[box type=”bio”] Learning Point of the Article: [/box]
This is a case report that demonstrates clinical, radiological and histological features of ribbing disease and that it can be treated by intramedullary reaming with good symptomatic relief postoperatively.
Case Report | Volume 10 | Issue 4 | JOCR July 2020 | Page 69-73 | M Lokesh, Sundar Suriyakumar. DOI: 10.13107/jocr.2020.v10.i04.1808
Authors: M Lokesh[1], Sundar Suriyakumar[1]
[1]Department of Orthopedic Surgery, Sri Ramachandra Medical College and Research Institute, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. Sundar Suriyakumar,
Department of Orthopaedic Surgery, Sri Ramachandra Medical College and Research Institute, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai – 600 116, Tamil Nadu, India.
E-mail: drssundhar @gmail.com
Abstract
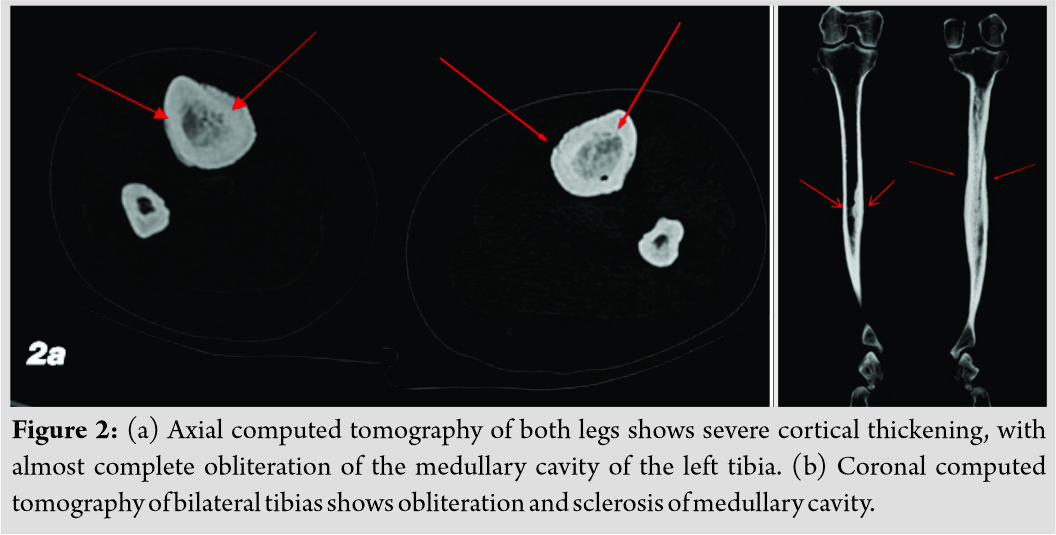
Introduction: Ribbing diseases is rare and have only been occasionally reported. We here in report a case of Ribbing disease affecting bilateral tibia which was diagnosed based on computed tomography (CT), magnetic resonance imaging (MRI), and histopathological features and managed by intramedullary reaming .
Case Report: A 45 – year – old female presented with complaints of pain in the right leg for the past four 4 months duration and the patient had similar complaints of pain in the left leg 3 years back for which she had had taken treatment at an outside hospital where she underwent saucerization of the left tibia as a case of low- grade osteomyelitis . To evaluate the cause of pain X-ray, CT and, MRI were done which were suggestive of Ribbings disease and biopsy was performed which favoured the diagnosis of Ribbings disease. The patient was tried on a course of analgesics , with no symptomatic betterment , after going through the literature, the patient was taken up for the right tibia intramedullary reaming. Post operatively, the patient symptomatically improved and is pain free for the past 4 years.
Conclusion: Ribbing disease is an uncommon cause of a common symptom. It is a rare diaphyseal sclerosing dysplasia. With lack of clinical signs of infection and biochemical evidence of metabolic bone disease and positive clinical, radiological and histological features in favour of ribbing disease helped us in arriving at the diagnosis. Intramedullary reaming of the affected bone has been useful in providing symptomatic betterment .
Keywords: Diaphysis of tibia, intramedullary reaming, Ribbing disease.
