Post-traumatic severe manus valgus deformity with ulnar overgrowth in adolescents can be optimally managed by a single stage distal radius and ulnar osteotomy where restoration of ulnar variance and prevention of future distal ulnar overgrowth by distal ulnar epiphysiodesis is important.
Dr. Aniruddha Sinha Sarkar,
Department of Orthopaedics, B.S.M.C.H., Bankura, West Bengal, India.
E-mail: dr.asinhasarkar@gmail.com
Introduction: Distal radius physeal growth arrest in children secondary to trauma is a rare complication. Various modalities of surgical treatment exist. Correction of severe deformity by a single-stage surgery is rare in current literature. We describe a case of surgically treated post-traumatic manus valgus deformity in an adolescent female with a satisfactory surgical outcome.
Case Report: A 13-year-old right-hand dominant girl presented to us with a painless, gradually progressive left wrist deformity for the past 3 years. She sustained a left wrist injury 3.5 years back for which she received native treatment. She was able to do most of her daily activities and cosmetic disability was her primary concern. She had a 20° fixed radial deviation deformity with further radial deviation up to 60°. Forearm rotation was from 70° supination to 60° pronation. Her pre-operative Mayo Modified Wrist Score was 25/10/10/25/70 (Pain/Satisfaction/Range of motion/Grip strength/Total). Radiologically, there was the obliteration of lateral distal radial physis with overgrowth of medial physis. Distal ulnar physeal overgrowth led to positive ulnar variance. Radiologically, the magnitude of deformity was 43° manus valgus (+24° radial inclination). We performed dome osteotomy at distal radius metaphysis with distal radius plating through modified Henry approach. Simultaneous ulnar diaphyseal shortening osteotomy with plate fixation was done through a dorsal approach and distal ulnar epiphysiodesis was done by physeal drilling to prevent future overgrowth. At 13 months follow-up, the wrist has clinically no deformity and radiologically 5° manus valgus (+24° radial inclination). Both the osteotomy sites have united and ulnar variance is restored. Now, her ulnar deviation was 20° and radial deviation was 30°. Her forearm rotational arc was maintained. Mayo Modified Wrist Score was 25/25/10/25/85 (Pain/Satisfaction/Range of motion/Grip strength/Total) with no hindrance of daily activity.
Conclusion: Correction of wrist deformity, restoration of ulnar variance, and normal wrist mechanics is possible in a single-stage surgery with judicious planning and can provide satisfactory result.
Keywords: Wrist, physis, manus, valgus, osteotomy.
Distal radius fractures are the most common long bone fracture in children [1, 2, 3]. Physeal injury occurs in around one-third cases [4]. Symptomatic physeal growth arrest leading to severe deformity is, however, a rare complication that can occur if not intervened early. We report a case of severe manus valgus deformity due to distal radius physeal growth arrest which was successfully treated by distal radius metaphyseal dome osteotomy, ulnar diaphyseal shortening osteotomy with distal ulnar epiphysiodesis.
A 13-year-old right-hand dominant girl presented to our outpatient clinic with painless, gradually progressive deformity of the left wrist for the past 3 years. She gave a history of fall on outstretched hand 3 years 6 months back while cycling and had closed injury to the left wrist with swelling and tenderness for which she received native treatment by some form of splintage for 2 months. She started noticing the deformity after few months, which gradually progressed to the current stage. Documents of the injury and treatment were not available. Although she had restriction of wrist and forearm movement, she was able to perform most of her daily activities. However, the deformity produced cosmetic disability, which was her primary concern. She had attained her menarche.
