[box type=”bio”] Learning Point of the Article: [/box]
Large femoral cystic swellings after ACL reconstruction surgery are rare and must be evaluated carefully: Surgical intervention may be required, particularly if there is suspicion of an infection.
Case Report | Volume 10 | Issue 4 | JOCR July 2020 | Page 20-24 | Christian Heng Hwee Yee, Andrew Tan Hwee Chye. DOI: 10.13107/jocr.2020.v10.i04.1784
Authors: Christian Heng Hwee Yee[1], Andrew Tan Hwee Chye[1]
[1]Department of Orthopedic Surgery, Singapore General Hospital, Academia Level 4, 20 College Rd, Singapore.
Address of Correspondence:
Dr. Christian Heng Hwee Yee,
Department of Orthopedic Surgery, Singapore General Hospital, Academia Level 4, 20 College Rd, Singapore.
E-mail: christian.heng@mohh.com.sg
Abstract
Introduction: Large cystic swellings in the knee are a rare complication of anterior cruciate ligament (ACL) reconstruction surgery. Most cystic swellings in the literature arise from the tibia; femoral cystic swellings which are clinically significant and infected are thus extremely rare. Little is known about the etiology of such cystic swellings post-ACL reconstruction, and there are no standardized protocols for their treatment.
Case Presentation: Our patient presented 6 months post-ACL reconstruction, with a large swelling over the lateral aspect of the femur in the operated knee. His presentation presented a clinical dilemma: On the one hand, he presented with a large cystic swelling adjacent to the knee, but had only vague knee pain with no significant joint effusion and no fever or other constitutional symptoms; while on the other, his swelling was significantly large and his imaging findings were worrisome. This cystic swelling turned out to be an infected cyst arising from the tissue adjacent to the femoral tunnel. We present a rare complication of ACL reconstruction and discuss the possible causes of such large cystic swellings. We also discuss the management of large infected cysts post-ACL reconstruction.
Conclusion: Large, infected femoral cyst post-ACL reconstruction is rare and requires appropriate clinical assessment and management. It is important to ascertain whether they are associated with intra-articular infections/septic arthritis. If there is no septic arthritis, these swellings can be treated with simple surgical debridement and antibiotics and retention of ACL graft. The long-term outcomes of graft retention in these patients are excellent.
Keywords: Femoral cyst, anterior cruciate ligament, reconstruction, reconstruction, infection, graft retention.
Introduction
Anterior cruciate ligament (ACL) reconstruction surgery is a commonly performed orthopedic procedure [1]. Commonly seen complications after ACL reconstruction include arthrofibrosis, graft stretching, and graft failure [2]. Large cystic swellings of the knee after ACL reconstruction are uncommon, especially over the femur. Furthermore, infections of these cysts are rarely reported occurrences [3]. Surgical site infections are rare after ACL reconstruction, with most reports citing an incidence of around 1–2% [4]. We report the first case of a large infected femoral cyst in the knee after ACL reconstruction with the transportal technique.
Case Report
Our patient was a 33-year-old man who had injured his left ACL while playing basketball. A month later, he underwent ACL reconstruction surgery at another hospital. He saw us 6 months after his index surgery with the complaint of a left lateral knee swelling.
Operation notes were traced from the hospital where the ACL surgery was done. He underwent a left knee arthroscopic ACL reconstruction with a quadrupled left hamstring (semitendinosus and gracilis) autograft. The transportal technique was used to drill the femoral tunnel. The femoral tunnel measured 7.5 × 25 mm and the femoral graft was secured with an Endobutton (Smith and Nephew, Andover, MA, USA). The tibial tunnel measured 7.5 × 30 mm and the tibial graft was secured with an 8 × 30 mm Biosure interference screw (Smith and Nephew, Andover, MA, USA) and supplemented with a single staple. During the operation, he was noted to have a lateral meniscal tear, which was repaired with a single Fastfix suture (Smith and Nephew, Andover, MA, USA).
At the time of presentation to us, he complained of vague left knee pain. The pain was worse at night and affected his sleep. He denied any reinjury to his knee after the index surgery. He did not have any fever or other constitutional symptoms. On examination, there was a vague, tender swelling at the superolateral aspect of his left knee, which was spherical in shape and measured approximately 3 cm in diameter. The swelling was a firm lump which was not pulsatile or compressible and was noted to be transilluminable. He had no joint effusion and the ACL graft was stable on physical examination. Blood investigations showed only mildly raised inflammatory markers (erythrocyte sedimentation rate [ESR] 22 mm/h [normal 0–15 mm/h], C-reactive protein [CRP] 15.9 mg/L [normal <3.0 mg/L], and total white counts 8.85 × 109/L [normal 4–11 × 109/L]).
