[box type=”bio”] Learning Point of the Article: [/box]
Melorheostosis, although being rare in itself, can have very unusual clinical presentations and radiological appearances which must be kept in mind while considering the diagnosis.
Case Report | Volume 10 | Issue 6 | JOCR September 2020 | Page 72-75 | Amit Kumar Salaria, Gaganpreet Singh, Ekta Dogra, Naveen Kumar, Praveen Sodavarapu, Deepak Neradi. DOI: 10.13107/jocr.2020.v10.i06.1882
Authors: Amit Kumar Salaria[1], Gaganpreet Singh[2], Ekta Dogra[3], Naveen Kumar[4], Praveen Sodavarapu[1], Deepak Neradi[1]
[1]Department of Orthopaedics, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
[2]Department of Orthopaedics, AIIMS Bathinda, Punjab, India.
[3]Department of Community Medicine, Dr. Radhakrishnan Government Medical College, Hamirpur, Himachal Pradesh, India.
[4]Department of Orthopaedics, Dr. Yashwant Singh Parmar Government Medical College, Nahan, Himachal Pradesh, India.
Address of Correspondence:
Dr. Ekta Dogra,
Department of Community Medicine, Dr. Radhakrishnan Government Medical College, Hamirpur 177001, Himachal Pradesh, India.
E-mail: 1dograekta@gmail.com
Abstract
Introduction: Melorheostosis, on its own, is an extremely uncommon disease. It is non-hereditary, sclerosing bone lesion affecting the adjacent soft tissues. Long bones are commonly involved. About 50% of the cases are evident before 20 years of age. It is gradually progressive and involves the adjacent soft tissues resulting in pain, fibrosis, joint contractures, and limb length discrepancies. Various forms of clinical presentation such as hemimelic, monomelic, mono-ostotic, and polyostotic have been described in the literature. Similarly there are different radiological varients like classical, osteoma , osteopathic striatae , and myositis ossificans.. Treatment is mainly palliative.
Case Report: We describe a highly unusual and extensive involvement of the lower limb in a Melorheostotic patient of 35 years of age with a deformity and limb length discrepancy. X-rays are like that of myositis ossificans and mixed type of pattern with extensive involvement from the pelvis to the toe. There is also intra-articular extension of melorheostosis mimicking synovial chondromatosis. The patient is in our close follow-up and physiotherapy guidance. Such an extensive involvement, along with para-articular and intra-articular involvement, is very rare.
Conclusion: Melorheostosis can extensively involve the whole of the limb right from the pelvis to the digits. It can also extend into the joints producing intra-articular loose bodies. Para-articular soft-tissue masses are also common. Radiologically, it can have a mixture of patterns described in the literature. Close follow-up of the patient is essential so as to provide palliative treatment, deal with the deformities, and to assess the progression of the diseases.
Keywords: Contractures, limb length discrepancy, melorheostosis, sclerosis.
Introduction
Melorheostosis is a rare sporadic, benign sclerosing bone disease that affects the appendicular skeleton (very rarely axial skeleton) and adjacent soft tissues with an incidence of about 0.9/million. It was first described by L”eri and Joanny in 1922 [1]. Numerous theories have been given regarding the etiology and pathogenesis. There is no sex predilection. Long bones are most commonly affected. Various forms of clinical presentation such as hemimelic, monomelic, mono-ostotic, and polyostotic have been described in the literature [2]. Clinically, it may remain asymptomatic for a long time but ultimately progresses to pain, deformity, contractures, and limb length discrepancy. Radiological examination reveals the various patterns of involvement. Diagnosis is usually made with the help of X-rays. It is associated with various clinical entities such as tuberous sclerosis, neurofibromatosis, mesenteric fibromatosis, various anomalies of lymph and blood vessels, capillary hemangiomas, nephrotic syndrome, hypophosphatemic rickets, and many more [3, 4, 5]. The treatment is mainly symptomatic using analgesics anti-inflammatory and bisphosphonates. Surgical treatment is reserved for selected cases, and amputation is the last resort.
Case Report
A 35-year-old male presented to us in the outpatient department with a 17 years old history of pain, stiffness (of the knee, ankle, and foot), and deformity of the left lower limb. There was also a history of limb length discrepancy from the past 8 years. Surgical history revealed that he had undergone surgery of his right knee 10 years back for pain and stiffness at some other institution and some loose bodies were extracted out. Nature of which was not known. The patient was not satisfied with the outcome of the surgery. Medical history revealed that he was on pain killers off and on. There was no history suggestive of infection, trauma, inflammatory arthropathy, or tuberculosis. On examination, there was no tenderness and no signs of inflammation.
