Accurate complete physical examination at the emergency department is crucial for the early diagnosis of Morel–Lavallée in order to decrease complications related to chronic presentation.
Dr. Mohamad K Moussa,
Department of Orthopedic Surgery, Zahraa Hospital, University Medical Center, Beirut, Lebanon.,
E-mail: mhamadmoussa71976798@gmail.com
Introduction: Morel–Lavallée (MLL) is an uncommon entity that is missed by many physicians, it is the result of a shearing force that leads to degloving of the subcutaneous fat from the underlying deep fascia.
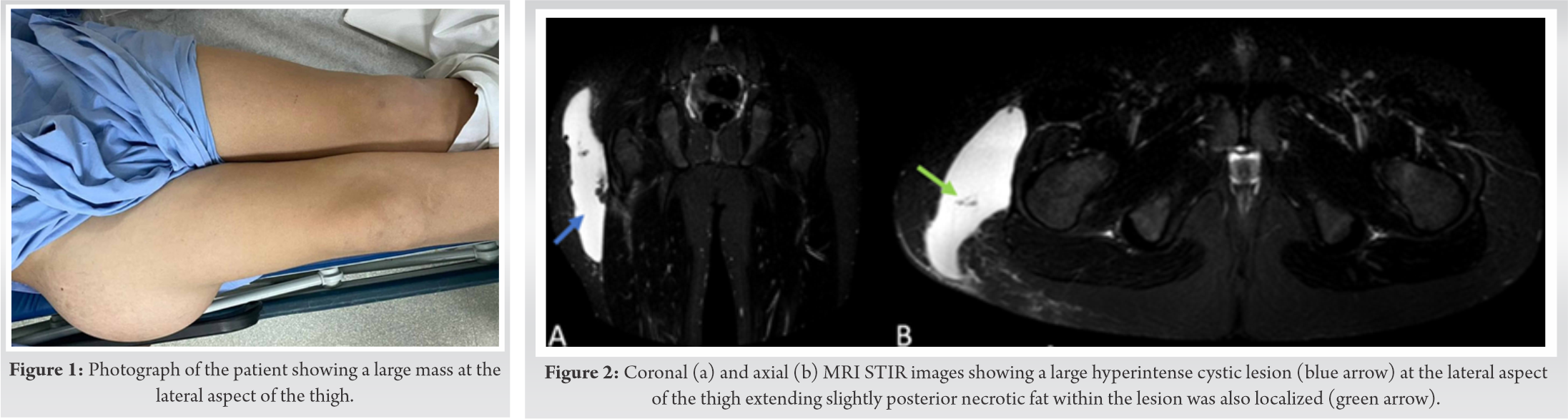
Case Report: We present a case of a 15-year-old male patient who presented 3 months after the initial crush injury with a large MLL lesion at the lateral aspect of the right proximal thigh. He was treated with incision and drainage with compressive dressing and a negative pressure drain.
Conclusion: Diagnosis of MLL is usually clinical and can be aided with radiological tools like MRI that is the gold standard of imaging in this lesion. Several treatment options are available, ranging from conservative treatment with compressive bandages to percutaneous drainage, injection of sclerotic agents, and surgical treatment with incision, drainage, and debridement. Diagnosis and treatment should be familiar to all caregivers to prevent further complications that could be life or organ-threatening.
Keywords: Morel–Lavallée, thigh trauma, chronic Morel–Lavallée, thigh mass.
Morel–Lavallée (MLL) was first described in the 19th century by the French surgeon Victor Auguste [1]. It is usually due to direct trauma with shearing forces leading to complete separation of the skin and subcutaneous fat from the underlying fascia, where the region of the greater trochanter is the most common location to occur followed by the thigh [2]. The separation of the skin and subcutaneous fat creates a dead space in which lymph, necrotic fat, and blood from the disrupted perforators will collect in Hak et al. [3], followed by an inflammatory reaction that will create further permeability to the cavity. After the cavity formation and fluid collection, the inflammatory reaction will lead to the formation of a pseudo capsule that will prevent resorption of the fluids inducing chronic fluid accumulation with a high risk of infection [4, 5]. Hence, early diagnosis and treatment are paramount to prevent late complications that could be life threatening.
A 15-year-old male patient with no previous medical history sustained a low velocity crushing injury to the lateral aspect of the proximal thigh. He did not suffer from any associated injury during the trauma and did not even seek medical advice. Few hours after the insult, he started noticing bruises at the site of trauma but it was not given much attention. Ten days later, he started noticing a mass growing in size at the level of the greater trochanter.