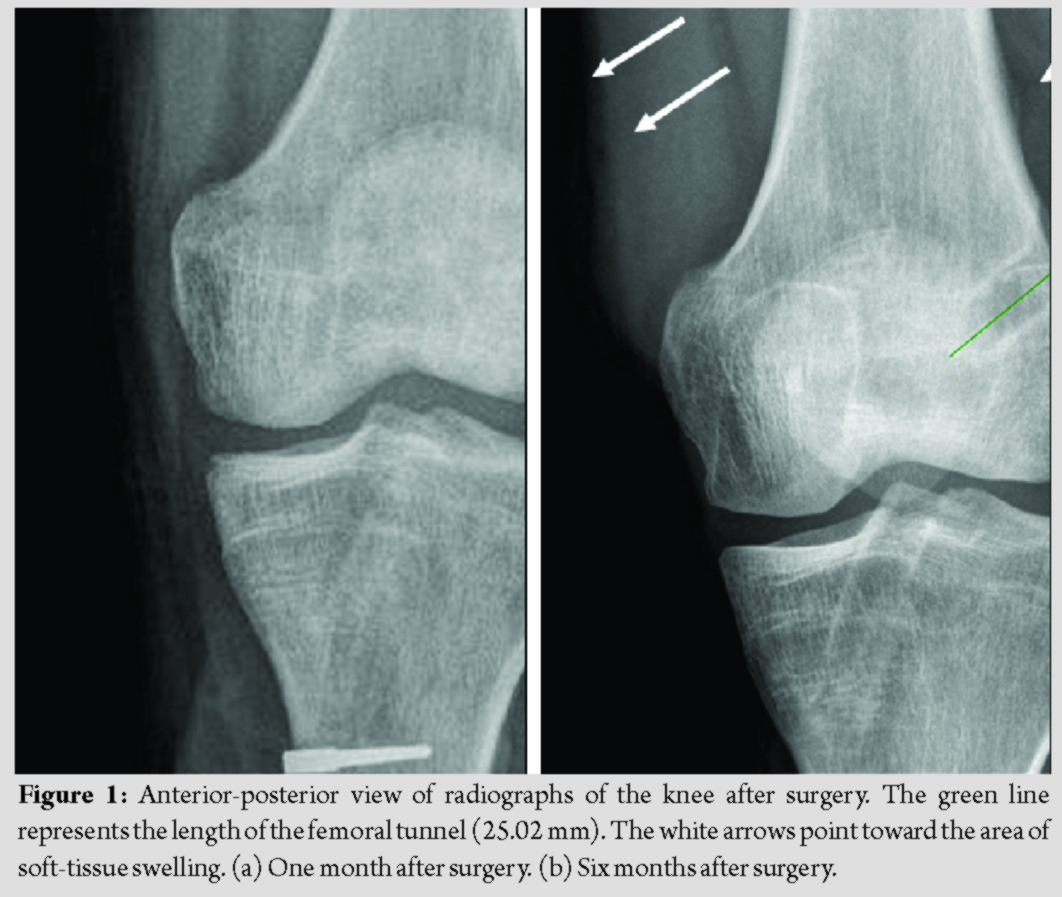
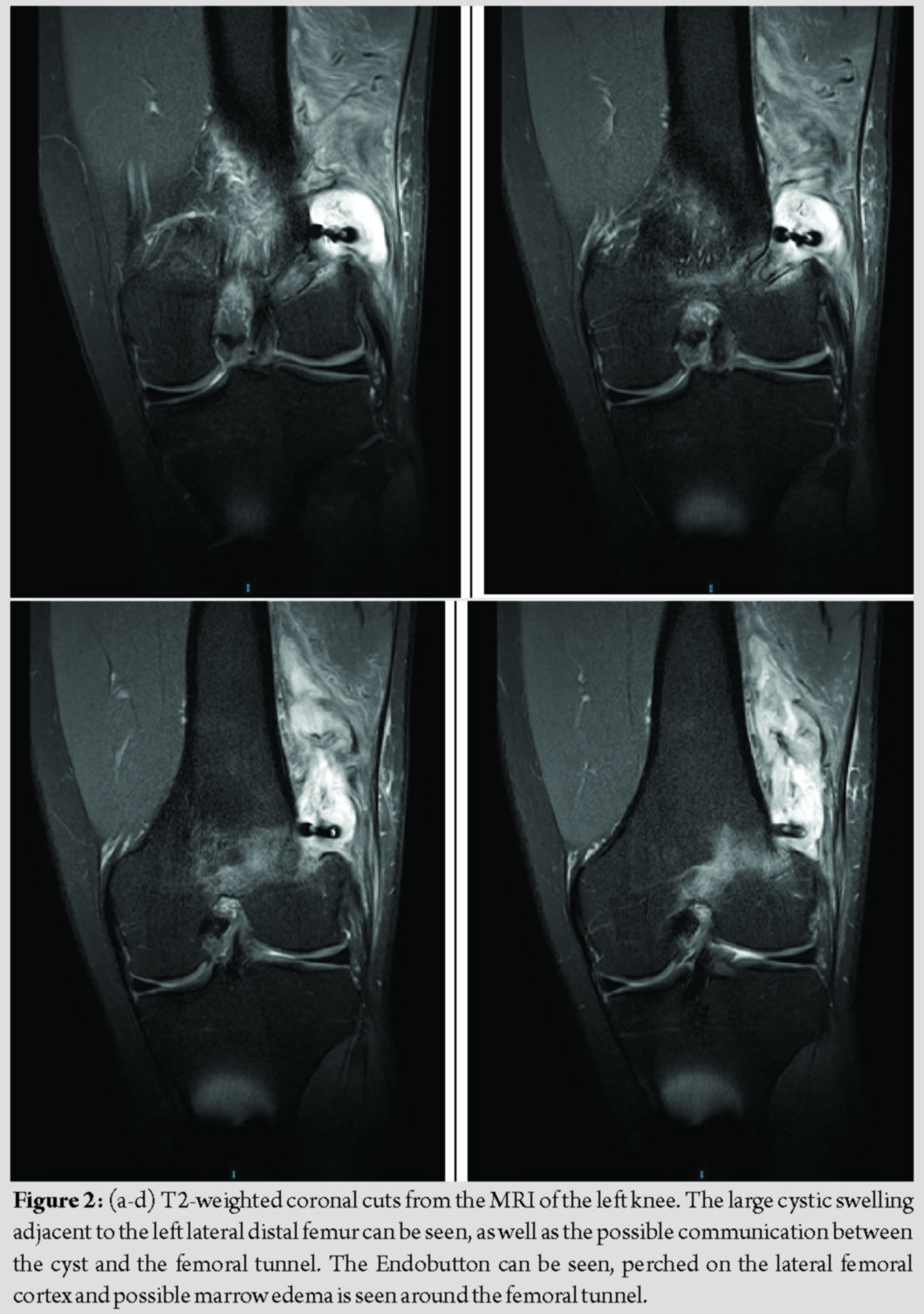
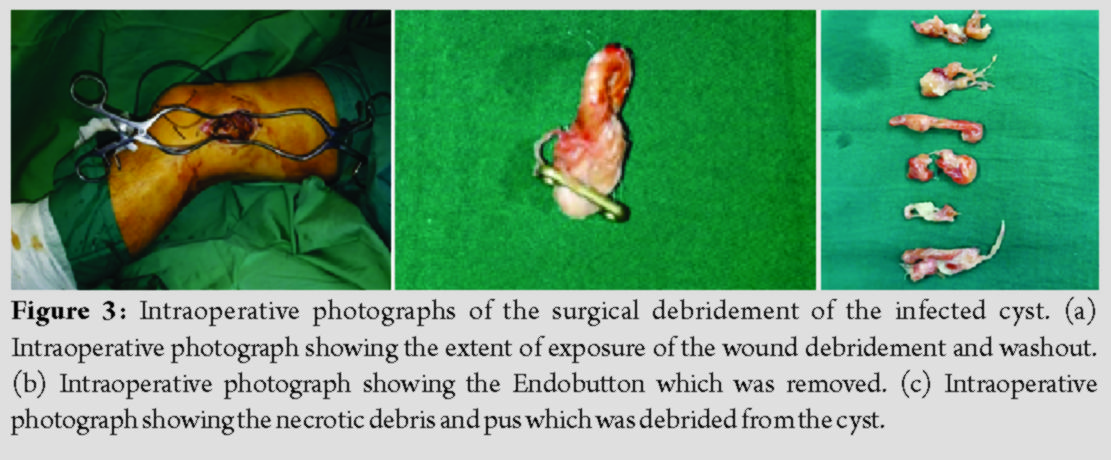
Radiographs of the left knee showed cortical erosion of the femur at the Endobutton site and soft-tissue swelling around the lateral aspect of the distal femur (Fig. 1); MRI of the left knee (with contrast) was subsequently performed, which showed a thick rim-enhancing collection posterolateral to the knee joint, measuring 6.5 × 5.1 × 1.5 cm (Fig. 2). There was a heterogeneous appearance of the ACL graft fibers, worrisome for a partial tear of the graft. The decision was made for conservative management to await resolution of the swelling. This decision was made for two main reasons: First, while the swelling was large and significant, the patient himself was not septic/febrile, there were no signs or symptoms of septic arthritis and the inflammatory markers were only borderline raised; second, the patient himself was counseled on the risks of surgery and the consequences of conservative management, and he declined surgery at the time. When he was seen 9 months later during a follow-up visit, he was still experiencing pain from the left knee and the swelling had persisted. Blood tests remained unremarkable, but a repeat MRI showed persistence of the collection. In view of the persistence of the symptoms, we elected for exploration of his cystic swelling under anesthesia. Intraoperatively, we noted a 4 × 4 cm left lateral distal femoral cyst containing pus and necrotic material with underlying unhealthy synovial tissue (Fig. 3). Tissues were sent for histology and cultures. The femoral Endobutton was also noted to have migrated and was removed. On exploration of the femoral tunnel, there was no pus expressed from the bone and no obvious osteomyelitic changes in the femur. The lateral distal femur and surrounding soft tissue were washed with copious amounts of hydrogen peroxide, diluted iodine, chlorhexidine, and normal saline. Histology of the cyst showed “fibrocollagenous tissue with a heavy infiltrate of neutrophils, lymphocytes, and plasma cells with an area of necrosis.” Cultures grew methicillin-sensitive Staphylococcus aureus sensitive to clindamycin. The patient was treated with oral clindamycin postoperatively for 6 weeks. At 2-year follow-up, he had no further pain in his left knee and had returned to sports, with no symptoms of instability in his left knee. On examination, the wound had healed, no knee swelling was noted, and the knee showed no clinical evidence of infection. Anterior drawer test showed Grade 1 laxity with an end-point, and Lachman’s test was negative.
Discussion
