Early diagnosis of Seymour’s fracture and its proper treatment. Differentiating it from Mallet finger.
Dr. Tarang S. Khairnar,
Department of Paediatric Orthopaedics,
Sancheti Institute for Orthopaedics and Rehabilitation, 16, Shivaji Nagar,
Pune – 411 005. Maharashtra, India.
E-mail: tarang_k@hotmail.com
Introduction: A nail bed injury concomitant with an underlying physeal injury of the distal phalanx is termed as “Seymour’s fracture.” These are seemingly innocuous injuries commonly misdiagnosed and are subsequently under-treated. These injuries demand treatment like an open fracture to prevent complications such as infection, growth arrest, and nail dystrophies.
Case Report: A 13-year-old boy suffered Seymour’s fracture of the left ring finger distal phalanx after a direct injury from a dodge ball. The fracture was treated with thorough debridement with normal saline, physeal injury reduction through the wound, and fixation with k-wire passed through the tip of the ring finger, metaphysic, physis, and the tip of the k-wire ending in the epiphysis of the distal phalanx. The nail bed was sutured with 3–0 monofilament absorbable sutures. The fracture healed at 3 months and a 1-year follow-up showed a completely formed nail without any deformity.
Conclusion: Excellent outcome was observed with debridement of the wound, nail bed repair, and fixation with k-wire in our case. Nail bed injuries in children should be treated with a high index of suspicion for Seymour’s fracture as it necessitates treatment like that of an open fracture to avoid complications.
Keywords: Mallet finger, Nail bed injury, Open fracture, Physeal injury, Seymour’s fracture.
Nail bed injuries are quite common in children due to their carelessness and clumsiness. When a nail bed is avulsed or lacerated causing a physeal injury, it is known as “Seymour’s Fracture” [1,2]. These fractures are almost always underestimated followed by under treatment leading to complications such as infection, growth arrest, and nail deformities [3,4,5,6,7]. First described in 1966, Seymour’s fracture [1] is rarely discussed elaborately as a separate entity. Due to modern-day sports, hoverboard transportation mode, etc., these fractures have gained a special interest in literature in the western world [8]. However, there is a paucity of literature on Seymour’s fracture in the Indian scenario. In India, most of the nail bed injuries present either in a busy emergency room or in the peripherals at the primary care center, where there are high chances for this rare and seemingly harmless injury to be misdiagnosed as a simple nail bed injury or mallet finger leading to wrong treatment and increased rate of complications. Plain radiographs are a must and usually sufficient to diagnose an injury to the physis [9]. It is imperative to rule out the aforementioned differentials [10] and treat the fracture as an open fracture to avoid under treatment in the form of conservative management. We intend to report a case of Seymour’s fracture in a 13-year-old boy successfully treated with debridement, k-wire fixation, and suturing of the nail bed and to discuss the differential diagnosis of this rare injury.
A 13-year-old male child sustained a nail bed injury of the left ring finger while playing dodge ball. He presented to us within 12 h after the time of injury. Clinically, the patient had an avulsed nail bed of the left ring finger and a flexion deformity (Fig. 1). Sensations over the fingertip were intact and capillary refill time was normal. There were no other systemic injuries. A lateral radiograph of the ring finger demonstrated Salter–Harris type I physeal injury of the distal phalanx (Fig. 2). These findings led to a diagnosis of open physeal injury of the distal phalanx. Surgical intervention was advised for the same.

Under a ring block and all aseptic precautions, the nail bed was thoroughly irrigated with normal saline through the wound. The distal phalanx physeal injury was reduced through the wound and fixed with k-wire passing through the tip of the ring finger, metaphysis, physis, and the tip of k-wire ending in the epiphysis of the distal phalanx (Fig. 3). The nail bed was sutured back meticulously with 3–0 monofilament absorbable sutures (Fig. 4). An extension splint was applied and the patient was discharged on the same day with oral antibiotics for 5 days. The patient was followed up after 1 week for a wound check. K-wire and splint were removed in the outpatient department after 3 weeks and gentle active exercises were started for distal and proximal interphalangeal joints. At 3 months follow-up, the radiograph showed healed physeal injury (Fig. 5) and clinically there was evident new nail formation (Fig. 6) with a full range of motion at the distal interphalangeal joint. At 1-year follow-up, the patient had a fully recovered nail bed with a well-formed nail and no deformity of the phalanx (Fig. 7).

Seymour’s fracture, a rare fracture but a common cause for complications such as infection, growth disturbances, nail deformity, if undertreated [2]. These injuries can be easily misdiagnosed as a simple nail bed injury or a mallet finger [3]. Understanding the anatomy of distal phalanx helps in understanding the fracture and rule out the aforementioned differentials to reach an apt and comprehensive diagnosis. There are reports of a similar type of nail bed avulsion with physeal injury of the hallux which also warrants treatment as open fracture [11,12,13]. Ugurlar et al. reported similar injury in adults and recommended the term “Seymour-type” fracture for extra-articular distal phalanx fracture with nail bed injury mimicking mallet finger [14]. Infection in a “Seymour-type” fracture has also been reported [15]. The distal phalanx is closely attached to the germinal matrix and the overlying skin; hence, any amount of injury to the nail bed is bound to cause injury to the physis. The extensor tendons are attached to the epiphysis and the flexor tendons are attached to the metaphysis.
