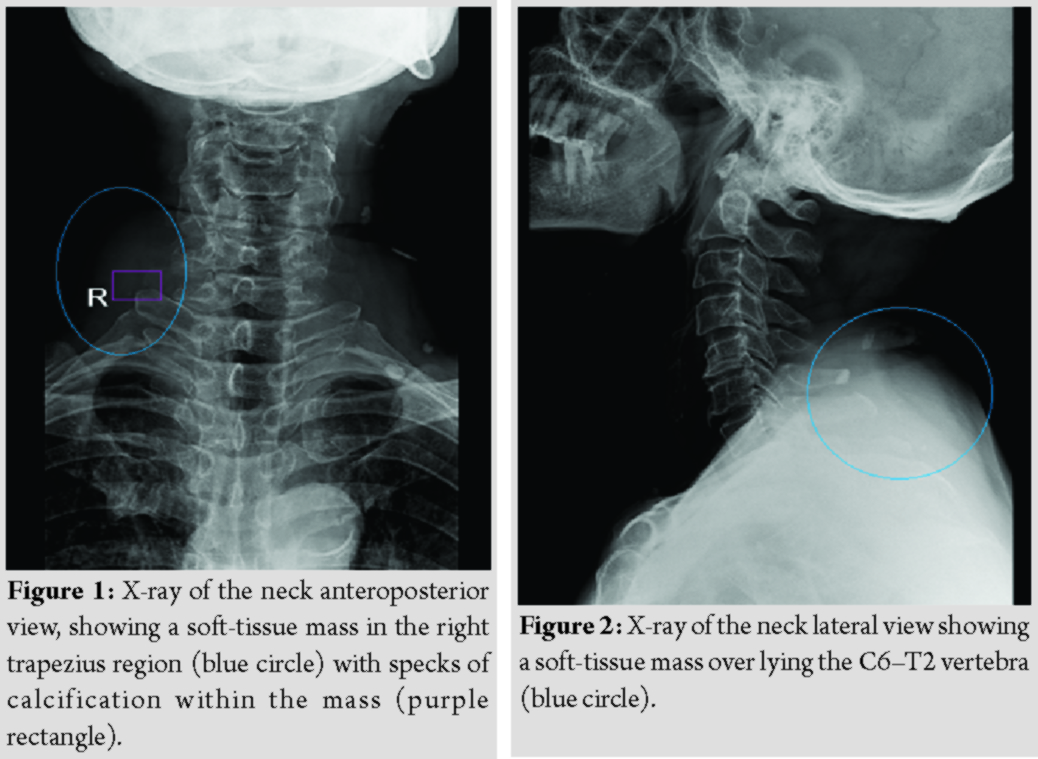
Differential diagnosis
Neurocysticercosis.
Fibromatosis.
Histopathology
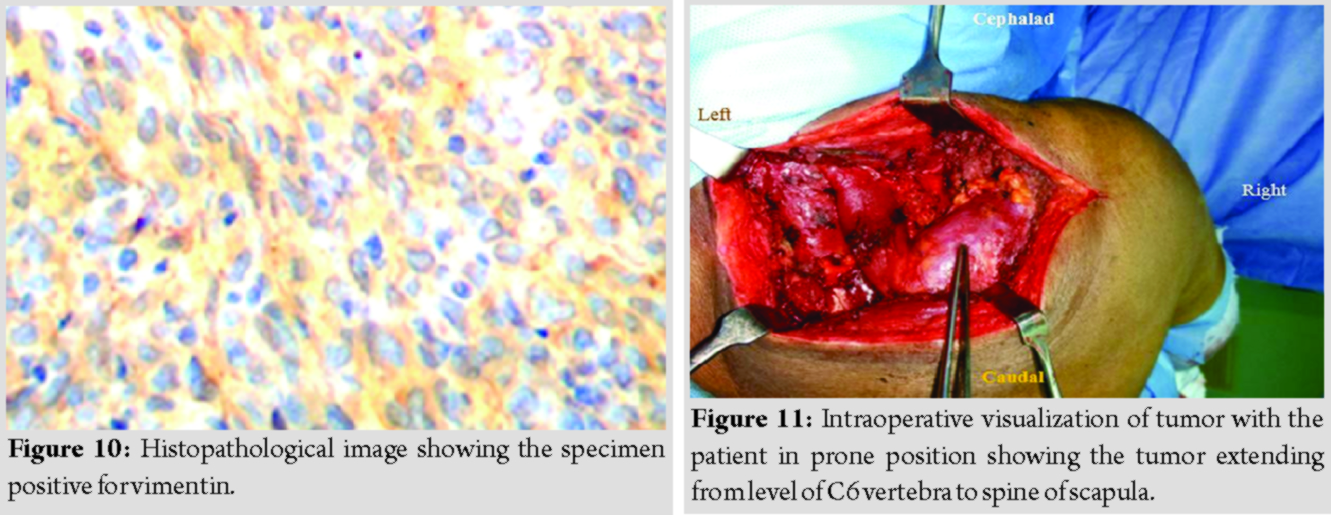
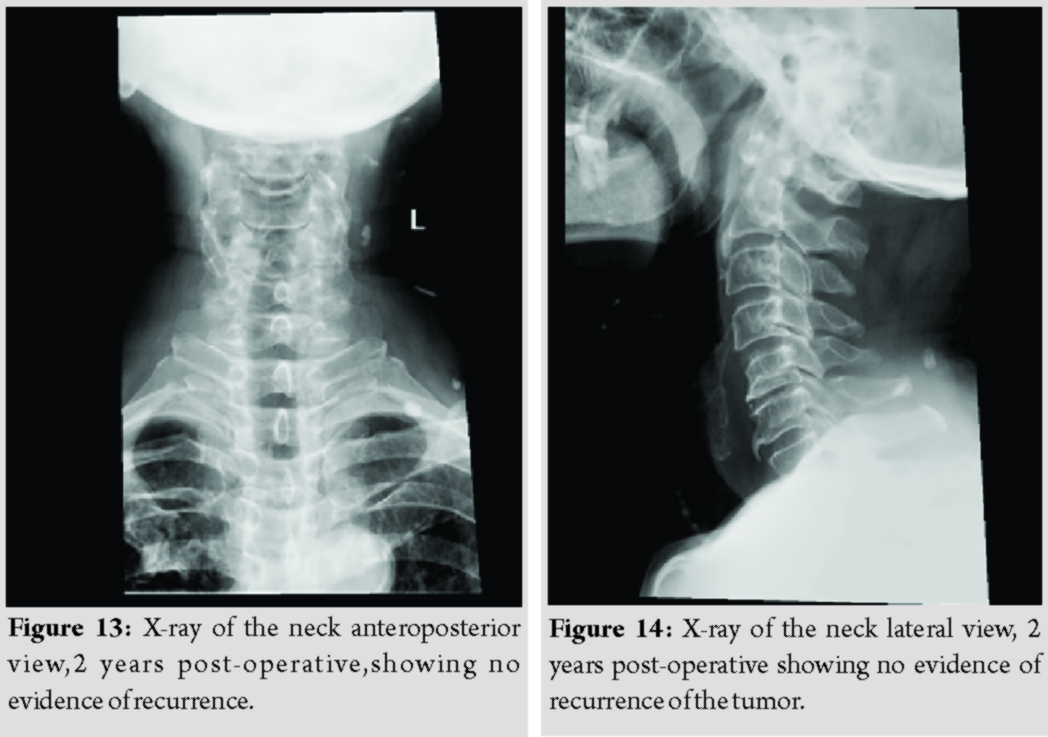
Open biopsy was done which showed benign spindle cell lesion infiltrating skeletal muscles, focal reactive skeletal bundle, with no necrosis, and no increase in mitosis. The tumor cells were positive for vimentin, focally positive for beta-catenin, and smooth muscle actin (SMA) (Fig. 9 and 10). The cells were negative for S100. Hence, the lesion was suggestive of fibromatosis.