Large femoral cystic swellings after ACL reconstruction are rarely reported. The management of such infected cysts represents both a diagnostic and a management dilemma. The diagnostic difficulties include the cause and nature of the cystic swelling, and whether it has an intra-articular communication. The contentious issue in management lies in whether to preserve or remove the ACL graft in the treatment of the knee infection. A large cystic swelling adjacent to the femur presents a diagnostic difficulty as it is rare and ascertaining the actual etiology of the cyst may be elusive. There is a lack of literature with regard to femoral cystic swellings that occur after ACL surgery. The majority of reported cystic swellings arise from the tibial side as opposed to the femoral [5]. Tibial cysts can be divided into two groups, depending on whether they communicate with the knee joint [3]. Most tibial cysts are thought to arise as a result of degradation of the biodegradable interference screws used to secure the tibial end of the graft [6]. There was one reported case of cystic swelling because of an oversized tibial tunnel, but this occurred after a posterior cruciate ligament reconstruction [7]. There was just one case of femoral synovial cyst after ACL reconstruction; the authors postulated that the synovial cyst formed due to a fistula associated with the use of a non-absorbable silk suture for traction on the femoral bone plug [8]. There are very few reports on the etiology of femoral cysts, but we can extrapolate from the literature on tibial cysts that the presence of biodegradable material, non-absorbable sutures resulting in fistula formation or oversizing of the femoral tunnel could be possible causes. We postulate that in this case, the cyst arose because of an excessively short femoral tunnel. It is known that the transportal technique is associated with femoral tunnel complications of short tunnel length and cortical bone blowout [9]. On this patient’s early (1 month post-operative) follow-up radiographs, the femoral cortex looks excessively wide compared to the size of the Endobutton. This cortical defect seems to have progressed slightly in the subsequent months (Fig. 1). On the anterior-posterior view of the left knee radiographs, a soft-tissue swelling at the lateral distal femur can be appreciated. The femoral tunnel was reamed through a transportal, all-inside technique; thus, the femoral cystic collection could have been due to fluid extravasation from the knee joint. This represents a communicating cyst due to breaching of the lateral femoral cortex by the femoral reaming. In the surgical notes of the index operation, it was documented that the femoral tunnel was drilled to 25 mm. On radiographs, the lateral femoral condyle from notch (femoral footprint) to the cortex