Management of solitary plasmacytoma of the bone, which presents as a pathological fracture with a Mirel’s score advocating internal fixation requires surgical management and adjuvant chemotherapy in order to prevent its progression to multiple myeloma.
Dr. Swapnil A. Keny,
Department of Orthopaedics,
Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India.
E-mail: swapnilakeny@gmail.com
Introduction: Solitary plasmacytoma of the bone is a rare neoplasm characterized by proliferation of neoplastic plasma cells in the bone in the absence of systemic involvement. We present a managed case of a 64-year-old male with solitary bone plasmacytoma of the right proximal femur, who presented as a pathological subtrochanteric femur fracture.
Case Report: A 64-year-old male presented to our outpatient department with pain in the right hip and restricted range of motion following a trivial trauma. The radiographs showed an osteolytic lesion in the right proximal femur with a right subtrochanteric femur fracture. A magnetic resonance imaging scan revealed a well-defined lesion in the right proximal femur. A 18F-fluorodeoxyglucose positron emission tomography did not show a lesion at any other site suggesting that the lesion was solitary. A serum protein electrophoresis study was normal and the urine was negative for myeloma protein. The patient had a score of 12 as per Mirel’s criteria and hence required operative intervention and fixation. The patient was managed with a thorough mechanical and chemical curettage of the lesion followed by fixation with a proximal femur locking plate and augmentation with fibula and iliac crest bone graft. He was then given a chemotherapy regimen consisting of nine cycles of bortezomib, lenalidomide, and dexamethasone.
Conclusion: Solitary bone plasmacytoma is a rare neoplasm of the bone. Early diagnosis and intervention are required to manage it and prevent its progression to multiple myeloma, which is a more aggressive entity and lies at the other end of the spectrum of plasma cell dyscrasias. Management of this lesion requires an active participation of the hematologist and a holistic approach which includes radiotherapy or surgery with possible adjuvant chemotherapy.
Keywords: Solitary bone plasmacytoma, subtrochanteric femur fracture, multiple myeloma, bortezomib, lenalidomide, dexamethasone.
Plasmacytoma is a plasma cell disorder involving abnormal proliferation of plasma cells in the soft tissues or skeletal tissues. Solitary plasmacytoma of bone (SPB) involves local accumulation of monoclonal plasma cells in any part of the bone causing destructive lesions. SPB accounts for approximately 3–5% of all monoclonal gammopathies [1]. These neoplasms lack the CRAB criteria (hypercalcemia, renal insufficiency, anemia, and multiple bone lesions), which is seen in multiple myeloma. Patients present commonly with pain and pathological fractures. Neurological deterioration can be seen when the spine is involved. Approximately 50% of cases progress to multiple myeloma over a period of 4–5 years [1]. A magnetic resonance imaging (MRI) scan is recommended in all patients with a SPB [2]. The lesions appear darker on T1-weighted images and hyperintense on T2-weighted images on MRI [3]. 18F-fluorodeoxyglucose positron emission tomography (FDGPET) is used for detecting lesions at other sites.
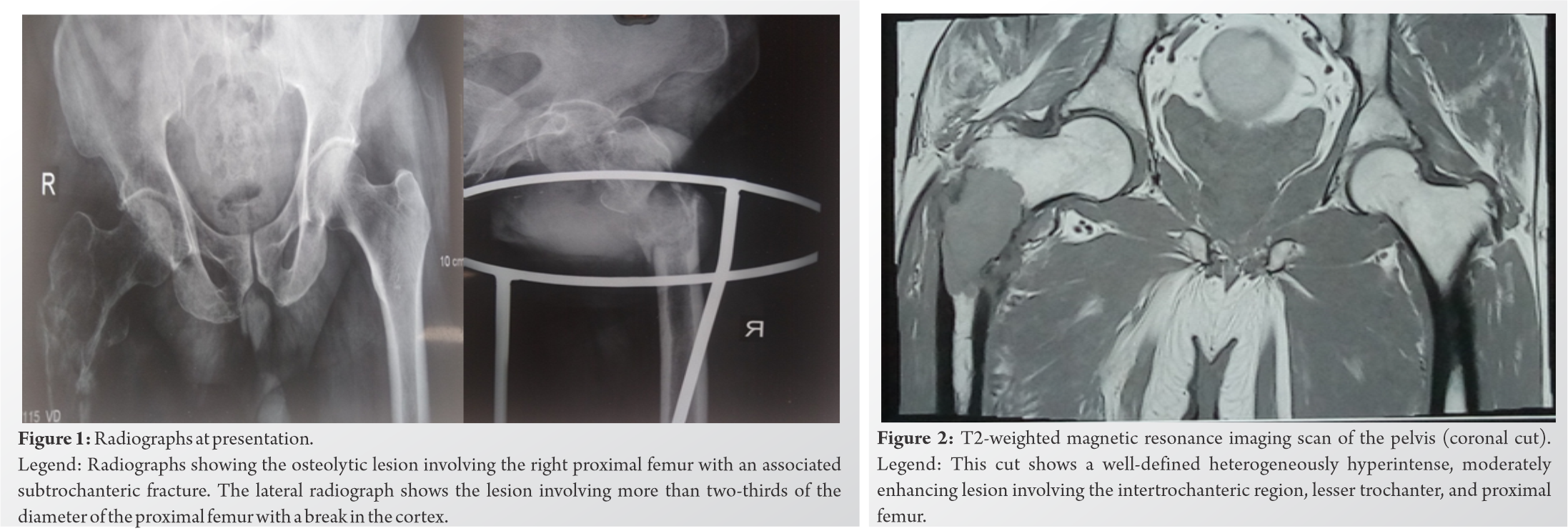
A 64-year-old male presented with pain in the right hip and inability to walk following a trivial trauma. Clinically, the patient had local tenderness at the right hip with a restricted and painful hip range of motion. A radiograph revealed a right femur subtrochanteric fracture with an osteolytic lesion (Fig. 1).