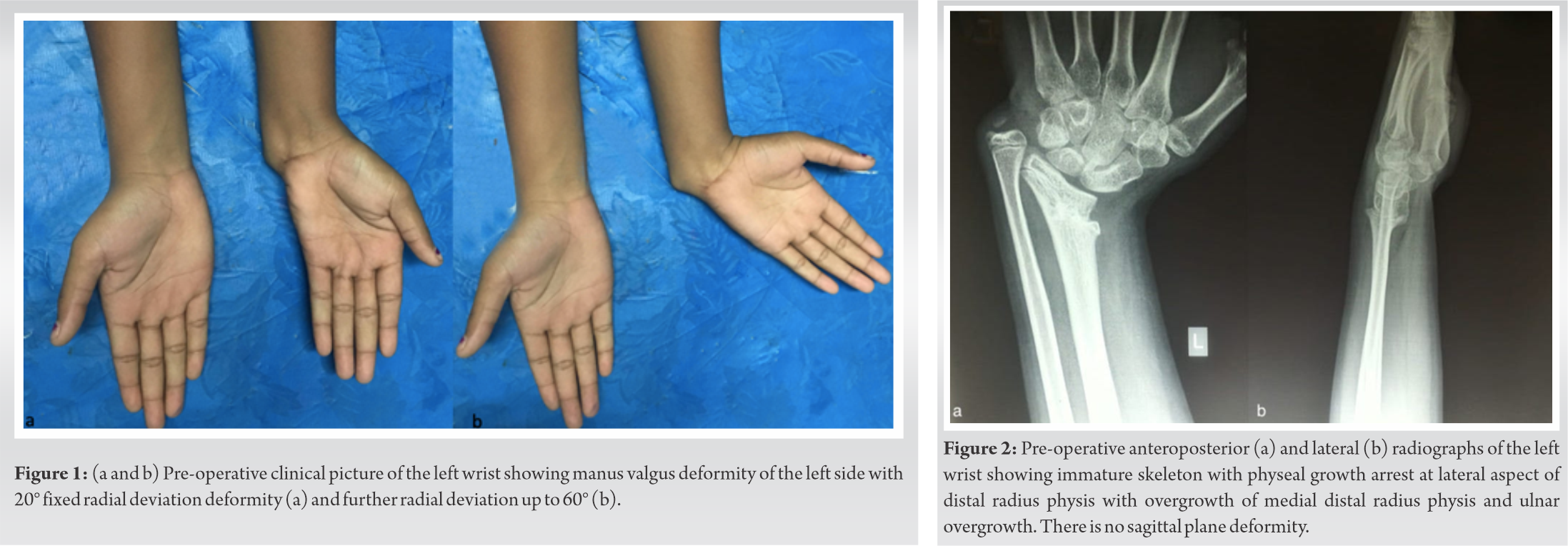
On examination, there was gross valgus deformity of the left wrist without any scars suggestive of previous operative intervention (Fig. 1). The ulnar head was prominent suggesting ulnar overgrowth and there was no bony tenderness. Wrist dorsiflexion and volar flexion, both were 70°. She had a 20° fixed radial deviation deformity with further radial deviation up to 60° (Fig. 1). Forearm rotation was from 70° supination to 60° pronation with an arc of 130°. Her pre-operative Mayo Modified Wrist Score (MMWS) [5] was 25/10/10/25/70 (Pain/Satisfaction/Range of motion/Grip strength/Total). There was no distal neurovascular deficit.
Radiologically, there was the obliteration of lateral distal radial physis with sclerosis and medial physis showed overgrowth (Fig. 2). Distal ulnar physeal overgrowth led to positive ulnar variance. Radiologically, magnitude of the deformity was 43° manus valgus (+24° radial inclination) [6]. There was no sagittal plane deformity.
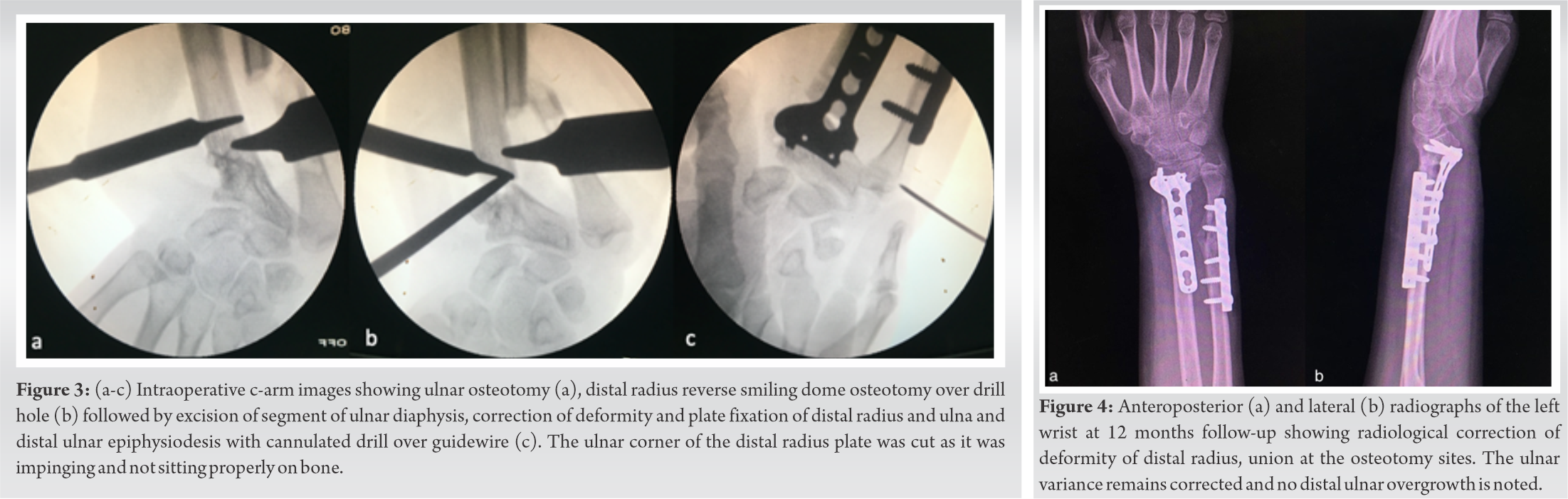
We did a thorough review of the literature and planned for surgical correction by templating the normal opposite wrist joint. Our primary aim was to correct distal radial angulation and restoration of neutral ulnar variance with stable fixation. Under brachial plexus block, after antibiotic prophylaxis, the operative limb was painted, draped and the tourniquet was inflated. Through incision over subcutaneous border of ulna osteotomy of the ulna was done without any bone resection (Fig. 3a). Through modified Henry approach, distal radius osteotomy site was exposed and dome osteotomy was done by connecting multiple drill holes under fluoroscopy guidance (Fig. 3b). The osteotomy was done at the distal radius metaphysis proximal to the center of rotation of angulation (CORA) with proximal convexity. The provisional reduction was held with K-wires and distal radius plating was done with a 3.5 mm distal radius locking plate which was modified by trimming off a distal ulnar part to prevent impingement. Ulnar diaphyseal shortening osteotomy with resection of a segment was done after restoring the ulnar variance followed by six-hole 3.5 mm DCP plate fixation with compression at the osteotomy site (Fig. 3c). Distal ulnar epiphysiodesis was done by physeal drilling with a 2.7 mm drill to prevent future overgrowth (Fig. 3c). Tourniquet was deflated and meticulous hemostasis was achieved. The wound was closed in layers over a suction drain. Temporary below elbow slab was applied, the limb was elevated, and finger movement was encouraged to reduce edema. Two days after surgery, change of dressing was done with removal of drain and slab. Below elbow wrist splint was applied, and gradual intermittent wrist and forearm movement were started. The subsequent post-operative period was uneventful. The patient was followed up at 2 weeks, 6 weeks, 3 months, 6 months, 12 months, and 13 months and she showed good functional recovery without any residual or recurrent deformity or any neurovascular deficit. Both the osteotomy sites united by 5 months. At last follow-up of 13 months, the wrist had clinically