The combination of the medical treatment leads to the success of the operation for the fracture by the osteomalacia.
Dr. Takahiro Niikura,
Department of Orthopedic Surgery, ,
Kobe University Graduate, School of Medicine, 7-5-1 Kusunoki-cho, ,
Chuo-ku, Kobe – 650-0017, Japan.,
E-mail: tniikura@med.kobe-u.ac.jp
Introduction: Hypophosphatemic osteomalacia can be overlooked or confused with other musculoskeletal disorders due to the variety of associated clinical, laboratory, and radiographic findings. If osteomalacia is diagnosed early and the fractures are not displaced, they often heal with nutritional supplements, but, if they progress to displaced fractures, they may require surgical intervention.
Case Report: We present a case of secondary osteomalacia due to autoimmune polyendocrine syndrome Type 2 due to this condition, the patient developed bilateral tibial proximal fractures and her varus deformity had progressed. No clear indication of the timing for surgery for adults with osteomalacia has been reported. However, medical treatment improves the symptoms of osteomalacia and it is reported that in children, appropriate level of the serum phosphate (P) should be attained and maintained for the successful bone healing after osteotomy. Therefore, we prioritized pharmacological treatment and prescribed surgery after confirming that the value of serum phosphate P had been improved to recommended levels (2.5-3.5 mg/dl). We performed high tibial osteotomy for the right side and gradual correction by an external fixation for the left tibia, because of more severe deformation, and converted to an internal fixation to shorten the treatment period. During conversion, we performed the operation with a locking plate by the minimal invasive plate osteosynthesis method (MIPO).
Conclusion: We conclude that the use of different deformity correction methods, depending on the degree of deformity, and the pharmacological treatment of osteomalacia may lead to favorable results.
Keywords: Osteomalacia, autoimmune polyendocrine syndrome type 2, deformity correction method.
The bone is formed by association of hydroxyapatite crystals, composed of calcium (Ca) and phosphate (P), with the organic matrix, mainly composed of type I collagen. Therefore, if the value of serum calcium Ca and phosphate P becomes too low, bone mineralization is impaired leading to osteomalacia; it occurs after the closure of the epiphyseal line. The failure of calcification of cartilage and bone matrix causes the increase of uncalcified bone matrix and osteoid and the growth inhibition and deformation of the bone and cartilage, which may lead to fracture in advanced cases. It is important to detect and treat osteomalacia early because the fractures highly impact a patient’s patient’s quality of life. We report a case of secondary hypophosphatemic osteomalacia due to autoimmune polyendocrine syndrome type 2 (APS2); the patient developed bilateral proximal tibial fractures and varus deformity. APS2 is a syndrome defined by a characteristic combination of dysfunction of multiple tissues including endocrine glands caused by autoimmune diseases, the patient had celiac disease which caused hypophosphatemia by intestinal malabsorption. Surgical treatment was performed in parallel with pharmacological treatment, resulting in a favorable outcome.
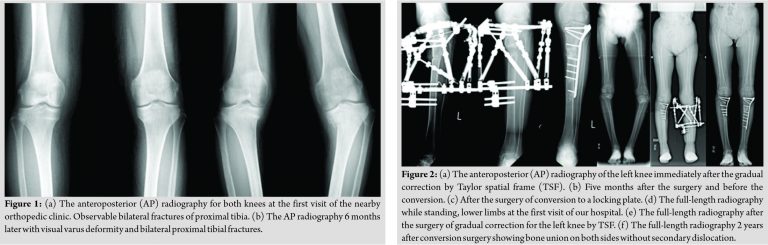
A 44-year-old female with type 1 diabetes was diagnosed with electrolyte abnormality of unknown cause and examined by a nearby physician. She visited an orthopedic clinic due to pain in both knees and was diagnosed with bilateral osteoarthritis (Fig. 1(a)). Six months later, her knees developed varus deformity and the pain worsened. X-ray findings revealed bilateral proximal tibial fractures (Fig. 1(b)) and she was referred to our hospital. The range of motion (ROM) of the knee has slightly extension restriction. The hip-knee-ankle angle was –10.7 degrees for the right and –23.3 degrees for the left. The bone mineral density in the left femoral neck by dual-energy X-ray absorptiometry was 0.383 g/cm2 (T-score:–3.7).