There was a flexion deformity of 30° of the knee and equino cavo varus deformity of the foot and the ankle. There was a limb length discrepancy of 7 cm. The patient was ambulatory without any walking aid. There was no sensory loss. Laboratory tests, including complete blood count, erythrocyte sedimentation rate, C-reactive protein, serum calcium, phosphorus, and alkaline phosphatase, were within normal limits. Other tests, including renal function tests, liver function tests, T3, T4, thyroid-stimulating hormone, and parathyroid hormone, were normal. X-rays characteristically showed dense sclerotic nodular, hyperostotic lesions involving the pelvis, femur, tibia, fibulae, and the 1st and 2nd toes. Knees and ankle also showed intra-articular/para-articular involvement. Such an extensive involvement right from the pelvis to toes, including the knee and ankle, has not been reported before. The X-rays did not precisely fit into any of the patterns described in the literature; rather they were of the mixed type. 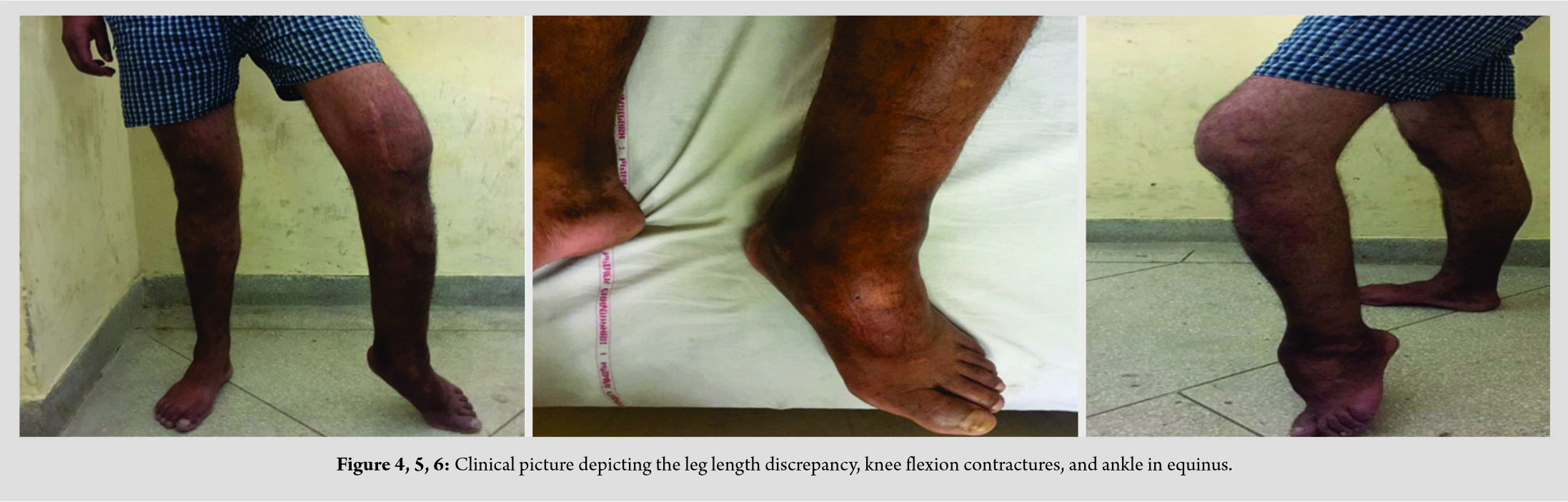
Discussion
Melorheostosis is derived from the Greek word Melos (limb), Rhein (to flow), Ostos (bone) due to its characteristic periosteal hyperostosis giving the appearance of a flowing wax from the candle. It is also known by the various other names such as Leri”s disease, candle bone diseases, and osteosis eburnisans monomelica. The etiology and pathogenesis are still an unsolved mystery. Numerous theories have been proposed. The classical theory of Murray and McCredie suggested that it might be due to the insult of a specific segment or segments of neural crest during embryogenesis. Fryns hypothesis suggested early post-zygotic mesenchymal mutation resulting in asymmetric involvement with vascular and hamartomatous changes of the soft tissues [6, 7]. Two other separate theories suggested by Hellemans and Debeer suggested that loss of function mutations in the LEMD3 gene causes osteopoikilosis and further mutation of this gene as a second hit on the other allele leads to melorheostosis [8, 9]. Diaphysis and epiphyseal regions of the long bones are commonly involved. The clinical presentation can be monomelic, hemimelic, mono-ostotic, or polyostotic. The lower limb is more commonly involved in a sclerotomal distribution. It may extend over the synovial joints and rarely involves the axial skeleton [10]. It is associated with various clinical entities such as tuberous sclerosis, neurofibromatosis, mesenteric fibromatosis, various anomalies of lymph and blood vessels, capillary hemangiomas, nephrotic syndrome, hypophosphatemic rickets, and many more [3, 4, 5]. The clinical course is gradually progressive, with patches of exacerbations and arrest. Various clinical signs and symptoms are pain, stiffness, joint contractures, angular deformities, limb length discrepancies, overlapping toes, neurological involvement due to compression of nerves, para-articular soft-tissue masses, and sometimes intra-articular extension as well [11]. Flowing cortical hyperostosis, along with one side of a long bone resembling that of a melting wax flowing from the side of a candle, is the classical radiological appearance. But there are several radiological variants described in the literature e.g. osteoma, osteopathic ,myositis ossificans and mixed varients [12]. Similarly, in our case, the classical radiological presentation was not there; it was more toward the myositis ossificans like, and in some areas, mixed radiological pattern was there. The various other clinical conditions should be kept in mind while making the diagnosis such as chronic osteomyelitis, myositis ossificans, osteochondroma, paraosteal osteosarcoma, and osteoid osteoma particularly in mono-ostotic types [13]. Higher radiological investigations, such as computed tomography scan, magnetic resonance imaging, radionucleotide scan, and bone biopsy, are warranted in case of any confusion. The treatment is mainly palliative. Analgesics, bisphosphonates, and physiotherapy are the mainstay of treatment. Surgery in the form of release of contractures, corrective osteotomies, tendon lengthening, excision of the fibrous and osseous tissues, capsulotomy, fasciotomy, and even amputations has been described in the literature [14]. Recurrence is common after surgery.
