Total hip arthroplasty using a dual mobility system and posterior soft-tissue repair was needed for a rare case of atraumatic posterior dislocation after SFN fixation of a femoral trochanteric fracture.
Dr. Yasuhisa Yoshida,
Department of Orthopaedic Surgery, Saiseikai Toyama Hospital, 33-1 Kusunoki,
Toyama Prefecture, 931-8533, Japan.
E-mail: magic198308130820@gmail.com
Introduction: Atraumatic hip dislocation after short femoral nail (SFN) fixation for an intertrochanteric fracture is extremely rare.
Case Report: An 84-year-old woman presented with an atraumatic posterior hip dislocation that occurred 8 years after SFN fixation for an intertrochanteric hip fracture. She experienced an acute-onset left hip pain when standing up from a sitting position while bathing at a day care facility. We performed total hip arthroplasty (THA) with a dual mobility system. During the post-operative THA evaluation, the combined anteversion angle was within the optimum range of 57. However, the dislocation recurred after the THA. During the revision THA, a dual mobility system was used to moderately extend the stem neck. Measures were adopted to strain the posterior soft tissues of the hip joint. We speculated that the posterior hip joint capsule ruptured because the support of the posterior hip joint was weak after the intertrochanteric hip fracture. At the final follow-up visit at 6 months after the operation, the hip joint pain had disappeared, and her activities of daily living recovered to almost the same level as her preinjury activities.
Conclusions: We should consider the lack of support of posterior soft tissues as a cause of this atraumatic posterior hip dislocation following intertrochanteric fracture fixation.
Keywords: Atraumatic posterior hip dislocation, post-operative state of intertrochanteric hip fracture, short femoral nail, total hip arthroplasty, dual mobility system.
