[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Osteonecrosis of Talus is a common complication seen after Talus Neck fractures, which can be prevented if they are diagnosed and intervened at the earliest.
Case Report | Volume 11 | Issue 4 | JOCR April 2021 | Page 41-44 | Nagaraj Manju Moger, J. Pragadeeshwaran, Aman Verma, Ankith K.V, K. S. Aditya, Pradeep Kumar Meena. DOI: 10.13107/jocr.2021.v11.i04.2144
Authors: Nagaraj Manju Moger[1], J. Pragadeeshwaran[1], Aman Verma[1], Ankith K.V[1], K. S. Aditya[1], Pradeep Kumar Meena[1]
[1]Department of Orthopaedics, All India Medical Sciences, Rishikesh, India.
Address of Correspondence:
Dr. Pradeep Kumar Meena,
Department of Orthopaedics, All India Medical Sciences, Rishikesh, India.
E-mail: dr.pradsms@gmail.com
Abstract
Introduction: Talus fracture is an uncommon fracture that can be encountered on day- to- day basis. However, it is the 2nd most common tarsal bone to get fractured after calcaneum and accounts for approximately 1% of all fractures around foot and ankle. The anastomotic ring around the talar neck is highly likely to get damaged at the time of the fracture, which, in turn, hampers the blood supply to the body of talus. As a result, the bone healing is delayed and the integrity of the healed fracture is poor which leads to poor functional outcome. Almost 39% cases are missed during the initial evaluation, and talus fracture accounts for almost 50% of all the missed injuries (6–8). A high level of clinical suspicion is required to avoid missing such injuries.
Case Report: A 26-year-old male presented to the outpatient department with chief complaint of pain over the left foot while walking for past 6 months. There was a history of significant trauma to the foot 6 months back (fall from 12 feet) for which he sought medical advice and was managed with analgesics and rest for a couple of weeks. He presented to us 6 months later with chronic, dull aching, and continuous pain which aggravates while walking and standing. The diagnosis of the non-union fracture neck of talus was made after radiology and was managed by open reduction and internal fixation with cannulated cancellous screws along with contralateral iliac crest cancellous bone grafting.
Conclusion: Delay in diagnosing such injuries accelerates the vascular compromise, delays timely intervention, and ultimately leads to increased morbidity.
Keywords: Talar neck fracture, non-union talus fracture, delayed union talus.
Introduction
Talus fracture is an uncommon fracture that can be encountered on day to day basis. However, it is the 2nd most common tarsal bone to get fractured after calcaneum and accounts for approximately 1% of all fractures around foot and ankle [1, 2]. The neck is the most vulnerable part of talus and fractures around the neck constitute 50% of overall talus fractures. The rarity of the fracture and its peculiar blood supply make the talus fracture a medical emergency and has gained importance over the recent years [3]. The anastomotic ring around the talar neck is highly likely to get damaged at the time of the fracture, which, in turn, hampers the blood supply to the body of talus. As a result, the bone healing is delayed and the integrity of the healed fracture is poor which leads to poor functional outcome. The most dreaded complication of talar neck fracture is osteonecrosis of the body of talus which ultimately leads to collapse of the body. Subtalar arthritis is the 2nd most common complication observed following a talar neck fracture [4]. The complications can be as high as 53.3% with subtalar arthritis and 25% with tibiotalar arthritis as reported by Elgafy et al. [5]. Delayed intervention and failure to achieve good reduction in such cases are the major cause of chronic pain, disability, revision surgeries, and poor functional outcomes. An early diagnosis and prompt treatment can significantly reduce the rates of these complications. Talus fractures are typically missed during the initial evaluation, either due to poor clinical examination or inadequate radiological images. Several studies reported that, among all midfoot and ankle fractures, almost 39% cases are missed during the initial evaluation, and talus fracture accounts for almost 50% of all the missed injuries [6, 7, 8]. A high level of clinical suspicion is required to avoid missing such injuries. Use of advanced imaging modalities such as computed tomography, ultrasonography, and magnetic resonance imaging can surely aid in making an early diagnosis and treatment, there by significantly decreasing the long-term complications and morbidity in such patients. We report a case of talus fracture in young male that was missed initially. We present the radiological findings, the intervention done, and the clinical outcome of the case.