Treatment
The patient was planned for wide local excision. A horizontal incision was made over the tumor and the overlying muscles were separated. The entire tumor was removed in toto (Fig. 11 and 12) which measured 9.0 x 8.5 x 6.0 cm. The cut surface showed an ill-defined gray-white lesion which was hard in consistency and the margins were reported to be free off the tumor.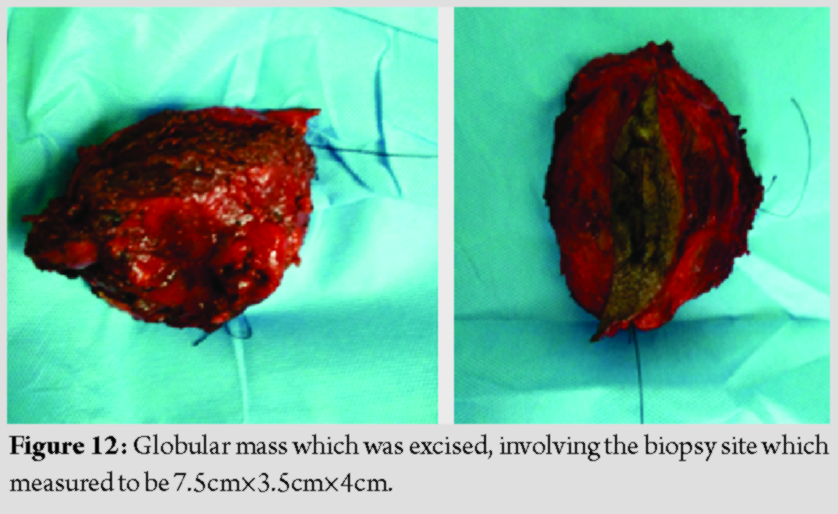
Discussion
A desmoid tumor was first described in 1832 by John MacFarlane as arising from the anterior abdominal wall and it is a rare disease, with a reported prevalence of 2–4 in 1,000,000/year [5]. The tumor may be located in the abdominal wall, extremities, and abdominal mesenteric. About 50% of the tumors are found in the abdominal wall and trunk muscle layers, 40% develop in the extremities, and 10% are located in the abdominal mesenteric. The most common locations apart from the abdomen are the shoulder and pelvis [5]. Our patient has a similar presentation with a lesion spanning over the right shoulder to the neck. Fibromatosis seen in the head-and-neck region is variants which tend to be locally aggressive, invading and eroding bone and soft tissue, thus compromising vital structures [6]. Incidences of trauma have been reported to precede the development of fibromatosis in 19–49% of cases. The postulated hypothesis for the same being abnormal response to healing with persistent immature fibroblast formation. Steroid sex hormones are also believed to play a role in the pathogenesis of the tumor [7]. There was, however, no preceding history of trauma or signs of erosion of the surrounding neurovascular structures in our patient, indicating a less aggressive form of the tumor. Diagnosis of the tumor is usually late since the clinical features are usually the result of pressure effects on surrounding structures. In cases involving the shoulder region, the most common clinical features, include tingling, numbness, paresthesia, and weakness of muscles of the hand “Shooting” pains radiating from shoulder to hand, have also been reported [8]. Since the lesion was well within the muscle bulk, no such symptoms or signs were elicitable in our case. Malignant transformation is quite rare. Metastasis has not been known to occur [9]. Imaging is of utmost importance in diagnosis. X-rays are usually inconclusive and may reveal calcifications if present, as seen in our case. Computed tomography scan reveals a soft-tissue mass of variable attenuation [10] but is not ideal. MRI is the optimal modality for evaluating the lesion. MRI showed a hypovascular multilobulated lesion of heterogeneous signal intensity with no hemorrhagic spots. However, neurocysticercosis as a differential cannot be ruled out after radiological evaluation. Biopsy is the only modality for definitive diagnosis. On gross examination, the lesion was hard to rubbery in consistency with light pink surface. On histological examination, the tumor was composed of uniform benign spindle-shaped cells infiltrating the skeletal muscles and poorly defined fascicles within a collagenous stroma, which were positive for vimentin, focally positive for beta-catenin, SMA, and negative for S100. There was moderate degree of cellularity. The lesions have prominent, mildly dilated, thick-walled intratumoral capillaries. Areas of myxoid degeneration and hemorrhage were seen. Nuclear pleomorphism is not usually seen, mitotic activity is low [1, 2, 3]. Low-grade fibrosarcoma, inflammatory pseudotumor, and scar hypertrophy should be considered as a differential diagnosis [11]. Complete surgical excision is considered the only effective treatment. However, there is a high chance of recurrence of head-and-neck fibromatosis (40–70%). Majority of recurrences occur within 18 months of excision [12]. There was no incidence of recurrence in our case at 24 months of follow-up. In case of recurrences, re-operation is mandatory, drug therapy or radiotherapy is further recommended if radical excision is not possible. Chemotherapy may have a significant role, considering the possible hormonal etiopathogenesis of the condition. One of the most commonly tried chemotherapeutic drugs is the antiestrogenic drug tamoxifen. Other drugs which have been tried include toremifene, progesterone, prednisolone, testosterone, and goserelin [13, 14]. Other NSAIDs such as indomethacin, sulindac, and colchicine have been tried with variable results [15, 16]. Our patient was started only on indomethacin (NSAIDs), 25 mg twice daily for a period of 1 month. In cases which fail to respond to treatment with antiestrogens, NSAIDs, cytotoxic drugs such as doxorubicin-dacarbazine combination, doxorubicin-cyclophosphamide-vincristine, or vincristine, actinomycin-D, and cyclophosphamide regimen may be used [17]. Recent advances advocate the use of interferon alpha and imatinib, monoclonal antibodies against tyrosine kinase c-kit receptors, platelet-derived growth factor receptor alpha [18]. Recurrences are reported to appear as late as 12 years after resection, hence annual follow-up mandatory lifelong.