Laboratory investigations for hemoglobin, total protein, serum creatinine, blood urea, and calcium were within normal limits. A serum electrophoresis study was normal, and the urine was negative for myeloma protein. A T2-weighted MRI scan revealed a hyperintense lesion in the intertrochanteric region, lesser trochanter, and proximal femur (Fig. 2). There was a cortical breach and extension into the surrounding muscles and soft tissues. The whole-body FDG-PET scan did not show a metabolically active lesion at any other site (Fig. 3).
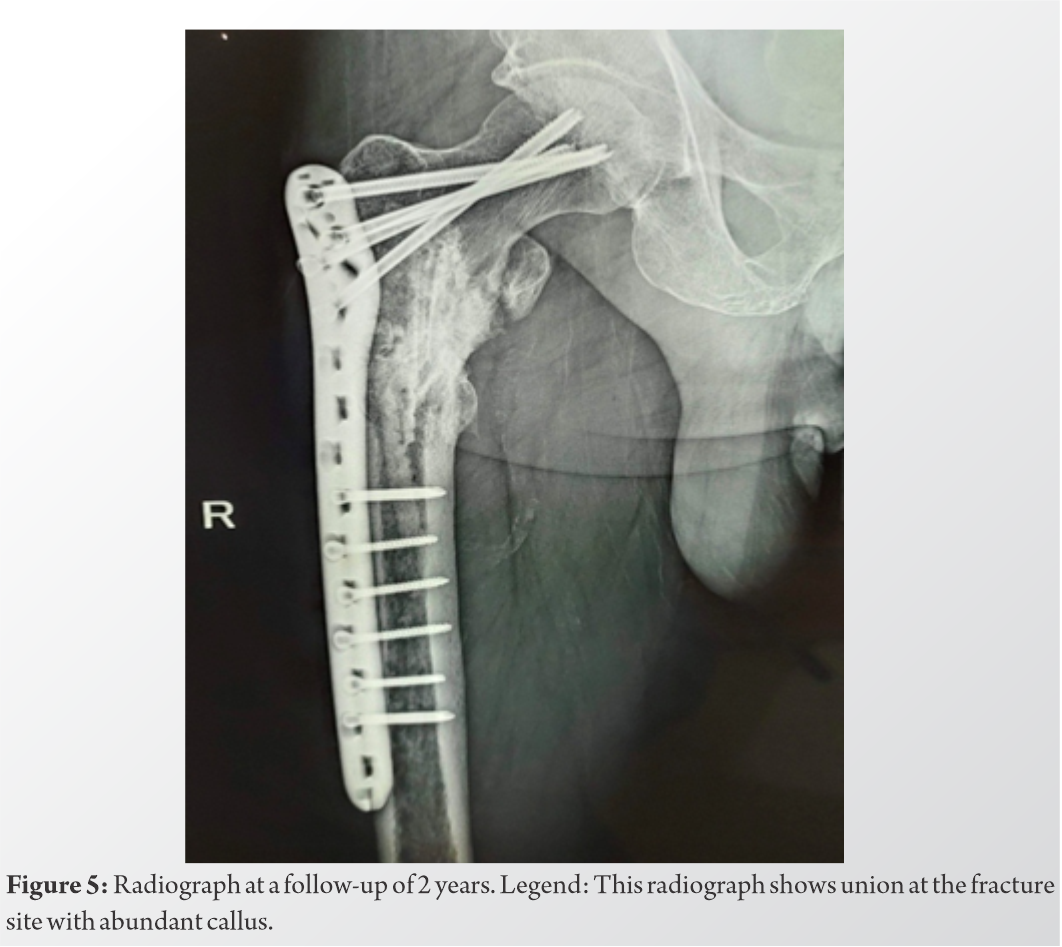
The lesion was approached through the subtrochanteric fracture after localizing under fluoroscopy. Extended intralesional curettage was performed using a hand curette, and the major tumor bulk was removed. The material was sent for a biopsy, which later confirmed the diagnosis of SPB. Following this, phenol (liquefied phenol 91%) was applied to the walls of the tumor cavity for 3–5 min using soaked swabs, following which the cavity was rinsed with 99.5% ethanol. This mixture of phenol and ethanol was extracted by suction, and final irrigation of the tumor cavity was performed with isotonic saline. This cycle was repeated 3 times. Following the mechanical and chemical curettage, fixation was done using a proximal femur locking plate, and augmentation was done using autologous bone graft from the iliac crest and the fibula (Fig. 4). The patient was then managed with 9 cycles of chemotherapy. A single cycle comprised of tablet lenalidomide 10 mg given for 21 days, tablet dexamethasone 40 mg given in the morning with food on days 1, 8, 15, and 22, and injection bortezomib (1.3 mg/m2) given on days 1, 8, 15, and 22. The patient was immobilized for 1-month post-surgery, following which gradual; non-weight bearing mobilization with a walker was started for 3 months. The patient was then mobilized full-weight bearing with a walker, which was gradually withdrawn. The follow-up radiographs at 2 years showed complete union at the fracture site (Fig. 5).
