The treatment of choice for GCT of the proximal femur is a hip arthroplasty with either a standard THA for small confined tumours or endoprosthesis insertion for more extensive tumours.
Dr. Hany Elbardesy,
Department of Trauma and Orthopaedic, Cork University Hospital, Wilton, Cork, Ireland.
E-mail: elbardecy@hotmail.com
Introduction: Giant cell tumors (GCTs) of the bone are uncommon primary bone neoplasms that occur mainly in the epiphysis of long bones. GCT of the femoral head is rarely encountered.
Case Report: We report a rare case of GCT of the femoral head in a 20-year-old female. The patient presented with pathological fracture. The patient underwent total hip arthroplasty (THA). The aim of this paper is to present a case study with pathological fracture of the femoral head and to report the results of a literature review.
Conclusion: The treatment of choice for GCT of the proximal femur is a hip arthroplasty with either a standard THA for small confined tumors or endoprosthesis insertion for more extensive tumors. Joint preserving procedures have a high revision rate (47.06%). Denosumab has been tried as a neoadjuvant treatment with some success in certain cases.
Keywords: Giant cell tumor, pathological fracture, arthroplasty.
Giant cell tumor (GCT) of bone represents 5% of all skeletal tumors. They are more common in young adults and females [1, 2]. Common sites of origin include the metaphyseal-epiphyseal region of the distal radius, proximal tibia, and distal femur [2]. Proximal femoral tumors have been infrequently reported in the literature [3]. GCT is a benign tumor that may become locally invasive leading to extensive bony destruction [4, 5]. Surgical management is the first line of treatment for relieving symptoms, preventing local recurrence, and improving overall patient survivorship [1]. The proximal femur is the location with the highest risk of pathological fracture, which, in turn, may increase the risk of local recurrence [6]. The best treatment option for a pathological fracture of the femoral neck due to GCT is total hip arthroplasty (THA) [7, 8].
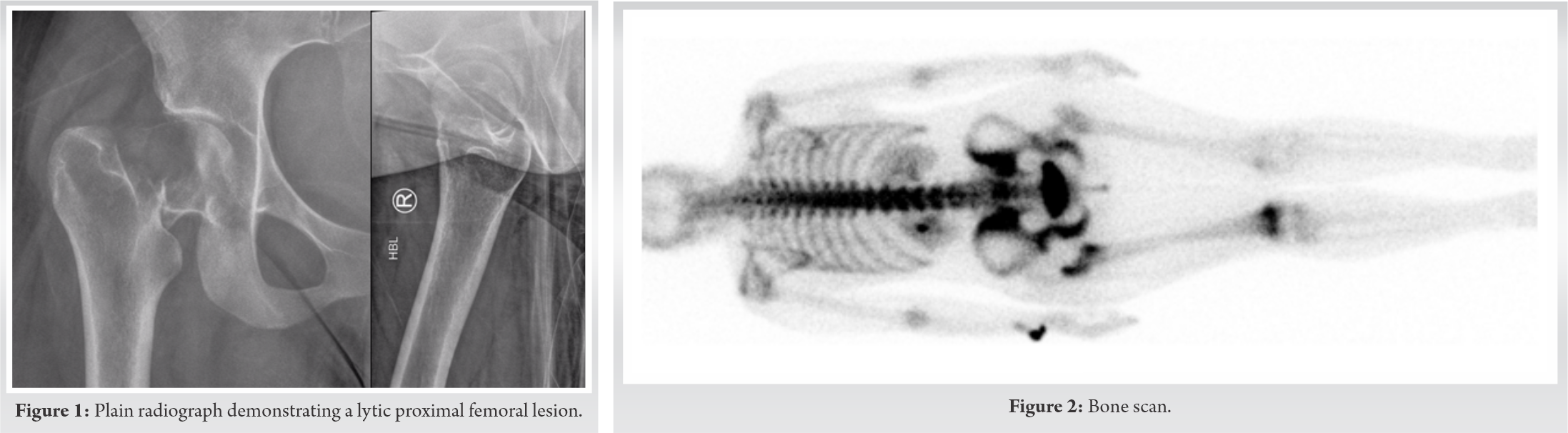
A 20-year-old lady presented to the emergency department with progressive atraumatic right hip pain and an inability to weight bear for 3 months. Plain films showed a pathological fracture of the right femoral neck with an eccentric epiphyseal-metaphyseal lytic lesion (Fig. 1).