After 3 months of neglection, he sought medical advice. On physical examination, the mass was fluctuant and positive with transillumination, with no systemic signs recorded, blood tests were within normal limits with the absence of infection markers (Fig. 1). Echography was done and showed a 22 × 4.8 cm homogenous hypoechoic mass with some echogenicity seen within swelling of subcutaneous fat. MRI of the right proximal thigh showed longitudinal fluid collection deep to the subcutaneous tissue and superficial to the deep fascia with the previously mentioned size (Fig. 2). A diagnosis of MLL was established and the patient was scheduled for operative treatment with incision, drainage, and debridement. 1.5 L of serosanguinous fluid was drained and necrotic fat was removed from the cavity. This was followed by talc application to increase the chance for recovery. The skin was in good condition so a decision was made to do primary closure with a vacuum drain inserted in the subcutaneous space in addition to compressive dressing. Two weeks later, the drain was removed and the wound healed quite well uneventfully.
MLL was first described in the 19th century by the French surgeon Victor Auguste [1]. It is characterized by a serous fluid collection between the subcutaneous fat and the deep fascia following degloving injuries [6]. It occurs more in females with female to male ratio being 12:1, possibly due to the abundance of fat at the pelvis, thigh, and lumbar regions [6]. It arises mostly at the level of the hip, thigh, lumbar, and scapular regions with an incidence of 30.4% and 20.1% at the greater trochanter and thigh regions, respectively [2, 7]. Although it rarely occurs at knee regions, some reports mentioned it in professional American football players [8, 9]. The cause of MLL is usually a trauma with forces that contain pressure and shear, resulting in separation of the subcutaneous fat from the deep fascia creating a dead space where fluids from the disrupted blood and lymphatic vessels collect in Hak et al. [3], Sawkar et al. [6]. An inflammatory reaction will follow inside the cavity leading to its encapsulation and further preventing the resorption of the fluids [4]. This accumulation will be a platform for bacterial colonization with a high risk of infection [5, 9, 10].
The diagnosis of MLL is usually a clinical diagnosis and should be suspected in all patients presenting with a history of a shearing trauma [2]. These lesions usually take around hours to several days to become visible, with some papers extending this period to several years in one-third of patients [11]. Clinical presentation is usually variable where small lesions might present as a small fluctuating mass or after becoming infected, while larger lesions can cause compression to nearby structures or skin necrosis due to insult to skin vascularity [6].
When the clinical scenario raises the suspicion of MLL, further imaging studies should be done to confirm the diagnosis. MRI is the modality of choice due to its high resolution in evaluating soft tissues, multiplanar images, and precise anatomical details [12, 13]. CT scan has no role in the diagnosis of MLL due to its low resolution in characterizing soft tissues [13]. Ultrasound imaging can also be utilized, but it is not essential, it will show a hypoechoic or anechoic area located deep to subcutaneous tissue in addition to the presence of some hyperechoic structures due to necrotic fat lying in the cavitary lesion.
MLL can be treated conservatively or surgically depending on the chronicity, size, infective status, pain, and discomfort. For small volume lesions, conservative treatment can be considered and is usually by compressive bandages or tapes and rest [14]. If conservative treatment failed or there is recurrence, needle aspiration can be utilized if the volume of the lesion is <50 mL since higher volumes have high rates of failure and recurrence if aspirated [15]. Tseng and Tornetta stated that early percutaneous drainage and debridement were successful in a series of 19 patients [16]. According to Mooney et al., incision and drainage is a successful method for the treatment of MLL, where a 2 cm incision is made in the midline of the lesion over its proximal aspect followed by irrigation with normal saline and betadine solution. A VAC sponge I then used to eliminate the dead space. Another modality of treatment is the utilization of liposuction, where liposuction of the cavity was done and it was shown to be successful with no recurrence after 6 weeks of the procedure [17]. The implementation of sclerosing agents in the treatment of MLL was also described where it is thought that the sclerosing agent can induce fibrosis at the periphery of the lesion. Moreover, the application of talc on lesions older than 3 months was described by Luria et al. on a series of 4 patients where it successfully eliminated the dead space without recurrences [18, 19].
MLL is an entity that is still missed by many practitioners, especially in the emergency department and in polytraumatized patients. Its complications range from organ to life-threatening conditions, thus physicians should be aware of its cause, presentation, complications, and treatment.