Introduction
Ribbing disease is a rare disease that is not often clinically encountered in our day- to- day practice. Ribbing described a family with six siblings for the first time in 1949 in which four of them had asymmetrical diaphyseal sclerosis of long bones. He designated the term hereditary multiple diaphyseal sclerosis; later, it was named after him as Ribbing disease. Ribbing disease is a form of sclerosing dysplasia characterized by benign endosteal and periosteal osseous growth confined to the diaphysis of the long bones sparing the epiphysis, usually the long bones of lower limb, i.e., tibia and femur. The exact etiology is not known yet, some researchers think that Ribbing disease is caused by genetic changes (pathogenic variants or mutations) in the TGFB1 gene, and that the disease is inherited in an autosomal recessive manner. The prevalence of Ribbing disease is unknown. Only a very few cases of Ribbing disease have been reported in medical literature. According to Seegar et al. (1996), only 13 cases of Ribbing disease had been previously described in the English literature. Some authors estimate that in the whole literature, only 20-30 cases have been reported, according to a systematic review of Ribbing disease published by Pijls et al. (2017), literature search yielded 420 unique hits of which 23 studies, covering a total of 40 patients, were only considered to have Ribbing disease by the reviewers [1]. The disease usually manifests in 4th and 5th decade of life. The patients end up with frequent hospital visits due to progressive pain. The patient usually presents with intolerable pain which is the most important symptom of this disease that does not resolve with medical treatment, clinical examination is usually unremarkable with normal blood parameters. The conventional radiology shows cortical thickening of the diaphyseal portion of long bones, sometimes associated with the narrowing of the medullary canal, while the epiphyses are spared. The magnetic resonance imaging (MRI) examination confirms the presence of sclerosis and reveals usually bone marrow edema in the diaphyses of the affected bones. It is often initially diagnosed as low-grade osteomyelitis, but it may also be confused with other causes of increased bone density on radiological investigations (sclerosing dysplasia) such as Camurati-Engelmann disease, Van Buchem disease and Erdheim–Chester disease, etc. Diagnosis of the disease is aided by clinical, radiological, and pathological workup. Treatment options for Ribbing disease may include medications such as non-steroidal anti-inflammatory drugs (NSAIDs), bisphosphonate, and prednisone. If medications do not help resolve the symptoms of Ribbing disease, a surgical procedure called intramedullary reaming may be recommended.
Case Report
A 45-year- old female patient presented with pain in the right leg for the past 4 months duration, pain gradually progressive and deep seated , the patient also gives history of similar complaints in the left leg 3 years back for which the patient went to an outside hospital where she underwent saucerization of the left tibia as a case of low-grade osteomyelitis. There was no history of fever, trauma, or undue stress on the bones. There was no history of autoimmune diseases in her family. Her general examination was unremarkable. Local examination did not reveal any significant findings except for mild tenderness. Her routine blood investigations were unremarkable.
MRI revealed similar findings; in addition, it revealed bone marrow edema and minimal adjacent soft- tissue inflammation (Fig. 3a, b and c).

Discussion
Ribbing disease is a sclerosing dysplasia of unknown etiology affecting the diaphysis of tubular bones with sparing of epiphyses; it especially affects the tibia and femur. It was first described in 1949 by Ribbing. [2]. It is a disease of adults and the incidence is reported to be more in women, [3], with our patient being a woman too in her fourties. The typical presenting symptom is pain, which may be progressive in nature and associated with physical activity. Ribbing postulated that the disease was transmitted in an autosomal dominant fashion [2], but others suspect that the transmission is autosomal recessive, [4], while yet others believe that Ribbing disease and Camurati-Engelmann disease (progressive diaphyseal dysplasia, OMIM 131300) may represent a phenotypic variation of the same disease. MRI images confirmed diaphyseal sclerosis, both periosteal and endosteal thickening associated with bone marrow signal abnormality are consistent with marrow oedema [5], MRI shows low- signal- intensity areas in the medullary cavity, corresponding to the sclerosis, on all pulse sequences. Associated increased signal on short- tau inversion recovery and proton-density fat-saturation sequences may be seen; this represents bone marrow edema, which is believed to be the cause