measured approximately 25 mm as well. This excessively short femoral tunnel could have caused the large cortical exit hole. This exit hole was not adequately plugged by the graft, thus fluid from the joint was able to escape into the peri-femoral space. Furthermore, this large cortical defect caused the Endobutton to be “perched” on the lateral femur, with potential compromise to the stability of the femoral fixation. The second diagnostic dilemma was whether this cystic collection represented an infection/abscess. Surgical site infections after ACL reconstruction are rare, and current literature suggests an incidence of <2%. SSIs can be divided into superficial or deep infections. Superficial infections can be managed with conservative treatment and antibiotics, but deep infections may require surgical treatment. In this patient, there was a discrepancy in the clinical findings, radiological findings, and actual intraoperative findings of the size of the cystic swelling. A possible reason for the discrepancy between the size of the cyst on clinical examination as compared to the actual lump excised at surgery was that it was a deep cystic swelling; hence, its actual size may have been difficult to estimate on clinical examination. A possible reason for the discrepancy between the size on MRI and the actual size of the excised cyst at surgery was that the excision was performed 9 months after the MRI; hence, there may have been interval resorption of the contents of the cyst. This was an atypical presentation of a peri-articular infection. The initial clinical picture was equivocal for infection. He had vague knee pain which persisted for 6 months after surgery, but there were no other accompanying signs or symptoms. His biochemical and radiographical investigations were also inconclusive. However, given the persistence of his symptoms for 9 months, we decided for surgery. The source of the infection in our patient was unclear. The abscess was found on the femoral fixation site, which had minimal exposure to direct contamination. The femoral graft and Endobutton was inserted through an all-inside approach, and the overlying skin on the femur was hardly breached, except for a small exit puncture wound used to pull the graft up the femoral tunnel. The persistent cystic swelling at the femoral exit site was substantial in size and it could have served as a nidus for infection. Studies have shown that the incidence of infection varies between the different choices of grafts, with hamstring autografts having a higher rate of infection than bone-patellar tendon-bone autografts [10]. Previous knee surgery and concomitant surgical procedures performed at the time of ACL reconstruction are known risk factors