Case Report
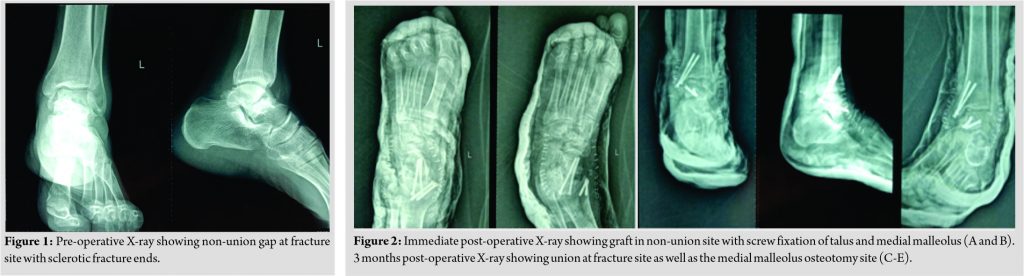
A 26-year-old male presented to the outpatient department with chief complaint of pain over the left foot while walking for past 6 months. There was a history of significant trauma to the foot 6 months back (fall from 12 feet) for which he sought medical advice and was managed with analgesics and rest for a couple of weeks. The patient now presented with chronic, dull aching, continuous pain which aggravated on standing and walking and relieved on rest and analgesics. Patient was mobilizing over the affected foot without any support. Physical examination showed no swelling or tenderness over the talus. Ankle dorsiflexion and plantarflexion movements were full but supination and pronation were terminally painful. There was no distal neurovascular deficit noted. X-ray of the right foot and ankle was taken and a fracture line was noted in the neck of the talus which showed sclerosed fracture ends and talar head (Fig. 1). The diagnosis of non-union fracture talus (Hawkins type 1) was made based on X-ray.
Operative procedure
Patient was positioned in left lateral position under spinal anesthesia. A tourniquet was tied in the mid-thigh for achieving a bloodless field intraoperatively. The surgical incision site marked after palpating the distal tibia, talus, navicular, and tibialis anterior tendon. A 10 cm incision was given, starting 4 cm from the posterior edge of the medial malleolus extending to the anteromedial border of the navicular. After careful dissection of the soft tissues and tendons, the medial malleolus was exposed and osteotomized obliquely. The distal fragment elevated along with the deltoid ligament to expose the talus. Fracture visualized and the fracture ends freshened. Fibrous tissue at the fracture site was curetted. Fracture was reduced and reduction maintained using reduction clamps. Cancellous bone graft procured from the contralateral iliac crest and filled at the fracture site. The talus fracture and the osteotomy site fixed using two cannulated cancellous screws at both sites. Wound closure done in layers and a supporting below knee plaster slab was applied.
Post-operative rehabilitation
The patient was advised non weight bearing mobilization for 4 weeks. Partial weight bearing mobilization started at 5 weeks postoperatively, while full weight bearing mobilization was not done until 3 months postoperatively. Serial radiographs were procured at 3rd and 6th month postoperatively (Fig. 2, 3). The 6th month post-operative radiograph of the patient showed features of complete union of the fracture. Clinically, the patient had no symptoms with full ankle range of movements.