of pain in these patients (6). The above features were consistent with our patient too. Pathologically, the involved bones manifested cortical and trabecular thickening, and obliteration of the Haversian systems was seen [7]. The diagnosis seems to be simple, but it is not easy. To make an accurate diagnosis of this disease, a couple of aspects are important to note. A comprehensive knowledge of the disease (both its X-ray manifestations and clinical features) should be mastered, ; otherwise, it is very easy to misdiagnose or to have a missed diagnosis. The close mimic of Ribbing disease is Engelmann-Camurati disease, a hereditary sclerosing dysplasia with autosomal dominant inheritance that affects children. Both diseases involve the diaphyses of long tubular bones with sparing of the epiphyses, but Engelmann-Camurati disease is bilaterally symmetrical, whereas Ribbing disease is either unilateral or, if bilateral, always asymmetric. The presence of skull bone involvement, gait and neurologic abnormalities, and anemia with extramedullary hemopoiesis favors Engelmann-Camurati over Ribbing disease [8, 9, 10]. In our patient, base of skull radiograph was normal, while Engelmann disease features trabecular thickening, normal or enlarged Haversian systems, and both osteoblastic and osteoclastic activity, implying bone formation and resorption, . In Ribbing disease, markers for bone formation such as alkaline phosphatase and osteocalcin are not elevated. In addition, the markers of bone resorption such as N-telopeptide, pyridinoline, and deoxypyridinoline cross-links are also normal. Together, these measures of bone metabolism would suggest that Ribbing disease is not a “high turnover” bone state, a finding which may help to differentiate it from Camurati-Engelmann disease [11]. Ribbings disease histopathological study may show osteoblastic activity and this was seen in case of our patient [9]. Chronic sclerosing osteomyelitis is a low- toxicity bone infection and often occurs in teenagers. Patients present with swelling, followed by local pain of a deep, boring nature, especially at night. Lesions in some osteomyelitis patients were discovered without a clear border of skin redness and with swelling and exudate of sinus abscesses. Radiographs consistently reveal hyperosteogeny and sclerosis. The surface of the cortical bone is not flat. This condition mainly manifests itself in a single bone; manifestations in multiple bones are rare. It does not manifest itself in bilateral tibia at the same time, as in this case. Chronic sclerosing osteomyelitis can be excluded if there is bilateral involvement. Sequential symmetrical radiographs of the lower extremities that show sparing of metaphyseal and epiphyseal areas can help differentiate between Ribbing disease and chronic sclerosing osteomyelitis. [12]. Van Buchem disease (hyperostosis corticalis generalisata familiaris) is a hereditary sclerosing dysplasia that affects the long bones; the diaphysis is predominantly affected, but the epiphysis can also be involved. In Van buchem disease there is conspicuous involvement of the jaws [13]. In our patient there was no epiphyseal or jaw involvement and no other features consistent with Van Buchem disease was found. Ribbing disease is mainly a diagnosis of exclusion. The important diagnostic features of Ribbing disease are adult onset, female predominance, absence of similar disease in family members, pain, normal serum markers; sclerosis of the diaphyses of long tubular bones, with sparing of epiphyses (especially affecting the tibia); the bilateral asymmetric involvement of bone, without any cortical break, periosteal reaction, and soft- tissue component; and the absence of involvement of the skull base, the jaw, or other systems, the diagnosis of Ribbing disease was confirmed. After arriving at the diagnosis, as there are no established medical or surgical treatments for Ribbing disease, although there is a single report of a postmenopausal woman with findings consistent with Ribbing disease and elevated markers of bone turnover who responded favorably to treatment with oral pamidronate [14]; the patient was treated conservatively with NSAIDs and pamidronate who had no symptomatic betterment. In a case reported by Beals described that intramedullary reaming dramatically relived pain by removing the sclerotic endosteal new bone [15]. A case reported by Noain-Sanz et al intra medullary reaming was performed and followed up for a year in which the patient was symptoms free post- procedure [16]. In a case reported by Yusuf Oztürkmen et al and Karamehmetoğlu [17] intramedullary reaming was performed for a patient with ribbing disease with good clinical outcome. Considering the experience of above authors we went on with intramedullary reaming of the right tibia. Patients symptoms drastically improved post operatively and is pain free for the past 4 years.