for post-operative infection [11]. This patient had reconstruction with hamstring autograft as well as a concomitant meniscal repair performed, thus possibly increasing his risk of post-operative infection. An important question to answer in considering the management options is whether this infection was intra-articular. Septic arthritis after ACL reconstruction typically presents in the acute or subacute phase (<2 months after surgery); late presentation (more than 2 months after surgery) is rare. Patients usually have joint effusion, severe pain, and limited range of motion, which is associated with fever and overlying skin erythema [11]. Blood investigations are deranged, with raised ESR and CRP suggestive of a more serious infection [12]. Some authors recommend joint aspiration as a gold standard for the diagnosis of septic arthritis, with synovial cell counts, Gram stain, and synovial fluid cultures as reliable guides to the confirmation of this diagnosis [13]. There exists controversy in the literature with regard to the management of the ACL graft in septic arthritis post-ACL reconstruction. Proponents for graft preservation recommend a treatment protocol which includes long-term antibiotics, arthroscopic irrigation, and debridement [14]. They suggest that this protocol may achieve success in eradicating infection in up to 85% of cases [15]. On the other hand, proponents for graft removal feel that the graft remains a source of infection in the joint and its preservation might lead to failure or delay of eradication of the infection [4, 11, 13, 15]. We felt that this patient’s infection did not constitute septic arthritis; hence, we did not perform joint aspiration or a diagnostic arthroscopy. We only excised the extra-articular cyst and debrided the surrounding unhealthy tissue. Since clinically, there were no signs of septic arthritis, we felt that there was no need to violate the joint, as it risks seeding the infection. Intraoperatively, we did not notice any osteomyelitic changes in the bone, and there was no communication between the cystic swelling and the joint. As the infection was extra-articular, and the patient had no signs or symptoms of septic arthritis or clinical instability about the knee, we decided to preserve the graft.
Conclusion
Large, infected femoral cyst post-ACL reconstruction is rare and requires appropriate clinical assessment and management. It is important to ascertain whether they are associated with intra-articular infections/septic arthritis. If there is no septic arthritis, these swellings can be treated with simple surgical debridement and antibiotics and retention of ACL graft. The long-term outcomes of graft retention in these patients are excellent.