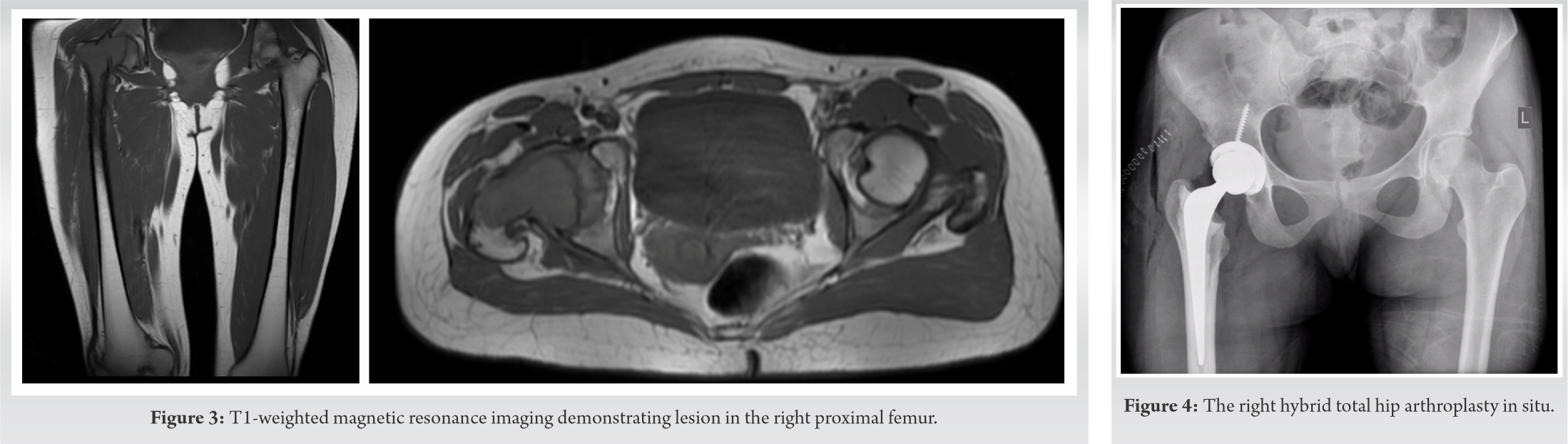
The patient was admitted for further biochemical investigations including a bone profile, inflammatory markers, and full blood count. Radiological investigations included a bone scan (Fig. 2) and magnetic resonance imaging (MRI) of the right femur (Fig. 3).
The MRI showed a solitary lesion in the proximal right femoral metaphysis extending into the femoral epiphysis superiorly and inferiorly to the subtrochanteric level. There was a homogenous appearance on T1-weighted images with a hyperintense signal on T2-weighted images. The main differential diagnoses were GCT, chondroblastoma, and a primary malignant lesion. The patients hip was reconstructed with a hybrid THA (Fig. 4) as the local cauterizing effect of the femoral bone cement has been known to reduce the incidence of local recurrence [7, 8]. Bone samples were sent for the histopathology.
The histopathological report confirmed the diagnosis of GCT due to the appearance of cellular tumor sheets of multinucleate osteoclast giant cells, admixed with a mononuclear round cell population with rare mitotic activity. There was no evidence of a high-grade sarcomatous component. After 1 year from the initial injury, the patient was fully weight-bearing with no limping. We assessed her quality of life and mobility by SF-12, SF-32, and modified Harris hip score (mHHS) [9, 10]. Her SF-12 was 42, SF-32 was 97, and her mHHS was 87. We could not identify any recurrence after 1 year of follow-up.