Conclusion
The diagnosis of Ribbing disease is challenging and often misdiagnosed. Ribbing disease is an uncommon cause of a common symptom, it is a rare diaphyseal sclerosing dysplasia. With lack of clinical signs of infection and biochemical evidence of metabolic bone disease and positive clinical, radiological and histological features in favour of ribbing disease helped us in arriving at the diagnosis. Proper work up would help in early diagnosis and management. More evidence is needed to illustrate the effectiveness of medical or surgical treatments for patients with Ribbing disease.
Clinical Message
The patient presenting with leg pain and diaphyseal sclerosis with cortical thickening on radiograph should be thoroughly evaluated for various differential diagnosis, the lesion was misdiagnosed as a case of chronic osteomyelitis by the previous surgeon. The occurrence of such a condition is rare and it may take even years to correctly diagnose the disease.
References
1. Pijls BG, Steentjes K, Schoones JW, Dijkstra SP. Ribbing disease: A systematic review Acta Radiol 2018;59:448-53.
2. Ribbing S. Hereditary, multiple, diaphyseal sclerosis. Acta Radiol 1949;31:522-36.
3. Amberger J, Bocchini CA, Scott AF, Hamosh A. McKusick’s online mendelian inheritance in man (OMIM). Nucleic Acids Res 2009;37:D793-6.
4. Hundley JD, Wilson FC. Progessive diaphyseal dysplasia. Review of the literature and report of seven cases in one family. J Bone Joint Surg Am 1973;55:461-74.
5. Gaeta M, Vinci S, Costa C, Oliviero R, Mazziotti S. MRI in Ribbing disease-a case report. Acta Orthop 2009;80:622-4.
6. Shier CK, Krasicky GA, Ellis BI, Kottamasu SR. Ribbing’s disease: Radiographic-scintigraphic correlation and comparative analysis with Engelmann’s disease. J Nucl Med 1987;28:244-8.
7. Bettini G, Bonvi V. Etiopathogenetic, clinical and radiographic considerations on Ribbing’s disease. (Report of 2 Cases of Familial Nature). Arch Putti Chir Organi Mov 1962;16:58-72.
8. Seeger LL, Hewel KC, Yao L, Gold RH, Mirra JM, Chandnani VP, et al. Ribbing disease (Multiple Diaphyseal Sclerosis): Imaging and differential diagnosis. AJR Am J Roentgenol 1996;167:689-94.
9. Byanyima RK, Nabawesi JB. Camurati-Engelmann’s disease: A case report. Afr Health Sci 2002;2:118-20.
10. Mukkada PJ, Franklin T, Rajeswaran R, Joseph S. Ribbing disease. Indian J Radiol Imaging 2010;20:47-9.
11. Mari C, Catafau A, Carrio I. Bone scintigraphy and metabolic disorders. Q J Nucl Med 1999;43:259-67.
12. Cai Y, Lin H, Huang F, Zheng X, Huang Y, Zhang S. Imaging features and differential diagnosis of multiple diaphyseal sclerosis: A case report and review of literature. Medicine (Baltimore) 2018;97:e11725.
13. Dixon JM, Cull RE, Gamble P. Two cases of Van Buchem’s disease. J Neurol Neurosurg Psychiatry 1982;45:913-8.
14. De Rubin ZS, Ghiringhelli G, Mansur JL. Clinical, humoral and scintigraphic assessment of a bisphosphonate as potential treatment of diaphyseal dysplasia: Ribbing and Cammurati-Engelmann diseases. Medicina (B Aires) 1997;57:56-60.
15. Beals BR, Pearson JM, Mansoor A. Ribbing disease: A case report, a review of the literature, and a description of novel treatment. J Bone Joint Surg Am 2002;84:2050-5.
16. Noain-Sanz E, De Morentin-Garraza JM, Eslava-Gurrea E. Intramedullary reaming in Ribbing disease. Rev Esp Cir Ortop Traumatol 2013;57:231-4.
17. Oztürkmen Y, Karamehmetoğlu M. Ribbing disease: A case report and literature review. Acta Orthop Traumatol Turc 2011;45:58-65.
 |
 |
| Dr. M Lokesh | Dr. Sundar Suriyakumar |
| How to Cite This Article: Lokesh M, Suriyakumar S. A rare case of Ribbing disease – Diagnosis and management. Journal of Orthopaedic Case Reports 2020 July;10(4): 69-73. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com