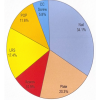
Mallet finger, the most common differential for Seymour’s fracture as both the injuries cause similar flexion deformity of the distal phalanx and hence has a very high chance of being misdiagnosed and subsequently being undertreated in the form of conservative management as a mallet finger would be treated most of the time [10]. In a Mallet’s finger, there is an osseous avulsion fracture of the extensor tendons causing a Salter-Harris type 3/4 physeal injury. The fracture line enters the distal interphalangeal joint. A Seymour’s fracture (avulsion of a nail bed/germinal matrix) causes a Salter-Harris type 1/2 physeal injury. The fracture line does not enter the joint line. This differentiation is important to avoid confusion between a Mallet finger and Seymour’s fracture to avoid future complications. Mallet finger can be treated conservatively with a splint whereas Seymour’s fracture needs to be treated as an open fracture.
Seymour’s fracture is a rare physeal injury of a distal phalanx but a common cause for complications such as infections, growth disturbance, and nail dystrophies. Excellent outcome was observed with debridement of the wound, nail bed repair, and fixation with k-wire in our case. All nail bed injuries in children should be treated with a high index of suspicion for Seymour’s fracture as it necessitates treatment as an open injury.
Seymour’s fracture is a rare physeal injury of a distal phalanx but a common cause for complications suchas infections, growth disturbance, and nail dystrophies. All nail bed injuries in children should be treated with a high index of suspicion for Seymour’s fracture as the injury seems innocuous but it needs to be treated as an open injury.
References
- 1.Seymour N. Juxta-epiphyseal fracture of the terminal phalanx of the finger. J Bone Joint Surg Br 1966;48:347-9. [Google Scholar | PubMed]
- 2.Goodell PB, Bauer A. Problematic pediatric hand and wrist fractures. JBJS Rev 2016;4:01874474-201605000-00003. [Google Scholar | PubMed]
- 3.Reyes BA, Ho CA. The high risk of Infection with delayed treatment of open Seymour fractures: Salter-Harris I/II or juxta-epiphyseal fractures of the distal phalanx with associated nailbed laceration. J Pediatr Orthop 2017;37:247-53. [Google Scholar | PubMed]
- 4.Krusche-Mandl I, Kottstorfer J, Thalhammer G, Aldrian S, Erhart J, Platzer P. Seymour fractures: Retrospective analysis and therapeutic considerations. J Hand Surg Am 2013;38:258-64. [Google Scholar | PubMed]
- 5.Lankachandra M, Wells CR, Cheng CJ, Hutchison RL. Complications of distal phalanx fractures in children. J Hand Surg Am 2017;42:574.e1-6. [Google Scholar | PubMed]
- 6.Nellans KW, Chung KC. Pediatric hand fractures. Hand Clin 2013;29:569-78. [Google Scholar | PubMed]
- 7.Abzug JM, Kozin SH. Seymour fractures. J Hand Surg Am 2013;38:2267-70. [Google Scholar | PubMed]
- 8.Al-Qattan MM. Extra-articular transverse fractures of the base of the distal phalanx (Seymour’s fracture) in children and adults. J Hand Surg Br 2001;26:201-6. [Google Scholar | PubMed]
- 9.Sivit AP, Dupont EP, Sivit CJ. Pediatric hand injuries: Essentials you need to know. Emerg Radiol 2014:21:197-206. [Google Scholar | PubMed]
- 10.Ganayem M, Edelson G. Base of distal phalanx fracture in children: A mallet finger mimic. J Pediatr Orthop 2005;25:487-9. [Google Scholar | PubMed]
- 11.Morris B, Mullen S, Schroeppel P, Vopat B. Open physeal fracture of the distal phalanx of the hallux. Am J Emerg Med 2017;35:1035.e1-3. [Google Scholar | PubMed]
- 12.Kensinger DR, Guille JT, Horn BD, Herman MJ. The stubbed great toe: Importance of early recognition and treatment of open fractures of the distal phalanx. J Pediatr Orthop 2001;21:31-4. [Google Scholar | PubMed]
- 13.Goldie SJ, Sargeant HW, Medjoub K, Rust P, Anderson W. A footballer’s finger injury. BMJ 2013;347:f5069. [Google Scholar | PubMed]
- 14.Ugurlar M, Saka G, Saglam N, Milcan A, Kurtulmus T, Akpınar F. Distal phalanx fracture in adults: Seymour-type fracture. J Hand Surg Eur 2014;39:237-41. [Google Scholar | PubMed]
- 15.Branco PM, Baptista C, Dias CM, Martinho G, Oliveira M, Silva AJ. Infected seymour-type fracture. Gaz Méd 2018;5:136-40. [Google Scholar | PubMed]