In the presence of stable joint after reduction, it is possible to achieve satisfied clinical results with early rehabilitation.
Dr. Ozcan Kaya,
Istanbul Training and Research Hospital,
Orthopedics and Traumatology Kasap İlyas Mah, Org.
Abdurrahman Nafiz Gürman Cd., 34098 Fatih/İstanbul.
E-mail: ozcankaya.md@gmail.com
Introduction:Ulnar volar dislocation (UVD) is a very rare entity. Due to rarity of condition, usually, it’s misdiagnosed at emergency departments and management of this clinical entity is not well studied. Here, we report a case of UVD impressing diagnostic challenge, indication of treatment, and follow-up.
Case Report: A 29-year-old man presented to orthopedic outpatient service with complaining of the right wrist pain. He had an assault history 3 days before. In the emergency department, he had been diagnosed as wrist sprain. Splint and pain killers were prescribed. Due to increase of pain, he admitted to orthopedics. He was diagnosed UVD. Under general anesthesia, joint was reduced with forced pronation maneuver. After 3 weeks immobilization period, magnetic resonance images revealed partial injury of triangular fibrocartilage complex then splint removed and rehabilitation initiated. Over than 24 months, he is doing well without movement limitation and wrist strength impairment.
Conclusion: For prevention misdiagnosis of UVD, physical examination is very important. Forearm rotation limitation with pain in the wrist should be indicative for distal radioulnar joint injury. Physical examination should be supported with proper evaluation of suitable radiographs. After reduction of joint, magnetic resonance images give clues about ligamentous injury. Our case supports the importance of rigorous physical examination and evaluation of radiographs for wrist injury. In the presence of partial injury of ligaments, the condition can be treated with shorter periods of immobilization and early rehabilitation.
Keywords: Wrist pain, ulnar volar dislocation, distal radioulnar joint, forearm rotation.
Dorsal dislocation of the ulnar head at the distal radioulnar joint (DRUJ) commonly coexists with forearm fractures and has been well studied [1]. On the other hand, ulnar volar dislocation (UVD) is a very rare condition, with literature knowledge consisting of only case reports. Since UVD is a very rare traumatic event, the literature information is only about case reports. Therefore, there is no incidence information about this injury. Misdiagnosis of UVD is not uncommon because of the rarity of injury with subtle clinical findings and inadequate evaluation of radiographs in emergency settings [2]. Disruption of the stabilizers of DRUJ (ulnar collateral ligament, triangular fibrocartilage discus, anterior and posterior radioulnar ligaments, and pronator quadrates [Pqs]) due to hypersupination of the forearm at the wrist or direct trauma to the DRUJ in a posterior to anterior direction may cause UVD [3]. The most prominent clinical findings of UVD are wrist pain and limited forearm rotation. Treatment options vary from closed reduction with immobilization in a pronated position 4–6 weeks to open reduction and repair of DRUJ stabilizers in cases of locked irreducible UVD. Open reduction and repair of stabilizer structures are generally preferred in cases that are unstable after closed reduction and in cases that cannot be reduced as closed [4]. We herein present a missed UVD where the ulnar head was stuck to the sigmoid notch and treated by closed reduction and immobilization. The patient is doing well at 24 months follow-up. There are no established guidelines for management due to the rarity of the injury. The case is presented along with a review of the pertinent literature.
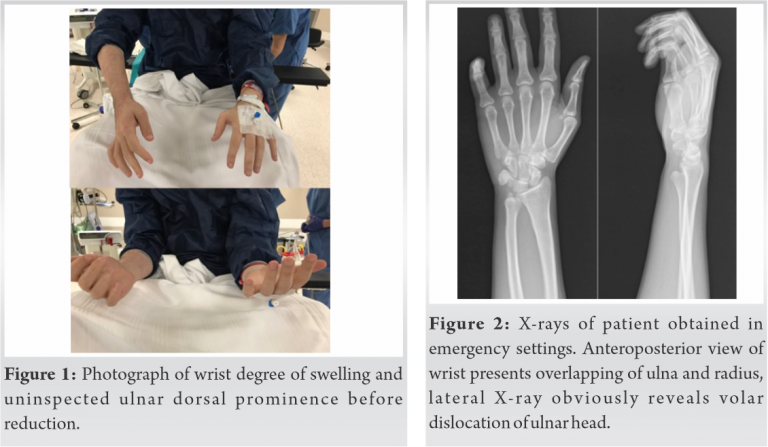
A 29-year-old man presented to the orthopedics department with progressive right wrist pain. He sustained a blunt injury caused by assault 3 days ago and initially evaluated in the emergency department. Radiographs of the wrist were obtained, and he was diagnosed with wrist sprain. He was prescribed with nonsteroidal anti-inflammatory and muscle relaxants drugs, and a volar short arm splint was applied. He was referred to the orthopedics clinics when his pain did not respond to treatment. The splint was removed, and inspection showed wrist edema along with loss of the dorsal ulnar styloid prominence (Fig. 1).