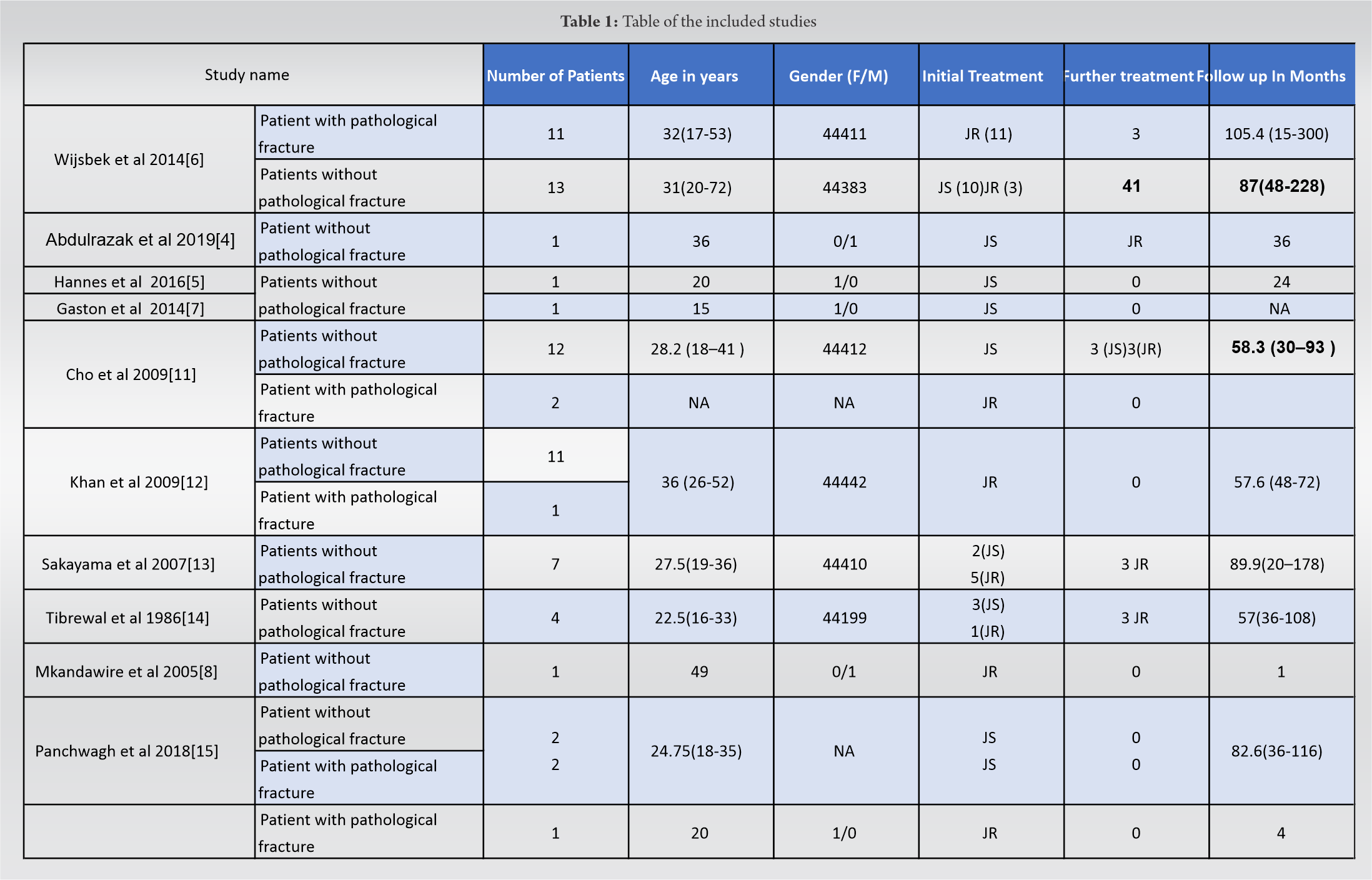
A literature search was conducted on March 27, 2020, using PubMed and EMBASE databases. Search terms included “GCT,” “femoral head,” and “proximal femur” in various combinations to identify articles published in any language. After screening, all articles that met the search criteria were read entirely, and the reference lists were checked for missing relevant publications. No additional studies were found. Our inclusion criteria involved any study describing a GCT of the proximal femur. We identified 10 articles (Table 1), four of which were case studies [4, 5, 7, 8]. The other six were case series. The total number of patients included overall was 69 patients with a proximal femoral GCT. Fifty-three patients (76.8%) had presented with hip pain exclusively without any pathological fracture. Sixteen patients (23.2%) presented with a pathological fracture. Of the 16 patients with a pathological fracture, 14 were treated with THA and the remaining two were treated with joint preservation surgery. These two cases involved curettage and fibular strut bone graft in one and a pediatric dynamic hip screw in another. The total number of patients that been treated with THA was 35. Five patients (11.3%) underwent revision surgery due to disease recurrence. Thirty-four patients (49.3%) underwent joint preservation procedures including curettage with bone cement or bone grafting and internal fixation. Sixteen patients (47%) underwent revision to either a repeat joint preservation procedure (n = 3) or THA (n = 13). GCT of the femoral head may be managed in a number of ways. Due to limited bone stock and high rates of local recurrence, primary excision and reconstruction with THA or end prosthetic replacement has been advocated [7]. Joint preserving procedures in the form of curettage and bone cementing have a high rate of recurrence ranging from 50% to 60% [7, 11]. Rüdiger et al. [5] advocated the use of a transfoveal approach. Medical management includes the use of denosumab as a neoadjuvant treatment to down size the tumor and decrease the recurrence rate after joint preserving procedures [12]. The current best evidence does seem to support THA as only 4 patients (11.43%) underwent revision. Two patients managed with THA had lesions were extending distal to the proximal femur and so an endoprosthesis might have been a preferable option here from the outset. The remaining 88.5% of patients undergoing THA experienced very good outcomes.