Femoral intertrochanteric fractures, which are fragility fractures that commonly occur in the elderly, are generally extracapsular. Short femoral nail (SFN) fixation is used in unstable intertrochanteric fractures, and the frequency of its usage has been increasing in recent years [1]. In general, there is no need to reach inside the joint during the surgery. To the best of our knowledge, atraumatic hip dislocation after SFN fixation is extremely rare. We managed a case of atraumatic posterior dislocation that occurred 8 years after SFN fixation, which indicated an intertrochanteric hip fracture, using total hip arthroplasty (THA) with a dual mobility prosthesis.
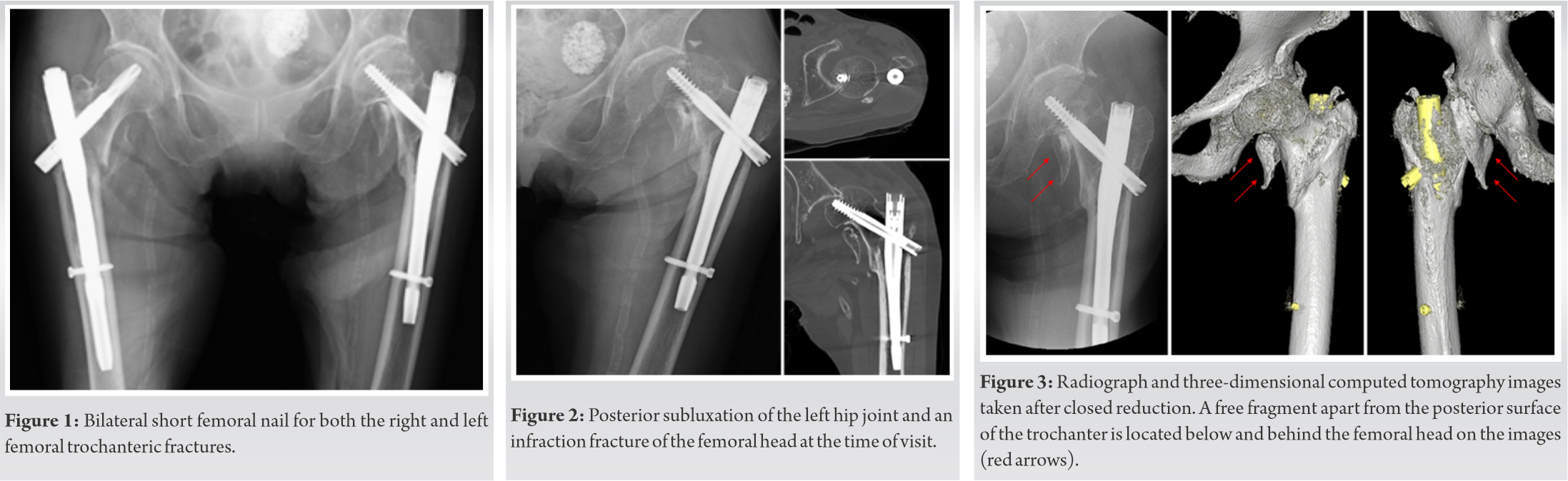
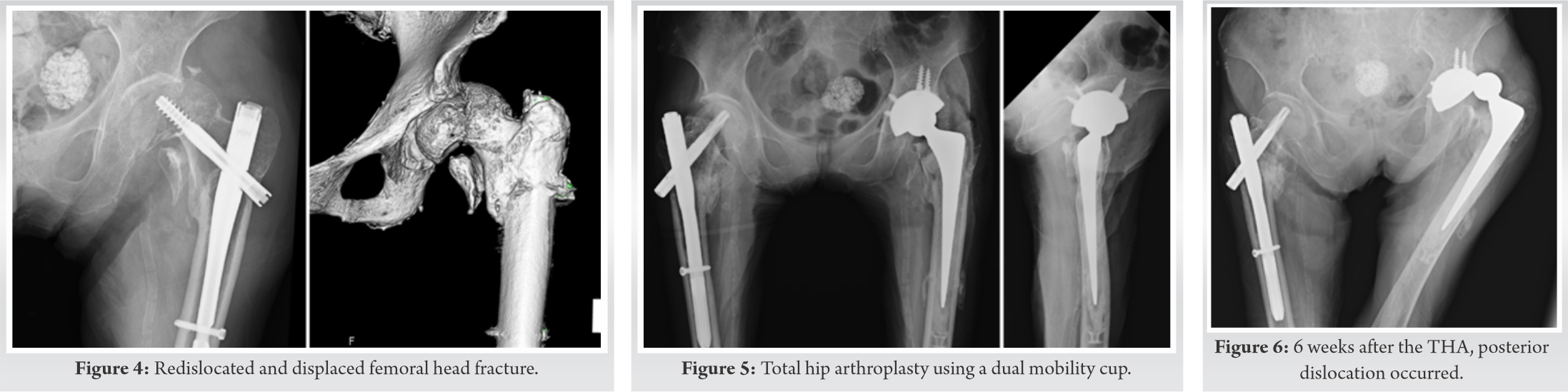
We report the case of an 84-year-old Japanese woman with an atraumatic posterior hip dislocation. She underwent SFN fixation for a left femoral intertrochanteric fracture 8 years before at other facility and another SFN fixation in our hospital for a right femoral intertrochanteric fracture 2 years before (Fig. 1). She experienced an acute-onset left hip pain when standing up from a sitting position while bathing at a day care facility. After her return home with the help of a staff member, a wait-and-see approach was applied, but she continued experiencing difficulty in walking due to the pain. She then consulted an orthopedist at the outpatient department of our hospital 2 days after the onset of the pain. On clinical evaluation, her height was 148 cm; weight, 31 kg; and body mass index, 14.1. She could not stand up from the wheelchair because of difficulty extending her left hip joint. A posterior subluxation of the left hip joint with undisplaced fracture of weight bearing portion of femoral head was identified on plain radiography and computed tomography (CT; Fig. 2). On the images, un-united fragments of the lesser and greater trochanter were also observed.