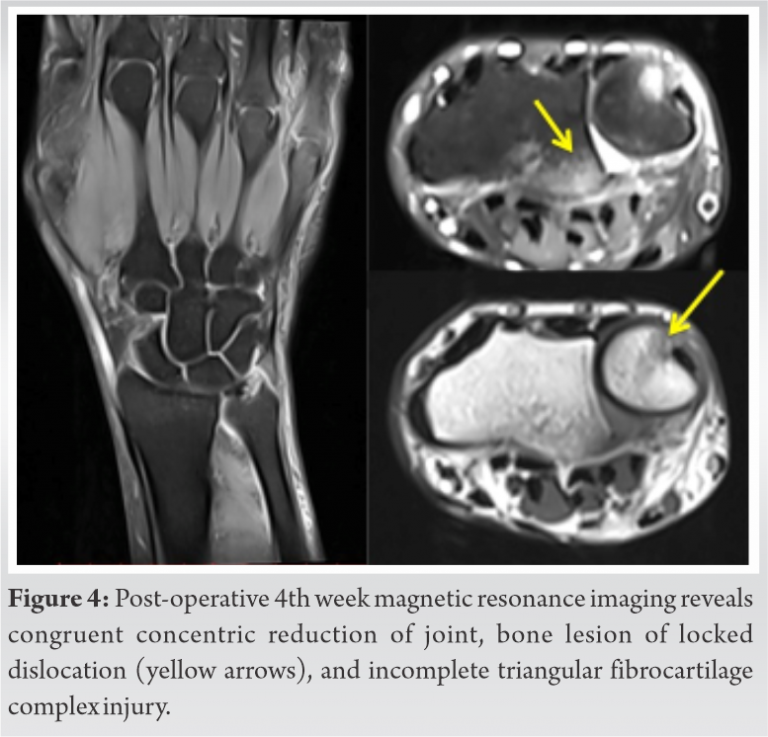
The wrist was tender to palpation, and the ulnar styloid process was not palpable at the dorsal aspect of the joint. He had mildly limited dorsiflexion and palmar flexion, and no forearm rotation. His previous X-rays, obtained 3 days ago in the emergency department, revealed an obvious UVD (Fig. 2). Closed reduction was attempted under local anesthesia, however failed due to extreme pain. A computerized tomography (CT) was taken for possible locked dislocation. Axial views and volume-rendered images of the DRUJ revealed volar dislocation of the ulnar head engaged with the sigmoid notch (Fig. 3).
The patient was taken to the operating room and under general anesthesia, the ulnar head was reduced by forceful pronation. The DRUJ was stable during passive forearm rotation. A long arm cast was applied with the forearm in semi-prone position and kept for 3 weeks. Magnetic resonance imaging (MRI) was obtained to inspect possible injuries to the stabilizing soft tissues and showed incomplete triangular fibrocartilage complex (TFCC) tear and bone impaction injury caused by engagement of the ulnar head to the sigmoid notch (Fig. 4). The cast was removed at the 3 weeks, and rehabilitation was initiated. The 3-stage wrist rehabilitation program was prescribed for the patient: Progression to each stage was guided by pain response. The stages of rehabilitation were described as pain control and ROM, regaining wrist stability with ROM, axial loading on the wrist and neuromuscular control. The patient performed isometric strengthening of the DRUJ stabilizers, PQ, and extensor carpi ulnaris (ECU). Isometric exercises were applied to the ECU and PQ muscles. Once the patient was able to complete two sets of 10 repetitions of isotonic strengthening exercises without significant increase in pain, a variety of balance, weight-bearing, and coordination activities was performed. After 3 weeks, he reached full range of forearm supination and pronation without pain. At the last follow-up, more than 24 months after closed reduction, he was doing well without any pain or limitations in range of motion (Fig. 5). Since the hospital outpatient service visits were limited due to the COVID-19 pandemic, the patient evaluated with a quick dash score (0) through online interview.