Careful physical examination is a key factor for the early diagnosis of MLL lesion and to achieve successful treatment. Talc application may be a good option for chronic cases.
References
- 1.Singh A, Anand A, Mittal S, Sonkar AA. Morel-Lavallee seroma (post-traumatic pseudocyst) of back: a rarity with management conundrum. BMJ Case Rep. 2016;2016:bcr2016216122. Published 2016 Jul 18. doi:10.1136/bcr-2016-216122 [Google Scholar]
- 2.Vanhegan IS, Dala-Ali B, Verhelst L, Mallucci P, Haddad FS. The Morel-Lavallée lesion as a rare differential diagnosis for recalcitrant bursitis of the knee: Case report and literature review. Case Rep Orthop 2012;2012:593193. [Google Scholar]
- 3.Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries: The Morel-Lavallée lesion. J Trauma 1997;42:1046-51. [Google Scholar]
- 4.Mooney M, Gillette M, Kostiuk D, Hanna M, Ebraheim N. Surgical treatment of a chronic Morel-Lavallée lesion: A case report. J Orthop Case Rep 2020;9:15-8. [Google Scholar]
- 5.Doelen TV, Manis A. Conservative management of Morel-Lavallée lesion: A case study. J Can Chiropr Assoc 2019;63:178-86. [Google Scholar]
- 6.Sawkar AA, Swischuk LE, Jadhav SP. Morel-Lavallée seroma: A review of two cases in the lumbar region in the adolescent. Emerg Radiol 2011;18:495-8. [Google Scholar]
- 7.Scaranelo AM, Davanco RA. Pseudocyst formation after abdominal liposuction-extravasations of Morel-Lavallée on MR images. Br J Plast Surg 2005;58:849-51. [Google Scholar]
- 8.Matava MJ, Ellis E, Shah NR, Pogue D, Williams T. Morel-Lavallée lesion in a professional American football player. Am J Orthop (Belle Mead NJ) 2010;39:144-7. [Google Scholar]
- 9.Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallée lesion of the knee: Twenty-seven cases in the National Football league. Am J Sports Med 2007;35:1162-7. [Google Scholar]
- 10.Phillips TJ, Jeffcote B, Collopy D. Bilateral Morel-Lavallée lesions after complex pelvic trauma: A case report. J Trauma 2008;65:708-11. [Google Scholar]
- 11.Powers ML, Hatem SF, Sundaram M. Morel-Lavallée lesion. Orthopedics 2007;30:322-3. [Google Scholar]
- 12.Diviti S, Gupta N, Hooda K, Sharma K, Lo L. Morel-Lavallee lesions-review of pathophysiology, clinical findings, imaging findings and management. J Clin Diagn Res 2017;11:TE01-4. [Google Scholar]
- 13.Mellado JM, Bencardino JT. Morel-Lavallée lesion: Review with emphasis on MR imaging. Magn Reson Imaging Clin N Am 2005;13:775-82. [Google Scholar]
- 14.Harma A, Inan M, Ertem K. The Morel-Lavallée lesion: A conservative approach to closed degloving injuries. Acta Orthop Traumatol Turc 2004;38:270-3. [Google Scholar]
- 15.Nickerson TP, Zielinski MD, Jenkins DH, Schiller HJ. The Mayo clinic experience with Morel-Lavallée lesions: Establishment of a practice management guideline. J Trauma Acute Care Surg 2014;76:493-7. [Google Scholar]
- 16.Tseng S, Tornetta P 3rd. Percutaneous management of Morel-Lavallee lesions. J Bone Joint Surg Am 2006;88:92-6. [Google Scholar]
- 17.Kalaria SS, Boson A, Griffin LW. Liposuction treatment of a subacute Morel-Lavallée lesion: A case report. Wounds 2020;32:E23-6. [Google Scholar]
- 18.Penaud A, Quignon R, Danin A, Bahe L, Zakine G. Alcohol sclerodhesis: An innovative treatment for chronic Morel-Lavallée lesions. J Plast Reconstr Aesthet Surg 2011;64:262-4. [Google Scholar]
- 19.Luria S, Applbaum Y, Weil Y, Liebergall M, Peyser A. Talc sclerodhesis of persistent Morel-Lavallée lesions (posttraumatic pseudocysts): Case report of 4 patients. J Orthop Traumatol 2006;20:435-8. [Google Scholar]