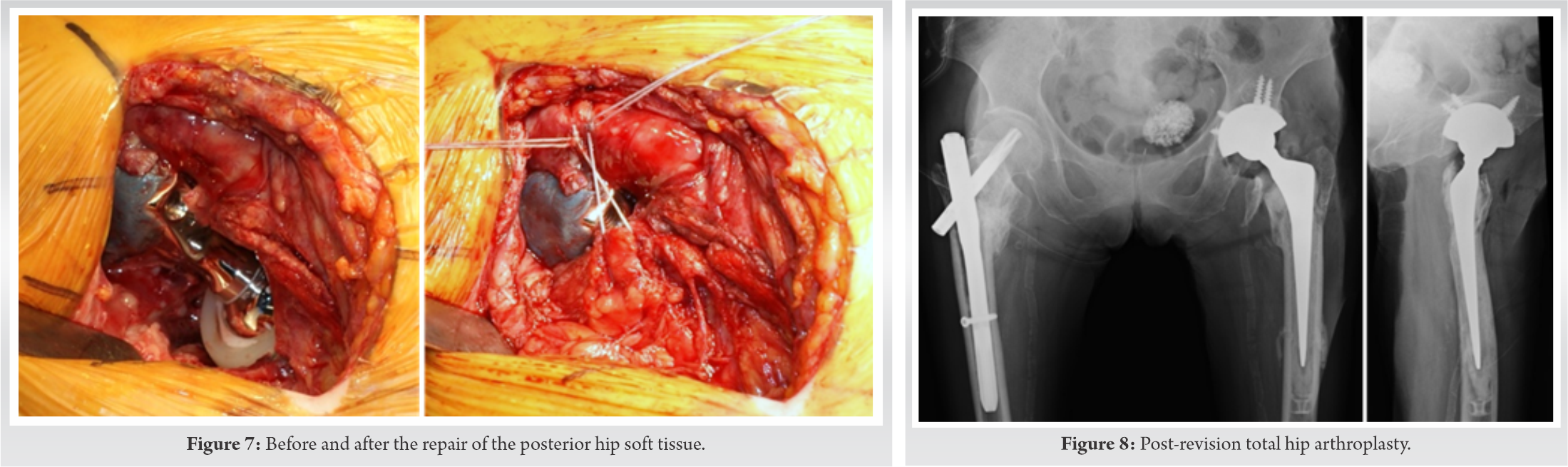
An atraumatic posterior dislocation associated with the femoral head fracture was diagnosed, and closed reduction was immediately performed under fluoroscopy. Reduction by hip flexion and internal rotation under sedation was possible (Fig. 3). She was admitted to the hospital with a hip abduction pillow, but 2 days later, she again complained of left hip pain and was found to have a redislocation and displaced femoral head fracture (Fig. 4).
She underwent surgery 10 days after admission. The operation was performed in the right lateral decubitus position under general anesthesia, and the SFN was removed (Gamma3, Stryker, Kalamazoo, MI, USA). We then performed THA with a dual mobility system (G7 cup 50 mm, Zimmer Biomet, Warsaw, IN, USA) using the posterior approach and installed the cemented stem (CPT size 2 standard, Zimmer Biomet), ensuring proper femoral anteversion. Although no treatment was performed for the un-united fragments the trochanter and for the posterior hip soft tissue, no dislocation tendency was observed in the intraoperative trials (Fig. 5). The post-operative hip abduction pillow was used 2 weeks after the THA. Early post-operative ambulation was started in accordance with the post-operative pain level, and the patient could straighten and raise the affected leg. She received gait training on the 3rd post-operative day. Education and guidance to prevent THA-related dislocation were provided early after the operation, and the patient’s walker-assisted gait gradually became stable and independent.