Conclusion
Although benign and rare, melorheostosis can result in tremendous morbidity. It can be extensive in the presentation. Proper awareness of the various radiological and clinical presentations is of paramount importance in the treatment planning of these patients so as to decrease the associated morbidity. Close follow-up and assessment of the clinic radiological progression are also very essential for obvious reasons.
Clinical Message
Melorheostosis can be very extensive in the presentation. It can mimic various clinical entities such as myositis ossificans and synovial chondromatosis. Radiologically, it can have different combinations of patterns.
References
1. Leri A, Joanny J. Une affection non decrite des os: hyperostose en coulee sur toute la longueur d’un membre ou melorheostose. Bull Mem Soc Med Hosp Paris 1922;46:1141–5.
2. Kalbermatten NT, Vock P, Rufenacht D, et al. Progressive melorheostosis in the peripheral and axial skeleton with associated vascular malformations: imaging findings over three decades. Skeletal Radiol 2001;30:48–52.
3. Roger D, Bonnetblanc JM, Leroux-Robert C. Melorheostosis with associated minimal change nephrotic syndrome, mesenteric fibromatosis and capillary haemangiomas. Dermatology 1994;188:166–8.
4. Rhys R, Davies AM, Mangham DC, et al. Sclerotome distribution of melorheostosis and multicentric fibromatosis. Skeletal Radiol 1998;27:633–6.
5. Reznik M, Fried G. Myelopathy associated with melorheostosis: a case report. Arch Phys Med Rehab 2005;86:1495–7.
6. Murray RO, McCredie J. Melorheostosis and the sclerotomes: a radiological correlation. Skeletal Radiol 1979;4:57–71.
7. Fryns JP. Melorheostosis and somatic mosaicism. Am J Med Genet 1995;28:199.
8. Debeer P, Pykels E, Lammens J, et al. Melorheostosis in a family with autosomal dominant osteopoikilosis: report of a third family. Am J Med Genet 2003;119A:188–93.
9. Hellemans J, Preobrazhenska O, Willaert A. Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke–Ollendorff syndrome and melorheostosis. Nat Genet 2004;36:1213–8.
10. Khurana JS, Ehara S, Rosenberg AE, et al. Melorheostosis of ilium, femur, and adjacent soft tissues. Skeletal Radiol 1988;17:53.
11. McLeod RA, Beabout JW, Cooper KL, et al. Case of the day. AJR Am J Roentgenol 1984;142:1062–8.
12. Freyschmidt J. Melorheostosis: a review of 23 cases. Eur Radiol 2001;11:474–9.
13. Parikh J, Hyare H, Saifuddin A. The imaging features of post-traumatic myositis ossificans, with emphasis on MRI. Clin Radiol 2002;57:1058–66.
14. Gong HS, Lee KH, Oh JH, et al. Successful elbowcontracturerelease secondary to melorheostosis a case report. J Bone Joint Surg Am 2008;90:1106.
 |
 |
 |
 |
 |
 |
| Dr. Amit Kumar Salaria | Dr. Gaganpreet Singh | Dr. Ekta Dogra | Dr. , Naveen Kumar | Dr. Praveen Sodavarapu | Dr. Deepak Neradi |
| How to Cite This Article: Salaria AK, Singh G, Dogra E, Kumar N, Sodavarapu P, Neradi D. A Highly Unusual Clinical Presentation and Imaging Appearance of a Rare Diseases: Melorheostosis. Journal of Orthopaedic Case Reports 2020 September;10(6): 72-75. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com





