When orthopedic surgeons encounter patients who complain of numbness and pain of their lower extremity and who have medical histories of asthma or eosinophilic pneumonia, Eosinophilic granulomatosis with polyangiitis should be considered.
Dr. Ryotaro Kumahara,
Department of Orthopaedic Surgery,
Hirosaki University Graduate School of Medicine,
5, Zaifu-cho Hirosaki 0368562, Japan.
E-mail: kuma0207@gmail.com
Introduction: Eosinophilic granulomatosis with polyangiitis (EGPA) patients with mononeuropathy multiplex often visit orthopedic clinics; however, orthopedic surgeons have limited experience in diagnosing EGPA because of its rarity. We report a case of EGPA that required 1 month to confirm the diagnosis.
Case Report: A 48-year-old woman presented with acute onset numbness in the right lower extremity. She had muscle weakness of the right lower extremity; lumbar spine magnetic resonance imaging showed lumbar disc herniation. Despite conservative treatment, her symptoms worsened. Blood tests showed increased eosinophils and serum IgE. She was diagnosed with EGPA, which should be considered in case of atypical paralytic symptoms.
Conclusion: EGPA is so difficult to diagnose. In our case, the symptoms worsened on the 30th day after the initial visit. She was diagnosed with EGPA by a blood test at the time of admission. If patients with bronchial asthma or a history of allergies develop lumbar radiculopathy or peroneal nerve palsy-like symptoms, EGPA should be considered, and steroid treatment should be initiated early.
Keywords: Eosinophilic granulomatosis with polyangiitis, peroneal nerve palsy, lumbar disc herniation, asthma.
Eosinophilic granulomatosis with polyangiitis (EGPA) is a very rare disease that is difficult to diagnose [1,2,3]. It has been reported that 50–70% of patients with EGPA present with asthma and eosinophilic pneumonia as initial symptoms [2,4]. Mononeuropathy multiplex in the lower extremities causes muscle weakness and dysesthesia, and these symptoms are similar to radiculopathy caused by lumbar disc hernia (LDH) or lumbar spinal stenosis [5]. As many as, 50–78% of patients with EGPA suffer from neuropathy of the lower extremity such as peroneal nerve palsy [6]. Therefore, differentiation from the peroneal nerve palsy is required. Here, we report a case of polyneuritis due to EGPA that required differentiation from peroneal nerve palsy and/or LDH. Our patient was informed that data concerning the case would be submitted for publication.
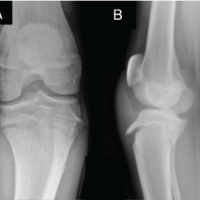
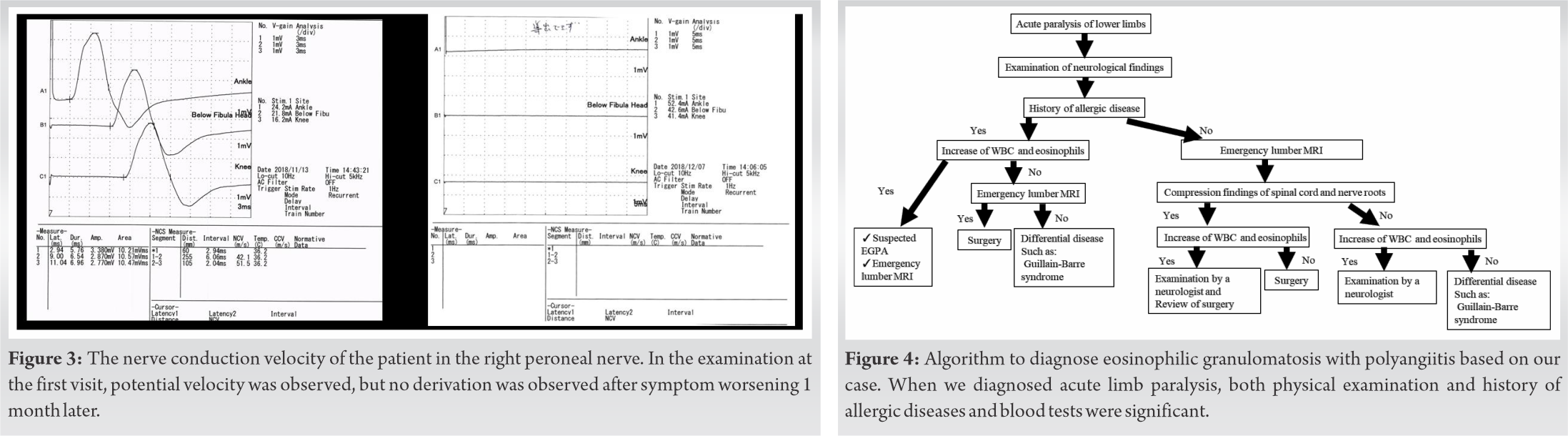
A 48-year-old woman presented with numbness and pain of her right lower extremity 2 days before her first visit. She visited our hospital because of worsening of pain. She was treated for asthma. On physical examination, we noted muscle weakness in the right lower extremity. On the manual muscle test (MMT), the tibialis anterior (TA) and extensor hallucis longus (EHL) were 3/5, and gastrocnemius and flexor hallucis longus (FHL) were 4/5. She denied low back pain. Straight leg raising (SLR) was positive at 70 degrees; however, the femoral nerve stretch test was negative. Deep tendon reflexes were normal. An X-ray revealed degenerative scoliosis at L5–S1 (Fig. 1). Magnetic resonance imaging (MRI) revealed a disc herniation at L5–S1, but there was no significant nerve root compression or cord compression (Fig. 2). Nerve conduction velocity testing in the peroneal nerve revealed that the motor nerve conduction velocity was 51.5 m/s (Fig. 3). When the ankle brachial index was measured to evaluate vascular lesions, a decrease of 0.78 on the right and 0.73 on the left was observed (reference value: 0.91–1.40). Considering the possibility of peripheral arterial disease of the lower extremities, we performed arteriography of the lower extremities but found no significant vascular lesions. Based on these results, the initial diagnosis was LDH and we initiated symptomatic treatment using only an extract from inflamed rabbit skin inoculated with vaccinia virus (Neurotropin®).