Clinical Message
Large femoral cysts arising from the femur are rare complications of ACL reconstruction. There are few reports in the literature as to their etiology or management. Our patient had a delayed presentation of a large femoral cyst, which exhibited signs of a localized infection and did not seem to be an intra-articular septic arthritis. We were able to manage him with only simple surgical debridement as well as antibiotics, without needing to perform an arthrotomy or ACL graft debridement/revision. He had excellent results from the treatment and was able to return to sports with no functional deficits.
References
1. Garrett WE Jr., Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ, et al. American board of orthopaedic surgery practice of the orthopaedic surgeon: Part-II, certification examination case mix. J Bone Joint Surg 2006;88:660.
2. Meyers AB, Haims AH, Menn K, Moukaddam H. Imaging of anterior cruciate ligament repair and its complications. Am J Roentgenol 2010;194:476-84.
3. Ghazikhanian V, Beltran J, Nikac V, Feldman M, Bencardino JT. Tibial tunnel and pretibial cysts following ACL graft reconstruction: MR imaging diagnosis. Skeletal Radiol 2012;41:1375-9.
4. Hantes ME, Raoulis VA, Doxariotis N, Drakos A, Karachalios T, Malizos KN. Management of septic arthritis after arthroscopic anterior cruciate ligament reconstruction using a standard surgical protocol. Knee 2017;24:588-93.
5. Faunø P, Christiansen SE, Lund B, Lind M. Cyst formation 4 years after ACL reconstruction caused by biogradable femoral transfixation: A case report. Knee Surg Sport Traumatol Arthrosc 2010;18:1573-5.
6. Deie M, Sumen Y, Ochi M, Murakami Y, Fujimoto E, Ikuta Y. Pretibial cyst formation after anterior cruciate ligament reconstruction using auto hamstring grafts: Two case reports in a prospective study of 89 cases. Magn Reson Imaging 2000;18:973-7.
7. Ahn JH, Lee YS, Chang MJ. Post-tibial cyst formation over 2 years after posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2008;16:996-8.
8. Feldmann DD, Fanelli GC. Development of a synovial cyst following anterior cruciate ligament reconstruction. Arthroscopy 2001;17:200-2.
9. Kim JG, Wang JH, Lim HC, Ahn JH. Femoral graft bending angle and femoral tunnel geometry of transportal and outside-in techniques in anterior cruciate ligament reconstruction: An in vivo 3-dimensional computed tomography analysis. Arthroscopy 2012;28:1682-94.
10. Barker JU, Drakos MC, Maak TG, Warren RF, Williams RJ, Allen AA. Effect of graft selection on the incidence of postoperative infection in anterior cruciate ligament reconstruction. Am J Sports Med 2010;38:281-6.
11. Cadet ER, Makhni EC, Mehran N, Schulz BM. Management of septic arthritis following anterior cruciate ligament reconstruction: A review of current practices and recommendations. J Am Acad Orthop Surg 2013;21:647-56.
12. Wang C, Ao Y, Fan X, Wang J, Cui G, Hu Y, et al. C-reactive protein and erythrocyte sedimentation rate changes after arthroscopic anterior cruciate ligament reconstruction: Guideline to diagnose and monitor postoperative infection. Arthrosc J Arthrosc Relat Surg 2014;30:1110-5.
13. Mouzopoulos G, Fotopoulos VC, Tzurbakis M. Septic knee arthritis following ACL reconstruction: A systematic review. Knee Surg Sport Traumatol Arthrosc 2009;17:1033-42.
14. Schuster P, Schulz M, Immendoerfer M, Mayer P, Schlumberger M, Richter J. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: Evaluation of an arthroscopic graft-retaining treatment protocol. Am J Sports Med 2015;43:3005-12.
15. Saper M, Stephenson K, Heisey M. Arthroscopic irrigation and debridement in the treatment of septic arthritis after anterior cruciate ligament reconstruction. Arthroscopy 2014;30:747-54.
 |
 |
| Dr. Christian Heng Hwee Yee | Dr. Andrew Tan Hwee Chye |
| How to Cite This Article: Heng CH, Tan AH. Large Infected Femoral Cystic Swelling after Anterior Cruciate Ligament Reconstruction through Transportal Technique. Journal of Orthopaedic Case Reports 2020 July;10(4): 20-24. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com