Symptomatic Aggressive vertebral haemangiomas require thorough decompression and regular fol-lowup to avoid catastrophic complications due to recurrence.
Dr. Raja Ganesh,
Junior Resident, Department of Orthopaedics,
D.Y. Patil Hospital and Research Centre, Navi Mumbai, Maharashtra, India.
E-mail: drrohangala17@gmail.com
Introduction: Vertebral hemangiomas although benign vascular lesions few of these may be ag-gressive causing osseous, extra-osseous and/or epidural expansions with recurrence rate as low as 3%. It should be considered as one of the important differentials while dealing with lytic lesions in the dorsal spine causing compressive myelopathy.
Case Report: A 16-year-old female came with an acute history of paraparesis with bladder in-volvement. She was diagnosed of vertebral hemangioma of D9 for which she underwent surgical decompression and fixation. At present, she had paraparesis with a sensory level of D10 on exami-nation. After radiological investigations (X-ray and MRI) she had high intensity signals in the extra osseous portion of D9 with significant neural compression indicating recurrence of vertebral he-mangioma. She underwent decompression with long segment instrumentation with prior arterial embolization. Histopathology features were suggestive of hemangioma and our diagnosis of recur-rence was confirmed. At 2 weeks, the patient had improved neurology with partial sensory recovery and Grade 2 power in the right lower limb and Grade 1 power in the left lower limb. Histopathology report confirmed the diagnosis of hemangioma indicating recurrence. At 6 months follow-up after aggressive rehabilitation, the patient was spastic and improved to Grade 3 power in the left lower limb and Grade 4 power in the right lower limb. The sphincteric control was also found to be fair at 1 year follow-up.
Discussion: Vertebral hemangiomas when causing progressive neurological deficit warrant surgical decompression. The choice of intervention depends on location and extent of the tumor. Due to their high vascularity, it is advisable for to preoperatively carry out arterial embolization.
Conclusion: Although commonly asymptomatic, vertebral hemangiomas may present as compressive myelopathy. Therefore, they should be detected early, intervened and followed up regularly to detect recurrence to prevent worsening of neurology and function.
Keywords: Vertebral body hemangioma, myelopathy, recurrence.
Vertebral hemangiomas are benign vascular bony lesions, comprised of thin-walled vessels which are surrounded by fat permeating the medullary cavity between bony trabeculae [1]. There has been a variable incidence reporting for vertebral hemangioma, with various publications reporting it to be between 10% and 27%, but only 0.9% and 1.2% are symptomatic [2, 3]. Few of these hemangiomas may be aggressive causing osseous, extra-osseous and/or epidural expansions with recurrence rate as low as 3%. If a patient complains of new-onset back pain along with thoracic myelopathy progression, then vertebral hemangioma should be considered as one of the differential diagnosis. It is not clearly known that whether vertebral hemangioma can actually lead to recurring myelopathy. Here is presenting an interesting case of recurrence with acute onset paraplegia in a post-operative case of D9 vertebral hemangioma young female.
A 16-year-old female came with mid backache since 3 months with bilateral lower limb weakness and urinary incontinence since 5 days. The backache was localized initially, gradually progressive aggravated since the past 5 days. The backache was not associated with any constitutional symptoms but the patient reported that the pain worsened at night. She noticed weakness while getting down the stairs 5 days ago and had difficulty in maintaining her balance while walking. Her symptoms rapidly progressed over 2 days and she was unable to walk without support with increased tightness in her lower limbs and also had urinary frequency and urge incontinence. She denies any history of trauma or fall. She gave a history of having undergone an surgical instrumented intervention in the mid back region for similar complaints 1 year ago. She does not report any history of trauma. She was brought on a wheel chair to our emergency department. On physical examination, the neurological examination of the upper limb along with the higher motor functions was found to be normal. The lower limbs were found to be spastic. Power in both the lower limbs was found to be 1/5. There was impairment in the touch and the pain sensations as well. Sensory level was found to be D10. The X-ray done of 1 year back was suggestive of the corrective measures taken for ver-tebral hemangioma (Fig. 1). The patient was then subjected to magnetic resonance imaging (MRI). The axial and the sagittal T2 images of the MRI had high intensity signals in the extra osseous portion of D9 compressing the cord, indicating of vertebral hemangioma. This lesion was causing spinal cord compression, ultimately leading to acute onset paraplegia (Fig. 2).