Solitary plasmacytoma can be classified into SPB, solitary extramedullary plasmacytoma (SEP), and multiple solitary plasmacytoma (MSP) [4]. Involvement of bones which actively produce hematopoietic elements is seen commonly in SPB. These include ribs, skull, spine, pelvis, and femur [4]. SPB is diagnosed when there is a solitary lesion of the bone, which is confirmed by a skeletal survey and has a biopsy-proven plasma cell infiltration, the bone marrow biopsy yields a normal result (<10% plasma cells), and there is an absence of myeloma-related organ dysfunction [5]. SEP involves sites other than the bone and accounts for approximately 3% of all plasma cell neoplasms [6]. MSP occurs as a monoclonal plasma cell infiltration in one or more lytic bone lesions, which often spreads to the adjacent tissues and lacks the systemic abnormalities seen in multiple myeloma [7]. SPB appears as a lytic lesion on radiographs and is not associated with a surrounding reactive sclerosis. Other investigations used for confirming diagnosis include computed tomography scan, MRI, serum immunoelectrophoresis, bone scan, and tissue biopsy. The monoclonal nature of plasma cells can be detected by flow cytometry and molecular detection of heavy and light chain rearrangements [8]. Fine-needle aspiration cytology can be used for establishing a provisional diagnosis in a clinically and radiologically unsuspected case of SPB [8]. Management of pathological fractures remains a challenge and includes debulking of the tumor followed by internal fixation and augmentation with methacrylate cement [1]. Matar et al. presented a case of a 57-year-old male with a giant solitary proximal femur plasmacytoma who presented with a giant lytic lesion on radiographs which occupied the medullary canal with thinning of the cortices and was thus not amenable to intramedullary or extramedullary fixation. This patient was managed with a total hip arthroplasty with proximal femur replacement and was followed by a course of chemotherapy. The patient was asymptomatic at 12-month follow-up and had a negative myeloma workup [1]. A lesion size of minimum 5 cm, patients aged 40 years and over, lesions involving the spine, high levels of M protein, the presence of light chains, and the presence of M protein after treatment are few factors associated with a high risk of progression to multiple myeloma [5]. Radiotherapy can be used to eradicate the local lesion as the cells are radiosensitive. Radiotherapy is the treatment of choice for solitary plasmacytoma [9]. Surgery is considered the treatment for plasmacytomas involving distinct locations such as the spine, which presents with neurological compromise and when the tumor causes anatomical instability [9]. The role of chemotherapy in management remains controversial [9]. The Greek group studied the use of novel agents. Twenty-seven patients in their study received novel agents: 22 bortezomib-based regimens and 5 immunomodulatory drugs [9]. However, they concluded that the addition of chemotherapy did not offer any advantage over radiotherapy [9]. Fukuhara et al. reported a case of gastric plasmacytoma managed with resection and chemotherapy using bortezomib, dexamethasone, and cyclophosphamide [10]. Some reports suggest that adjuvant chemotherapy after definitive surgery or radiotherapy may delay progression of SPB to multiple myeloma while others observe no benefit of chemotherapy [11]. Newer agents such as thalidomide and bortezomib have been used successfully in patients with relapsed plasmacytoma [11]. High-grade angiogenesis seen in SPB correlates with progression to multiple myeloma, and hence, antiangiogenic compounds such as thalidomide are useful in this disease [11]. Lenalidomide is a derivative of thalidomide. Kulkarni et al. reported a case of SPB involving the L5 vertebra in a 12-year-old boy which was initially managed as a primary bone lymphoma with antilymphoma therapy and radiotherapy but then showed a recurrence and was successfully treated with decompressive laminectomy and chemotherapy consisting of bortezomib, lenalidomide, and dexamethasone [11]. Adjuvant chemotherapy may be considered in tumors larger than 5 cm in size [12]. The median time of progression of SPB to multiple myeloma is 2–3 years, and the rate is 65–84% in 10 years in spite of curative treatment [5]. We preferred a plate as the implant of choice over intramedullary fixation since our plan was extended intralesional curettage which required a direct access to the lesion. Since we had approached the fracture site as well, it was preferable to use a plate as bone grafting of the entire defect and fixation with plate provided a stronger construct and an excellent biological healing of the lesion as compared to a nail. In case the lesion would have been malignant, there would have been the risk of intramedullary spread of the tumor cells during the steps of intramedullary reaming and nailing. Moreover, the proximal femur locking plate had additional advantages such as a pre-contoured shape and the ability to achieve three-dimensional fixation and provide multiangular stability with locking screws in the femoral head [13].