On the 7th day after the first visit to our hospital, her muscle strength appeared to recover, and on the 10th day, MMT in the right lower limb recovered to almost normal (Table 1). Because the pain remained from the lateral side of the right lower leg to the dorsum of the foot, symptomatic treatment was continued. On the 22nd day after the first visit, the pain in the right lower leg worsened, and on the 26th day, right drop foot was observed. MMT on the right side of TA, EHL, FHL, and peroneus longus were 1/5, and the left side TA, EHL, and FHL were 4/5 (Table 1). The Achilles tendon reflex disappeared on both sides. MRI was performed urgently; however, no exacerbation of LDH was observed. The peroneal nerve conduction velocity test failed to derive an evoked myogenic potential (Fig. 3). Subsequently, she was unable to walk and was hospitalized on the 30th day after the first visit.
Blood tests on admission showed eosinophilia (white blood cell 40,300/μL, eosinophil percentage 77% and IgE 1120 IU/ml), associated with mild liver dysfunction and increase of CPK levels (Table 2). When we referred her to the neurology department, she was diagnosed with polyneuritis in the context of EGPA. Administration of 10 mg/day of steroid was started. The dose was gradually increased to 20 mg/day on the 3rd day after hospitalization and 30 mg/day after 1 week. Blood tests 1 week after admission showed a decrease in eosinophil fraction and improved liver function tests (Table 2). Perinuclear-antineutrophil cytoplasmic antibody (ANCA) and cytoplasmic-ANCA that is specific for ANCA-related vasculitis were negative. Steroid pulse therapy (1000 mg/day) was administered 2 weeks after hospitalization because the neurological symptoms of the lower extremities were not improved. Thereafter, she continued to take steroids at a maintenance dose of 50 mg/day; however, the numbness of both hands and feet and muscle weakness remained. One month after hospitalization, she was readmitted to the other hospital for detailed examination and treatment. At the time of transfer, the MMT was 0/5 below the TA on the right lower extremity and 2–3/5 below the TA on the left lower extremity (Table 1). In the upper extremity, interosseous muscle and abductor digiti minimi were 4/5. After discharge from the department of neurology, rehabilitation was performed at our department. Six months after the onset of symptoms, she could walk with a right short leg brace, and MMT recovered to 1–3/5 below the TA on the right lower limb and 4–5/5 below the TA on the left lower limb (Table 1).