GCTs of the hip are commonly associated with pathological fracture and there is a debate surrounds its surgical management.
The treatment of choice for GCT of the proximal femur is a hip arthroplasty with either a standard THA for small confined tumors or endoprosthesis insertion for more extensive tumors. Joint preserving procedures have a high revision rate (47.06%). Denosumab has been tried as a neoadjuvant treatment with some success in certain cases.
References
- 1.Yin H, Cheng M, Li B, Li B, Wang P, Meng T. Treatment and outcome of malignant giant cell tumor in the spine. J Neurooncol 2015;124:275-81. [Google Scholar]
- 2.Miszczyk L, Wydmański J, Spindel J. Efficacy of radiotherapy for giant cell tumor of bone: Given either postoperatively or as sole treatment. Int J Radiat Oncol Biol Phys 2001;49:1239-42. [Google Scholar]
- 3.Saiz P, Virkus W, Piasecki P, Templeton A, Shott S, Gitelis S. Results of giant cell tumor of bone treated with intralesional excision. Clin Orthop Relat Res 2004;424:221-6. [Google Scholar]
- 4.Abdulrazak S, Marzouki A, Bah ST, Lahrach K, Boutayeb F. Giant cell tumour of the femoral neck: Failure of curettage-cavity filling cementation with screw fixation, a case report. Trauma Case Reports 2019;22:100216. [Google Scholar]
- 5.Rüdiger HA, Piasecki K, Becce F, Cherix S. Trans-foveal approach for curettage and bone grafting of a giant cell tumour in the femoral head. HIP Int 2016;26:612-4. [Google Scholar]
- 6.Wijsbek AE, Vazquez-Garcia BL, Grimer RJ, Carter SR, Abudu AA, Tillman RM, et al. Giant cell tumour of the proximal femur: Is joint-sparing management ever successful? Bone Joint J 2014;96:127-31. [Google Scholar]
- 7.Gaston CL, Puls F, Grimer RJ. The dilemma of denosumab: Salvage of a femoral head giant cell tumour. Int J Surg Case Rep 2014;5:783-6. [Google Scholar]
- 8.Mkandawire N. Case report: Giant cell tumour of the neck of femur treated by total hip replacement. Malawi Med J 2005;17:21-8. [Google Scholar]
- 9.Harold RE, Butler BA, Delagrammaticas D, Sullivan R, Stover M, Manning DW. Patient-reported outcomes measurement information system correlates with modified harris hip score in total hip arthroplasty. Orthopedics 2020;44:e19-25. [Google Scholar]
- 10.Lin Y, Yu Y, Zeng J, Zhao X, Wan C. Comparing the reliability and validity of the SF-36 and SF-12 in measuring quality of life among adolescents in China: A large sample cross-sectional study. Health Qual Life Outcomes 2020;18:360. [Google Scholar]
- 11.Cho HS, Park IH, Han I, Kang SC, Kim HS. Giant cell tumor of the femoral head and neck: Result of intralesional curettage. Arch Orthop Trauma Surg 2010;130:1329-33. [Google Scholar]
- 12.Khan SA, Kumar A, Inna P, Bakhshi S, Rastogi S. Endoprosthetic replacement for giant cell tumour of the proximal femur. J Orthop Surg (Hong Kong) 2009;17:280-3. [Google Scholar]
- 13.Sakayama K, Sugawara Y, Kidani T, Miyawaki J, Fujibuchi T, Kamei S, et al. Diagnostic and therapeutic problems of giant cell tumor in the proximal femur. 2007;1:867-72. [Google Scholar]
- 14.Tibrewal SB. Treatment of giant cell tumour of the femoral head and neck. J R Soc Med 1986;79:401-4. [Google Scholar]
- 15.Panchwagh Y, Joshi SK, Sancheti PK. Benign aggressive lesions of femoral head and neck: Is salvage possible? Indian J Orthop 2018;52:51-7. [Google Scholar]