The positions of the implants were evaluated on the CT images of the hip joint after THA. The cup inclination angle was 28°; cup anteversion angle, 12°; stem antetorsion angle, 45°; and combined anteversion angle, 57°. No abnormalities such as implant loosening or stem sinking were found. However, 6 weeks after the THA, posterior dislocation occurred while the patient was trying to stand up from the nursing-care chair during a shower in the ward (Fig. 6). Closed reduction was immediately performed, and a reduction was easily performed without anesthesia. Frequent recurrence of the dislocations after the THA seemed highly likely at that time, and reoperation was performed 10 days after the THA. The femoral head and bearing were replaced, and the neck was extended by 7 mm using the same dual mobility system. In addition, the free posterior trochanteric fragment was hung and anchored by two strong sutures (No. 2 FiberWire, Arthrex, Naples, FL, USA), striding over the stem-neck across the anterior and posterior femoral trochanters. The fragment was then partially pulled toward the bone defect of the posterior trochanter and fastened to repair the posterior soft tissue of the hip joint. At that time, due to degeneration, the piriformis and short external rotator muscles, which seemed to have inserted in the free fragment, were difficult to detect and identify. Moreover, because the bone fragments could not be drawn completely to the site where the bone defect was present, the posterior surface of the trochanter remained with the bone defect (Fig. 7, 8). After the reoperation, as in the previous surgery, a hip abduction pillow was used for 2 weeks, and early post-operative ambulation was started in accordance with the postoperative pain level. Gait training was performed with a hip orthosis to prevent THA dislocation. Walking with a walker was possible 2 weeks after the revision, and T-cane walking was stable 1 month after the operation. At the final follow-up visit at 6 months after the operation, the hip joint pain had disappeared, and her activities of daily living recovered to almost the same level as her preinjury activities. Her Japanese Orthopaedic Association clinical hip score was 63 points. According to the measurement on the bone density scan obtained using dual energy X-ray absorptiometry of the distal radius, bone mineral density (65%) was lower than the young adult mean.
A femoral intertrochanteric fracture is an extracapsular fracture caused by low-energy trauma that mainly occurs in the elderly. SFN fixation is often chosen as a treatment for unstable intertrochanteric hip fractures. To the best of our knowledge, atraumatic posterior hip dislocation after SFN fixation of intertrochanteric fractures has not been previously reported in the English literature, and only one Japanese study by Yamashita et al. [2] reported a similar dislocation in 2017. In their report, an AO Foundation/Orthopaedic Trauma Association (AO/OTA) [3] 31-A2 trochanteric fracture, which was a Nakano three-dimensional (3D) CT classification [4] type I-3 part A, was reduced to the Fukuda classification [5] inward/extramedullary type after SFN fixation, but the femoral neck was gradually shortened by 22.4 mm, with a bony union during the 1st post-operative year. However, an atraumatic posterior hip dislocation occurred 1 year 9 months after the SFN fixation. The breakage of the joint capsule due to the impingement between the intramedullary nail and the acetabular rim was considered the main cause of the dislocation. The case was treated with conservative measures using a hip orthosis after closed reduction. Our case had no findings of developmental hip dysplasia, and no evidence suggestive of infection or intense inflammation was obtained from the pre-operative examinations and intraoperative findings. Although the details of the intertrochanteric fracture were unknown because the patient had undergone SFN fixation in another hospital 8 years before, on further analysis of the images at the time of visit, we surmised that it was a fragile and unstable AO/OTA [3] 31-A2 fracture and type I-3 part B or C, or type I-4 part of the Nakano 3-D CT classification [4] (Fig. 2). In addition, we can assume that the free posterior trochanteric fragment was compressed between the ischium and femoral neck and impinged due to a slight deformity and sclerotic changes at the medial side of the femoral neck and fragment. As the posterior soft tissue was anatomically attached to the free posterior trochanteric fragment, the support of the posterior hip joint was weak. The posterior hip joint ruptured because of the impingement of the fragment during hip flexion and adduction. The hip dislocation was presumed to be the