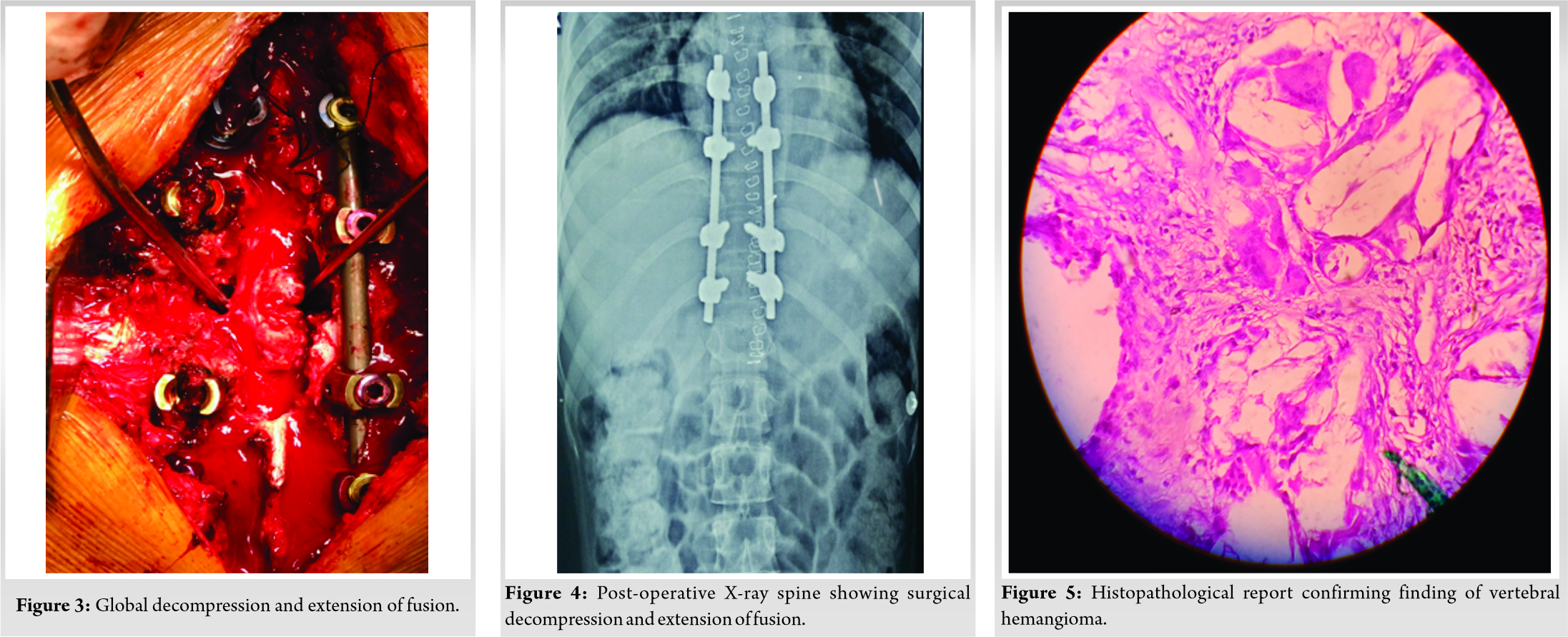
The decision was taken by the consulting orthopedic surgeons to manage the case with surgical intervention. The patient underwent arterial embolization 12 h before surgery. Decompression with long segment instrumentation was performed (Fig. 3, 4). On the 14th post-operative day, the patient had improved neurology with complete sensory recovery and Grade 2 power in right lower limb and Grade 1 power in the left lower limb. Histopathology report confirmed the findings correlating with that of hemangioma (Fig. 5). At 6-month follow-up after aggressive rehabilitation, the neurology of the patient improves to Grade 3 power in the left lower limb and Grade 4 power in the right lower limb. However, the spasticity persisted but was reduced. The sphincteric control was also found to be fair at 6-month follow-up.