no deformity and radiologically 5° manus valgus (+24° radial inclination) with neutral ulnar variance [6]. Her volar flexion and dorsiflexion of the wrist were unchanged. Ulnar deviation was restored to 20° and radial deviation to 30°. She had a forearm rotation arc of 130° (70° supination to 60° pronation). MMWS was 25/25/10/25/85 (Pain/Satisfaction/Range of motion/Grip strength/Total) with no hindrance of daily activity. There was no instability of the distal radioulnar joint. Although absolute correction to normal radial inclination was not achieved, the patient is satisfied with the appearance of the wrist and its function.
Distal radius and ulna contribute to 80% of the overall growth of the forearm which explains the cause of symptomatic deformity due to distal radius physeal growth arrest [7]. Distal radius fracture leading to premature physeal closure is, however, a rare complication with an overall incidence of 4–7% [8, 9]. The physeal growth arrest may be the result of the initial injury itself or may be iatrogenic [9, 10, 11]. Majority of these patients are asymptomatic with symptomatic severe deformity occurring when growth arrest is more than 1 cm [8]. Physeal bar, when detected early, can be treated easily before the development of severe deformity by non-operative method if remaining growth can lead to <2 mm of positive ulnar variance as predicted by multiplier method mentioned by Paley et al. [12]. More than 2.5 mm predicted growth of distal ulna relative to distal radius can lead to ulnar impaction with altered wrist mechanics and it needs surgical intervention [11, 13]. Modality of early surgical intervention includes removal of physeal bar and placement of interposition material into the void to permit the remaining growth, thus preventing complex reconstructive procedures with significant morbidity [11, 12]. Treatment modalities for more severe deformities include corrective osteotomy of the distal radius, epiphysiodesis of the distal ulna with or without radial lengthening, and ulnar shortening osteotomy [10, 11, 13, 14, 15, 16]. The gradual lengthening of the distal radius using the principle of distraction osteogenesis has been reported in the literature but it is technically challenging [11, 14]. The CORA in our case was at the level of physis, so the osteotomy was done proximally in the metaphysis to aid better distal fixation by plate [17]. Dome osteotomy was considered as it provides a large cross-sectional area of bone contact and the stability it provides without the need for bone grafting [18, 19]. Waters et al. in their study of 32 patients had the complication of residual distal ulnar overgrowth after surgery in two cases [13]. Hence, to prevent this complication following ulnar plating, ulnar physeal drilling was done with a 2.7 mm drill to prevent future ulnar overgrowth [20]. In this case, we achieved a good improvement of the total MMWS from 70 to 85, which is concordant with the studies mentioned in the literature [13]. Although various case reports and series have been mentioned in the literature, good outcome following surgery in a deformity of this magnitude was not found.