Endocrinologic examinations, in addition to diabetes type 1, revealed hypogonadism, hypothyroidism, hypoadren-ocorticism, and celiac disease; she was diagnosed with APS2. Blood examination showed low serum phosphate P (1.3 mg/dL), low 25-hydroxy vitamin D3, and high alkaline phosphatase (ALP), but normal serum calcium, 1,25-dihydroxy Vitamin D, parathyroid hormone, and fibroblast growth factor 23. She was suspected of secondary hypophosphatemic osteomalacia due to intestinal malabsorption caused by celiac disease and treated with gluten- free diet, oral phosphorus, and alfacalcidol. Oral phosphorus preparations were started by monobasic sodium phosphate P monohydrate at 20 mg/kg/day and the dose was adjusted according to the value of serum phosphorus as appropriate. Alfacalcidol was started at 0.5 μg and continued at the same dose. Three months after the initial visit, the value of serum phosphate P increased from 1.3 to 2.8 mg/dL (Table 1), so we performed open wedge high tibial osteotomy on the right side to correct the varus deformity after the fracture because of rapid progression of varus deformation and difficulty in walking by the limitation of range of motion ROM.
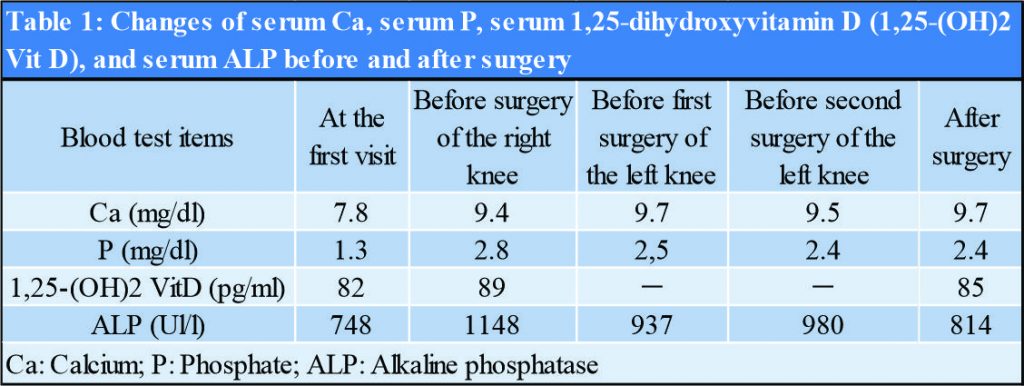
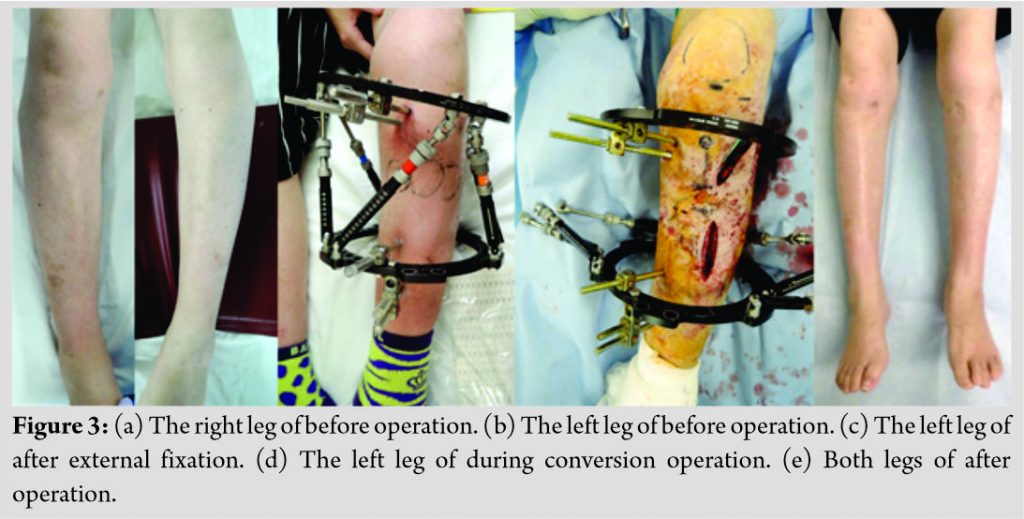
Three months later, we performed gradual correction, using a ring external fixation device (Taylor spatial frame; (TSF) for the left side. Six months later, we removed external fixator and converted to internal fixation with a locking plate (Fig. 2). At the time of conversion, to fix the osteotomy section while maintaining correction and reduce the risk of infection, we replaced the rings and struts of external fixation with the sterilized ones and performed internal fixation with the lateral plate in the state of external fixation by minimal invasive plate osteosynthesis method MIPO (Fig. 3). Two years postoperatively, X-ray showed bone union on both sides without secondary dislocation. The patient was able to walk with a cane. Her knee ROM was almost full recovered and varus deformity was also improved (the medial proximal tibial angle of the right tibia changed from 78° to 87°, the left changed from 68° to 86°). Informed consent was obtained from the patient for publication.
Osteomalacia is a mineralization disorder of the osteoid matrix, due to deficit in calcium Ca and phosphate P [1, 2]. Accumulation of non-mineralized osteoid induces bone fragility and clinically manifests as pain, bone deformity, and muscle weakness. In the developing skeleton, metaphyses are also affected, causing abnormal growth [3]. Administration of phosphate P and Vitamin D preparations improves growth [4] and lower extremity deformities, which are the main clinical manifestations of the affected children [5]. This therapy is generally continued until adult height is achieved. Due to controversy over the treatment, the long-term prognosis of untreated adults is unknown. The reported complications of osteomalacia in adults