Conclusion
Desmoid fibromatosis is predominately seen in younger individuals and has female preponderance. In this case report, we present an extremely rare case of a desmoid fibromatosis involving the trapezius of an elderly male patient. This case report also highlights the tumor radiologically mimicking neurocysticercosis of the trapezius.
Clinical Message
Desmoid fibromatosis should be included in the differentials while evaluating swellings and lesions of the neck even in elderly males. A radiological diagnosis of neurocysticercosis of the neck always warrants a histopathological examination. The tumor is benign and slow growing, proper surgical excision with chemotherapy in the form of NSAIDs seems to be adequate. However, patients are to be counseled regarding the importance of periodic follow-up, given the high rate of recurrences at later periods.
References
1. Fletcher CD, Unni KK, Mertens F. Pathology and genetics of tumours of soft tissue and bone. Geneva, Switzerland: World Health Organization; 2002. p. 978-92.
2. Kransdorf MJ, Murphey MD. Benign fibrous and fibrohistiocytic tumors. In: Imaging of Soft Tissue Tumors. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. p. 189-256.
3. Weiss SW, editors. Soft Tissue Tumors. St Louis, Mo: Mosby Elsevier; 2008. p. 431-44.
4. Shields CJ, Winter DC, Kirwan WO, Redmond HP. Desmoid tumours. Eur J Surg Oncol 2001;27:701-6.
5. Reitamo JJ, Häyry P, Nykyri E, Saxén E. The desmoid tumor. I. Incidence, sex-, age- and anatomical distribution in the Finnish population. Am J Clin Pathol 1982;77:665-73.
6. Prabhu R, Natarajan A, Shenoy R. Aggressive fibromatosis (desmoid tumour) of the head and neck: A benign neoplasm with high recurrence. BMJ Case Rep 2013;2013:bcr2013200156.
7. Goullner JR, Soule EH. Desmoid tumors. An ultrastructural study of eight cases. Hum Pathol 1980;11:43-50.
8. Enzinger FM, Shiraki M. Musculoaponeurotic fibromatosis of the shoulder girdle. Cancer 1967;20:1131.
9. Soule EH, Scanlon PW. Fibrosarcoma arising in an extraabdominal desmoid tumor: Report of case. Mayo Clin Proc 1962;37:443.
10. Murphey MA, Ruble CM. Musculoskeletal fibromatoses: Radiologic-pathologic correlation. RadioGraph 2009;29:2143-76.
11. Schwickerath J, Künzig HJ. Spontaneous malignant transformation of extra-abdominal fibromatosis to fibrosarcoma. Geburtshilfe Frauenheilkd 1995;55:173-5.
12. Kruse AL, Luebbers HT, Grätz KW, Obwegeser JA. Aggressive fibromatosis of the head and neck: A new classification based on a literature review over 40 years (1968-2008). Oral Maxillofac Surg 2010;14:227-32.
13. Kinzbrunner B, Ritter S, Domingo J, Rosenthal CJ. Remission of rapidly growing desmoid tumors after tamoxifen therapy. Cancer 1983;52:2201-4.
14. Mukherjee A, Malcolm A, De la Hunt M, Neal DE. Pelvic fibromatosis (desmoid) treatment with steroids and tamoxifen. Br J Urol 1995;75:559-60.
15. Lackner H, Urban C, Kerbl R, Schwinger W, Beham A. Noncytotoxic drug therapy in children with unresectable desmoid tumors. Cancer 1997;80:334-40.
16. Waddell WR, Gerner RE. Indomethacin and ascorbate inhibit desmoid tumors. J Surg Oncol 1980;15:85-90.
17. Weiss AJ, Lackman RD. Low-dose chemotherapy of desmoid tumors. Cancer 1989;64:1192-4.
18. Heinrich MC, McArthur GA, Demetri MD, Joensuu H, Bono P, Herrmann R, et al. Clinical and molecular studies of the effect of imatinib on advanced aggressive fibromatosis (desmoid tumor). J Clin Oncol 2006;24:1195-203.
 |
 |
| Dr. Praveen Ravi | Dr. S. Sundar Suriyakumar |
| How to Cite This Article: Ravi P, Suriyakumar SS. Case report: Trapezius Fibromatosis in the Elderly – An Extremely Rare Tumor. Journal of Orthopaedic Case Reports 2020 Mar-Apr;10(2): 92-96. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com