Satisfactory result can be achieved by correction of deformity, restoration of ulnar variance, and normal wrist mechanics by distal radius dome osteotomy together with ulnar diaphyseal shortening and distal ulnar epiphysiodesis in severe post-traumatic manus valgus deformity through judicious pre-operative planning.
Single-stage surgery for severe manus valgus deformity with positive ulnar variance secondary to physeal growth arrest of distal radius when done after proper planning can give satisfactory cosmetic and functional result.
References
- 1.Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: A study of 3, 350 children. J Orthop Trauma 1993;7:15-22. [Google Scholar]
- 2.Landin LA. Fracture patterns in children. Acta Orthop Scand 2009;54:3-109. [Google Scholar]
- 3.Worlock P, Stower M. Fracture patterns in nottingham children. J Pediatr Orthop 1986;6:656-60. [Google Scholar]
- 4.Mann DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in 2, 650 long-bone fractures in children aged 0-16 years. J Pediatr Orthop 1990;10:713-6. [Google Scholar]
- 5.Carter PB, Stuart PR. The Sauve-Kapandji procedure for post-traumatic disorders of the distal radio-ulnar joint. J Bone Joint Surg Br 2000;82:1013-8. [Google Scholar]
- 6.Schuind FA, Linscheid RL, An KN, Chao EY. A normal data base of posteroanterior roentgenographic measurements of the wrist. J Bone Joint Surg Am 1992;74:1418-29. [Google Scholar]
- 7.Pritchett JW. Longitudinal growth and growth-plate activity in the lower extremity. Clin Orthop Relat Res 1992;275:274-9. [Google Scholar]
- 8.Cannata G, de Maio F, Mancini F, Ippolito E. Physeal fractures of the distal radius and ulna: Long-term prognosis. J Orthop Trauma 2003;17:172-9; discussion 179-80. [Google Scholar]
- 9.Lee BS, Esterhai JL Jr., Das M. Fracture of the distal radial epiphysis. Characteristics and surgical treatment of premature. Clin Orthop Relat Res 1984;185:90-6. [Google Scholar]
- 10.Aminian A, Schoenecker PL. Premature closure of the distal radial physis after fracture of the distal radial metaphysis. J Pediatr Orthop 1995;15:495-8. [Google Scholar]
- 11.Abzug JM, Little K, Kozin SH. Physeal arrest of the distal radius. J Am Acad Orthop Surg 2014;22:381-9. [Google Scholar]
- 12.Paley D, Gelman A, Shualy MB, Herzenberg JE. Multiplier method for limb-length prediction in the upper extremity. J Hand Surg Am 2008;33:385-91. [Google Scholar]
- 13.Waters PM, Bae DS, Montgomery KD. Surgical management of posttraumatic distal radial growth arrest in adolescents. J Pediatr Orthop 2002;22:717-24. [Google Scholar]
- 14.Murase T, Oka K, Moritomo H, Goto A, Sugamoto K, Yoshikawa H. Correction of severe wrist deformity following physeal arrest of the distal radius with the aid of a three-dimensional computer simulation. Arch Orthop Trauma Surg 2009;129:1465-71. [Google Scholar]
- 15.Valverde JA, Albiñana J, Certucha JA. Early posttraumatic physeal arrest in distal radius after a compression injury. J Pediatr Orthop B 1996;5:57-60. [Google Scholar]
- 16.Hove LM, Engesaeter LB. Corrective osteotomies after injuries of the distal radial physis in children. J Hand Surg Br 1997;22:699-704. [Google Scholar]
- 17.Paley D. Principles of Deformity Correction. 1st ed. Berlin: Springer; 2002. [Google Scholar]
- 18.Paley D, Orthopedic P. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:425-65. [Google Scholar]
- 19.Steinman S, Oishi S, Mills J, Bush P, Wheeler L, Ezaki M. Volar ligament release and distal radial dome osteotomy for the correction of madelung deformity: Long-term follow-up. J Bone Joint Surg Am 2013;95:1198-204. [Google Scholar]
- 20.Atar D, Lehman WB, Grant AD, Strongwater A. Percutaneous epiphysiodesis. J Bone Joint Surg Br 1991;73:173. [Google Scholar]