include joint pain, osteoarthritis, enthesopathy, and fractures [6, 7, 8, 9]. Furthermore, it has not been fully assessed whether all affected adults benefit from therapy. Suzuki et al. reported that symptoms in adult patients with osteomalacia, who discontinued therapy after achieving final height, were improved by treatment with phosphate P and Vitamin D preparations, and none of the patients who restarted the treatment redeveloped serious symptoms [10]. If osteomalacia is diagnosed early and the fractures are not displaced, they often heal with supplementary nutrition [11]. However, if there is a displacement, presumably as a result of torsional, tensile, or shearing stress on the weakened area of the bone, surgical intervention may be required. It is important to prevent fractures that impact patient’’s quality of life by paying attention to bone pain, arthralgia, and muscle weakness and measuring 25-hydroxy Vvitamin D, and differentiate it from other causes of increased serum Alkaline Phosphatase ALP and decreased calcium Ca and phosphate P. In our case, the patient visited a nearby orthopedic clinic due to the pain in both knees and was diagnosed only with bilateral knee osteoarthritis, despite the fact, that the X-ray revealed fragile fractures in both proximal tibiae. If the medical treatment would have been started immediately, the deformation of the lower limbs would have stopped. We considered the following reasons for delayed diagnosis and treatment: The electrolyte abnormality was detected only six 6 years later due to the rare occurrence of patients with APS2 (reported prevalence 1.4 –2.0/100,000) and the orthopedic surgeon did not suspect osteomalacia and informed the patient about absence of any abnormality. We prioritized pharmacological treatment and performed surgery after confirming the improvement of serum P. No indications of the timing of surgery for adult patients with osteomalacia have been reported. However, pharmacological treatment improves the symptoms of osteomalacia; Choi et al. highlighted the significance of the pharmacological treatment, the role of the serum phosphate P value in the deformation of legs and bone elongation in patients with hypophosphatemic rickets and that the bone maturation at the time of bone elongation is significantly delayed when the value of serum phosphate P is 2.5 mg/dl or less [12]. We have concluded that an appropriate level of serum phosphate P should be obtained and maintained for successful bone healing after osteotomy. Considering patients’ compliance and tolerance to the treatment, we performed right tibial osteotomy firstly, and selected gradual correction by TSF for the left tibia due to more severe deformity. When the patient was able to bear weight on right side, we decided to convert to a locking plate due to shorter treatment period and to prevent surgical site infection, leaving only the half pin of the external fixation and replacing the ring and strut with sterile material.