In 1951, Churg and Strauss first described a syndrome characterized by asthma and symptoms of cardiac failure, renal damage, and peripheral neuropathy resulting from vascular embarrassment in various systems of organs [7]. Allergic symptoms such as asthma and allergic rhinitis occur simultaneously with vasculitis, and inflammation of the blood vessels occurs due to the invasion of neutrophils and eosinophils [1]. This disease had been known as Churg–Strauss syndrome and this entity was renamed and recognized as EGPA at the 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides [8]. EGPA has three stages. Stage I is atopic asthma and rhinitis that are usually difficult to control for decades. In Stage II, eosinophil infiltration is seen in various organs, including the lungs and the gastrointestinal tract. In Stage III, systemic vasculitis is observed with general symptoms including skin lesions, peripheral neuropathy, fever, body weight loss, kidney disorder, or mononeuropathy multiplex [9]. In our case, the patient was being treated for asthma. We observed a marked increase in the eosinophil fraction and peripheral neuropathy associated with vasculitis. Therefore, the patient was in Stage III of EGPA. Neuritis of EGPA causes pain in the affected leg that is similar to symptoms of radiculopathy such as LDH or strangulated peripheral neuropathy [5]. Mononeuropathy multiplex is observed in 50–78% of EGPA patients [4,6]. It was reported that the frequency of individual nerve involvement, as judged by sensory impairment, was highest in the peroneal nerves [6]. In our case, the SLR test was positive and LDH was suspected with MRI findings at the first visit. Subsequently, peroneal nerve conduction tests did not reveal derivation, suggesting peroneal nerve palsy. If there was a history of asthma and atypical neurological findings, EGPA was considered in the differential diagnosis and blood tests were considered necessary. Treatments of EGPA usually include steroids. To improve the prognosis of EGPA neuropathy, early high-dose steroid treatment is essential [4,6]. Effective treatment of EGPA requires suppression of the immune system. The treatment duration is prolonged with induction of remission, followed by maintenance treatment, sometimes lasting 12–18 months or longer [10]. Fortunately, our patient began treatment before life-threatening organ invasion and responded well to medical therapy. No complications occurred. Nevertheless, improvement of muscle strength was not achieved. This caused delays of diagnosis and treatment of steroid. These findings support the notion that delayed diagnosis and delayed treatment with steroids influences the result of treatment. As a diagnostic algorithm for EGPA, Nagata et al. [9] reported that it was necessary to perform emergency MRI when patients with asthma or eosinophilic pneumonia develop a sudden lower limb paralysis. Emergency surgery was given priority when the subarachnoid space is found to be severely compromised. If there is no exclusion of the subarachnoid space on MRI and blood tests reveal increased eosinophil fraction, EGPA, and neurology referral should be considered. If there was no increase of eosinophil fraction, one should suspect vasculitis and proceed with the appropriate work-up. EGPA is a very rare disease. However, when it is suspected, a work-up should ensue according to the algorithm that was considered in our case (Fig. 4).
EGPA is difficult to diagnose. In our case, the symptoms worsened on the 30th day after the initial visit. She was diagnosed with EGPA by a blood test at the time of admission. If patients with bronchial asthma or a history of allergies develop lumbar radiculopathy or peroneal nerve palsy-like symptoms, EGPA should be considered and steroid treatment should be initiated early.
EGPA is sometimes misdiagnosed as LDH or LSS. When orthopedic surgeons encounter patients who complain of numbness and pain of their lower extremity and who have medical histories of asthma or eosinophilic pneumonia, EGPA should be considered and steroid treatment should be initiated early.
References
- 1.Lanham JG, Elkon KB, Pusey CD, Hughes GR. Systemic vasculitis with asthma and eosinophilia: A clinical approach to the Churg-Strauss syndrome. Medicine (Baltimore) 1984;63:65-81. [Google Scholar | PubMed]
- 2.Sehgal M, Swanson JW, DeRemee RA, Colby TV. Neurologic manifestations of Churg-Strauss syndrome. Mayo Clin Proc 1995;70:337-41. [Google Scholar | PubMed]
- 3.Siemińska A. Churg-Strauss syndrome-a rare disease or a difficult diagnosis? Pneumonol Alergol Pol 2012;80:3-5. [Google Scholar | PubMed]
- 4.Nakamura M, Yabe I, Yaguchi H, Kishimoto R, Mito Y, Fujiki N, et al. Clinical characterization and successful treatment of 6 patients with Churg-Strauss syndrome-associated neuropathy. Clin Neurol Neurosurg 2009;111:683-7. [Google Scholar | PubMed]
- 5.Lozeron P, Lacroix C, Michon M, Theaudin M, Lacour MC, Denier C, et al. Vasculitis neuropathy mimicking lower limb mono-radiculopathy: A study and follow-up of 8 cases. Intern Emerg Med 2013;8:601-9. [Google Scholar | PubMed]
- 6.Hattori N, Ichimura M, Nagamatsu M, Li M, Yamamoto K, Kumazawa K, et al. Clinicopathological features of Churg-Strauss syndrome-associated neuropathy. Brain 1999;122:427-39. [Google Scholar | PubMed]
- 7.Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol 1951;27:277-301. [Google Scholar | PubMed]
- 8.Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 Revised international Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum 2013;65:1-11. [Google Scholar | PubMed]
- 9.Nagata K, Yamamoto S, Miyoshi K, Sato M, Arino Y, Mikami Y. A diagnostic algorithm for eosinophilic granulomatosis with polyangiitis initially diagnosed as lumbar disc hernia or lumbar spinal stenosis: Personal experience and review of the literature. Acta Med Okayama 2016;70:261-8. [Google Scholar | PubMed]
- 10.Ghosh S, Bhattacharya M, Dhar S. Churg-Strauss syndrome. Indian J Dermatol 2011;6:718-21. [Google Scholar | PubMed]