Although majority of the vertebral hemangiomas are asymptomatic according to published literature, some of the cases have been reported to cause cord compression along with neurologic clinical features. Such symptomatic vertebral hemangiomas are found to be mainly in the thoracic region. This type of aggressive vertebral hemangioma is seen in about 1–2% of cases [4, 5]. The sympto-matic vertebral hemangiomas have been found to be hypervascular, while the epidemiological pre-dilection being young females, just like our case. Embolization has been stated as the only required therapeutic modality for vertebral hemangioma leading to spinal compression by Jayakumar et al. [6]. However, some studies have found that the neurological symptoms did not improve if embolization was the only modality used to manage compressive vertebral hemangioma. Fox and Onofrio [7] stated that vertebral hemangioma presenting with progressive neurologic deficit warrant surgical decompression. The surgical interventions include tumor excision, laminectomy or corpectomy and en-bloc resection as well as reconstruction. The choice of surgical intervention varies depending over the location as well as the tumor extent [8]. However, care should be taken for intra-operative bleed, which is prevented by arterial embolization. Bremnes et al. [9] suggested radiotherapy after surgery to lead to complete tumor regression in some cases. However, Faria et al. [10] showed that some of the patients may also show malignant transformation after repetitive irradiation.
In this case, there was a recurrence of the vertebral hemangioma, giving rise to debilitating paraplegia. Hence, it is important for the patient to undergo urgent decompression and stabilization. This procedure must be done with prior arterial embolization to prevent intraoperative bleeding and re-duces surgical morbidity.
Vertebral hemangiomas should be considered as one of the important differentials while diagnosing lytic lesions in the dorsal spine. Aggressive hemangiomas which undergo surgical intervention should be regularly followed up so that their recurrence can be picked up early and they can be appropriately managed.
Management of aggressive vertebral heamangiomas is based on its clinical presentation. Pre operative arterial embolisation aids in surgery by reducing the blood loss of this highly vascular tumour. Although aggressive hemangiomas presenting with myelopathy have a satisfactory prognosis if treated with early surgery, a regular and close followup is needed to rule out recurrence. Radiotherapy is a good adjuvant in selected cases.
References
- 1.Mulliken JB, Glowacki J. Classification of pediatric vascular lesions. Plast Reconstr Surg 1982;70:120-1. [Google Scholar]
- 2.Barzin M, Maleki I. Incidence of vertebral hemangioma on spinal magnetic resonance imag-ing in Northern Iran. Pak J Biol Sci 2009;12:542-44. [Google Scholar]
- 3.Aich RK, Deb AR, Banerjee A, Karim R, Gupta P. Symptomatic vertebral hemangioma: Treatment with radiotherapy. J Cancer Res Ther 2010;6:199-203. [Google Scholar]
- 4.Alexander J, Meir A, Vrodos N, Yau YH. Vertebral hemangioma-an important differential in the evaluation of locally aggressive spinal lesions. Spine 2010;35:E917-20. [Google Scholar]
- 5.Laredo JD, Assouline E, Gelbert F, Wybier M, Merland JJ, Tubiana JM. Vertebral heman-giomas: Fat content as a sign of aggressiveness. Radiology 1990;177:467-72. [Google Scholar]
- 6.Jayakumar PN, Vasudev MK, Srikanth SG. Symptomatic vertebral haemangioma: Endovas-cular treatment of 12 patients. Spinal Cord 1997;35:624-8. [Google Scholar]
- 7.Fox MW, Onofrio BM. The natural history and management of symptomatic and asympto-matic vertebral haemangiomas. J Neurosurg 1993;78:36-45. [Google Scholar]
- 8.Shah KC, Chacko AG. Extensive vertebral haemangioma with cord compression in two pa-tients: Review of the literature. Br J Neurosurg 2004;18:250-2. [Google Scholar]
- 9.Bremnes RM, Hauge HN, Sagsveen R. Radiotherapy in the treatment of symptomatic verte-bral hemangiomas: Technical case report. Neurosurgery 1996;39:1054-58. [Google Scholar]
- 10.Faria SL, Schlupp WR, Chiminazzo H. Radiotherapy in the treatment of vertebral hemangi-omas. Int J Radiat Oncol Bio Phys 1985;11:387-90. [Google Scholar]