We experienced a rare case of bilateral tibial proximal fractures with varus deformity caused by secondary osteomalacia due to APS2. We conclude that the use of different deformity correction methods, depending on the degree of deformity, and the pharmacological treatment of osteomalacia may lead to favorable results.
In atypical cases of fracture, we should suspect the possibility of osteomalacia and make an early diagnosis, to start medical treatment. It is also necessary to adjust phosphorus levels even when the surgery is required to fix the deformity due to fracture.
References
- 1.Reginato AJ, Falasca GF, Pappu R, McKnight B, Agha A. Musculoskeletal manifestations of osteomalacia: Report of 26 cases and literature review. Semin Arthritis Rheum 1999;28:287-304. [Google Scholar]
- 2.Reginato AJ, Coquia JA. Musculoskeletal manifestations of osteomalacia and rickets. Best Pract Res Clin Rheumatol 2003;17:1063-80. [Google Scholar]
- 3.Shimada T, Kakitani M, Yamazaki Y, Hasegawa H, Takeuchi Y, Fujita T, et al. Targeted ablation of FGF23 demonstrates an essential physiological role of FGF23 in phosphate and Vitamin D metabolism. J Clin Invest 2004;113:561-8. [Google Scholar]
- 4.Miyamoto J, Koto S, Hasegawa Y. Final height of Japanese patients with X-linked hypophosphatemic rickets: Effect of vitamin D and phosphate therapy. Endocr J 2000;47:163-7. [Google Scholar]
- 5.Verge CF, Lam A, Simpson JM, Cowell CT, Howard NJ, Silink M. Effects of therapy in X-linked hypophosphatemic rickets. N Engl J Med 1991;325:1843-8. [Google Scholar]
- 6.Reid IR, Hardy DC, Murphy WM, Teitelbaum SL, Bergfeld MA, Whyte MP. X-linked hypophosphatemia: A clinical, biochemical, and histopathologic assessment of morbidity in adults. Medicine (Baltimore) 1989;68:336-52. [Google Scholar]
- 7.de Menezes Filho H, de Castro LC, Damiani D. Hypophosphatemic rickets and osteomalacia. Arq Bras Endocrinol Metabol 2006;50:802-13. [Google Scholar]
- 8.Berndt M, Ehrich JH, Lazovic D, Zimmermann J, Hillmann G, Kayser C, et al. Clinical course of hypophosphatemic rickets in 23 adults. Clin Nephrol 1996;45:33-41. [Google Scholar]
- 9.Tenenhouse HS, Econs MJ. Mendelian hypophosphatemias. In: Scriver CR, Beaudet AL, Valle D, Sly WS, editors. The Metabolic and Molecular Bases of Inherited Disease. New York: McGraw-Hill; 2001. p. 5039-67. [Google Scholar]
- 10.Suzuki E, Yamada M, Ariyasu D, Izawa M, Miyamoto J, Koto S, et al. Patients with hypophosphatemic osteomalacia need continuous treatment during adulthood. Clin Pediatr Endocrinol 2009;18:29-33. [Google Scholar]
- 11.Lee C, Lashari S. Pseudofracture of the neck of femur secondary to osteomalacia. J Bone Joint Surg Br 2007;89:956-8. [Google Scholar]
- 12.Choi IH, Kim JK, Chung CY, Cho TJ, Lee SH, Suh SW, et al. Deformity correction of knee and leg lengthening by ilizarov method in hypophosphatemic rickets: Outcomes and significance of serum phosphate level. J Pediatr Orthop 2002;22:626-31. [Google Scholar]