We have presented a case of a 64-year-old male with a solitary bone plasmacytoma of right proximal femur who presented with a pathological subtrochanteric femur fracture and was managed with surgical debulking of the lesion followed by internal fixation and augmentation with an autologous bone graft and adjuvant chemotherapy”.
Long-term follow-up by a hematologist is required in case of SPB as it has a high chance of progression to multiple myeloma which has a poorer prognosis. Chemotherapy plays an important role in preventing the progression of SPB to multiple myeloma.
References
- 1.Matar HE, Mottram C, Gudena R. Proximal femur giant solitary plasmacytoma of bone: Lessons learnt. BMJ Case Rep 2015;2015:bcr2014204976. [Google Scholar]
- 2.Dimopoulos M, Terpos E, Comenzo RL, Tosi P, Beksac M, Sezer O, et al. International myeloma working group consensus statement and guidelines regarding the current role of imaging techniques in the diagnosis and monitoring of multiple Myeloma. Leukemia 2009;23:1545-56. [Google Scholar]
- 3.He MX, Zhu MH, Zhang YM, Fu QG, Wu LL. Solitary plasmacytoma of spine: A clinical, radiologjc and pathologic study of 13 cases. Zhonghua Bing Li Xue Za Zhi 2009;38:307-11. [Google Scholar]
- 4.Basavaiah SH, Lobo FD, Philipose CS, Suresh PK, Sreeram S, Kini H, et al. Clinicopathological spectrum of solitary plasmacytoma: A single center experience from coastal India. BMC Cancer 2019;19:801. [Google Scholar]
- 5.Kilciksiz S, Karakoyun-Celik O, Agaoglu FY, Haydaroglu A. A review for solitary plasmacytoma of bone and extramedullary plasmacytoma. ScientificWorldJournal 2012;2012:895765. [Google Scholar]
- 6.Purkayastha A, Sharma N, Suhag V, Lohia N. Extramedullary plasmacytoma of oral cavity: Series of three unusual cases at unusual locations. Int J Oral Health Sci 2017;6:26-9. [Google Scholar]
- 7.Dattolo P, Allinovi M, Michelassi S, Pizzarelli F. Multiple solitary plasmacytoma with multifocal bone involvement. First clinical case report in a uraemic patient. BMJ Case Rep 2013;2013:bcr2013009157. [Google Scholar]
- 8.Saksena A, Mahajan N, Agarwal S, Jain S. Solitary bone plasmacytoma: An interesting case report with unusual clinico-cytological features. J Cytol 2014;31:158-60. [Google Scholar]
- 9.Grammatico S, Scalzulli E, Petrucci MT. Solitary plasmacytoma. Mediterr J Hematol Infect Dis 2017;9:e2017052. [Google Scholar]
- 10.Fukuhara S, Tazawa H, Okanobu H, Kida M, Kido M, Takafuta T, et al. Successful treatment of primary advanced gastric plasmacytoma using a combination of surgical resection and chemotherapy with bortezomib: A case report. Int J Surg Case Rep 2016;27:133-6. [Google Scholar]
- 11.Kulkarni RS, Parikh SK, Anand AS, Panchal HP, Patel AA, Trivedi P, et al. Solitary plasmacytoma of bone involving spine in a 12-year-old boy: Report of a rare case and review of literature. J Pediatr Neurosci 2017;12:67-71. [Google Scholar]
- 12.Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Clin Oncol 2004;16:405-13. [Google Scholar]
- 13.Zubairi A, Rashid RH, Zahid M, Hashmi PM, Noordin S. Proximal femur locking plate for sub-trochanteric femur fractures: Factors associated with failure. Open Orthop J 2017;11:1058-65. [Google Scholar]