result of an infraction fracture at the femoral head. Hiranaka et al. [6] proposed a method to evaluate the presence of a femoral anteversion or retroversion after SFN fixation using CT images. On the basis of the direction of the protrusion at the linea aspera in the unaffected femur, we assumed that a poorly fixed position was responsible for the posterior hip dislocation in our case, with reference to the method. However, because the femur on the other side was already operated for an intertrochanteric fracture, it could not be an accurate evaluation. Rather, the affected side was fixed in femoral anteversion at an angle of approximately 10° after SFN fixation by another surgeon. This factor is unlikely to have resulted in posterior dislocation. We speculated that atraumatic hip dislocations occurred after the SFN fixation due to the impingement of the fragment as described previously, but no dynamic appraisal was performed, and the actual definite pathology remains unknown. Due to the recurrence of the hip dislocation after closed reduction, surgery was required. Moreover, both the posterior approach for THA and bipolar hip arthroplasty were indicated for the posterior dislocation and removal of the SFN. However, we were concerned about post-operative dislocation. Considering the presence of some acetabular damage during the pre-operative examination and intraoperative findings, THA using the dual mobility system with substantial resistance to dislocation was indicated [7, 8]. During the post-operative THA evaluation, the cup inclination angle was 28°, which was rather low, but the combined anteversion angle was within the optimum range [9] of 57°. The patient’s comprehension was good; thus, patient education to prevent THA dislocation was conducted after the primary THA. However, the dislocation recurred after the THA. During the revision THA, a dual mobility system was used to moderately extend the stem neck. Measures were adopted to strain the posterior soft tissues of the hip joint. Hence, redislocation had not occurred so far, but the post-operative follow-up period was short, and further monitoring is necessary.
We encountered a rare case of atraumatic posterior dislocation that occurred 8 years after SFN fixation of a femoral trochanteric fracture. The factors involved were impingement due to the bone fragments released by the fracture and joint capsule rupture due to a lack of support of posterior soft tissues. As a preventive measure for post-operative dislocation, THA using a dual mobility system and posterior soft-tissue repair were performed as reported.
There are rare reports of hip dislocations following intertrochanteric fracture SFN fixation related to subsequent trauma or the impingement of the fixation device. This is the first report in English of atraumatic posterior hip dislocation which developed after intertrochanteric fracture fixation with a SFN and treated by THA with a dual mobility system.
References
- 1.Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: Changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am 2008;90:700-7. [Google Scholar]
- 2.Yamashita M, Sasaki M, Osako K, Tomita T, Ueda K, Uchimura T, et al. Atraumatic hip dislocation after osteosynthesis of the femoral intertrochanteric fracture: A case report. Orthop Accid Surg 2017;66:842-6. [Google Scholar]
- 3.Müller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of the long bones. In: Principles of the Classification of Fractures. Berlin: Springer-Verlag Berlin Heidelberg; 1990. p. 4-7. [Google Scholar]
- 4.Nakano T. Understanding of intertrochanteric fractures of the femur in the elderly: 3D-CT classification. Mon Book Orthop 2006;19:39-45. [Google Scholar]
- 5.Fukuda F, Motojima Y, Okada Y, Kurinomaru N, Toba N, Hijioka A. Fracture type at the injury of the femoral trochanteric fractures which made intramedullary type on lateral view after operation. Fracture 2013;35:357-60. [Google Scholar]
- 6.Hiranaka T, Matsuda S, Hida Y, Uemoto H, Tsuji M. Scandalized slice definition on three-dimensional computed tomography for evaluation and classification of trochanteric fracture. Fracture 2016;38:104-9. [Google Scholar]
- 7.Assi C, Kheir N, Samaha C, Kouyoumjian P, Yammine K. Early results of total hip arthroplasty using dual-mobility cup in patients with osteonecrosis of the femoral head. SICOT J 2018;4:4. [Google Scholar]
- 8.Darrith B, Courtney PM, Della Valle CJ. Outcomes of dual mobility components in total hip arthroplasty: A systematic review of the literature. Bone Joint J 2018;100-B:11-9. [Google Scholar]
- 9.Nakashima Y, Hirata M, Akiyama M, Itokawa T, Yamamoto T, Motomura G, et al. Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop 2014;38:27-32. [Google Scholar]