Discussion
Fixation of Talus neck fractures is an absolute necessity to decrease the overall risk of osteonecrosis. Vallier et al. noted that, any delay in fixation of talus neck fracture following a satisfactory reduction had no impact on the development of osteonecrosis [9]. Talus neck fractures are associated with high rates of complications, even when they are intervened timely and in the long run they eventually lead to chronic pain and stiffness off the ankle joint [10]. The disrupted blood supply leads to destruction of the organic component of the bone. The talus being the weight bearing bone develops multiple microfractures ultimately leading to collapse of the talus [11]. It is noted that the amount of soft-tissue injury and the extent of fracture displacement have direct correlation with the development of osteonecrosis [12]. The patient in the case was misdiagnosed initially. The patient presented with swelling and an un-displaced fractures on the radiograph, indicating minimal soft-tissue component, despite that the patient developed osteonecrosis. With the advent of improved surgical techniques and advanced fixation methods, it is extremely important to diagnose such cases at the earliest and a timely intervention is critical in preventing further complications. The treatment options for managing talar osteonecrosis varies from one case to another. The various treatment options available are core decompression, bone grafting, arthrodesis, partial or total talar replacement, and in extreme scenarios total ankle replacement. The choice of the procedure depends on the staging of the disease as classified by Berndt and Harty and the extent of necrosis [13]. The bone graft can be vascularized or non-vascularized (free medial femoral condyle or iliac crest graft). In our case, non-vascular iliac crest cancellous graft was used which showed an excellent outcome with complete union at the end of 6 months without any residual clinical symptoms.
Conclusion
Talar neck fractures might constitute to a small proportion of foot injuries but its association with high rates of post-operative complications makes it even more formidable to treat. Delay in diagnosing such injuries accelerates the vascular compromise, delays timely intervention, and ultimately leads to increased morbidity.
Clinical Message
Talar neck fractures may represent a small proportion of overall foot injuries but having an increased post-operative complication makes them more challenging to treat. Patients should be made aware of these complications and poor outcomes in the long run. Lack of timely diagnosis escalates the vascular insult, delays timely intervention, and increases morbidity.
References
1. Ahmad J, Raikin SM. Current concepts review: Talar fractures. Foot Ankle Int 2006;27:475-82.
2. Juliano PJ, Dabbah M, Harris TG. Talar neck fractures. Foot Ankle Clin 2004;9:723-36.
3. Peterson L, Goldie IF. The arterial supply of the talus: A study on the relationship to experimental talar fractures. Acta Orthop 1975;46:1026-34.
4. Dodd A, Lefaivre KA. Outcomes of talar neck fractures. J Orthop Trauma 2015;29:210-5.
5. Pack M. Level 1 level 1. Group 2018;32:1-23.
6. Wedmore I, Young S, Franklin J. Emergency department evaluation and management of foot and ankle pain. Emerg Med Clin North Am 2015;33:363-96.
7. Khadabadi N, Putti B, Jatti R, Kale D. Management of 1½ month old neglected talus neck fracture: A case report and review of literature. J Sci Soc 2014;41:50.
8. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician 2002;66:785-94.
9. Vallier HA, Nork SE, Barei DP, Benirschke SK, Sangeorzan BJ. Talar neck fractures: Results and outcomes. J Bone Joint Surg Ser A 2004;86:1616-24.
10. Bastos LR, Ferreira RC, Mercadante MT. Analysis of clinical and functional outcome and complications of talar neck fractures. Rev Bras Ortop (English Ed) 2010;45:362-74.
11. Pajenda G, Vecsei V, Reddy B, Heinz T. Treatment of talar neck fractures: Clinical results of 50 patients. J Foot Ankle Surg 2000;39:365-75.
12. Lindvall E, Haidukewych G, DiPasquale T, Herscovici D, Sanders R. Open reduction and stable fixation of isolated, displaced talar neck and body fractures. J Bone Joint Surg Ser A 2004;86:2229-34.
13. Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am 1959;41:988-1020.
 |
 |
 |
 |
 |
 |
| Dr. Nagaraj Manju Moger | Dr. J. Pragadeeshwaran | Dr. Aman Verma |
Dr. Ankith K.V |
Dr. K. S. Aditya | Dr. Pradeep Kumar Meena |
| How to Cite This Article: Moger NM, Pragadeeshwaran J, Verma A, KV Ankith, Aditya KS, Meena PK. Outcome of neglected talus neck fracture and it’s management: A Case Report. Journal of Orthopaedic Case Reports 2021 April;11(4): 41-44. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com

 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]