UVD is very rare compared to dorsal dislocation, and the medical literature is composed of only case reports. The lack of any case series has been published, makes it difficult to construct a treatment algorithm [5]. The injury mechanism differs between patients and treatment techniques vary according to surgeon preference. The anatomic features of the ulnar head and the radial notch allow the ulnar head to translocate during rotation of forearm at the DRUJ, where the ulnar head translates slightly volar in supination. Hypersupination injury, which is usually seen during a fight, is the most accused mechanism for UVD due to the anatomic features of DRUJ. Direct trauma to the DRUJ from posterior to anterior is also thought to be another mechanism of the injury. Our patient was attacked, and his forearm was forced to hypersupinate [4]. Disruption of the static (TFCC, interosseous membrane, and radioulnar ligament) and dynamic (ECU muscle and PQ muscle) stabilizer structures by trauma may lead to their entrapment, impeding reduction of the joint. TFCC is the most important stabilizer, and UVD is believed to coexist with TFCC tear or ulnar styloid fracture [6]. Even a partial TFCC injury may cause DRUJ instability, as presented in our case. Unfortunately, misdiagnosis rates for this injury are very high. It is estimated that 50% of cases are misdiagnosed due to subtle clinical findings and inadequate evaluation of radiographs in the emergency. Detailed physical examination, simply including assessment of forearm rotations, and obtaining true lateral X-rays, enables a correct diagnosis. CT may be helpful in confirming the diagnosis, and when reduction is not possible, it may provide additional information such as engagement of the ulnar head to the radial notch with osteochondral impaction fracture, similar to a Hill-Sachs lesion (Fig. 2). MRI, as presented here, gives further information including the presence of impaction, potential soft-tissue injuries, and interpositions (TFCC, tendons, and radioulnar ligaments) which may help to determine the appropriate management [2, 7]. In our patient, the MRI showed impaction injury of the ulnar head and radial notch with a partial TFCC tear which did not require additional intervention, and a congruent joint without any interposition of soft tissues with concentric reduction. Management of UVD is generally often differs between reports due to lack of a well-defined treatment algorithm. The first step for the treatment has been closed reduction with extreme pronation, and immobilization with the forearm in a neutral or semi-pronated position. Previous reports recommend immobilization for 6–8 weeks for all dislocations and in the prone position specifically for volar dislocations [8]. This duration is usually justified by the healing time of the TFCC and interosseous membrane. Closed reduction has yielded good results even in chronic injuries (>3 weeks). The authors advice assessment of forearm rotations after reduction. In the presence of instability, transfixation of DRUJ is be crucial for DRUJ stability until the capsule and the soft tissues healed. Possible limitation in range of motion, caused by prolonged transfixation of the DRUJ, seems to be a disadvantage for transfixation. In the presented paper, after reduction under general anesthesia, we evaluated the stability of the joint with rotations of forearm and applied cast in a semi-pronated position for 3 weeks to start the rehabilitation earlier. MRI revealed some degree of soft-tissue injury, but wrist pain resolved with excellent functional results with early rehabilitation. According to some authors, surgical intervention becomes essential in case of failed closed reduction and residual instability, which are mostly caused by capsuloligamentous or TFCC interposition [9]. Besides these indications, locked and irreducible UVD may be caused by the compressive pull of major dynamic stabilizer PQ and impaction of the ulnar head at the notch, which would require surgical management [7]. On the other hand, there are authors advocating repair of capsular ligaments and TFCC irrespective of whether closed or open reduction is performed, especially in young patients [10].
UVD is a very rare injury. Traumatic wrist pain should be evaluated rigorously and with truly obtained X-rays, and physical examination including rotations of the forearm for prevention of misdiagnosis in the emergency department. CT and MRI reveal more about injury when compared to X-rays in terms of soft-tissue injury and DRUJ anatomy. Even incomplete TFCC lesions may cause DRUJ instability, as in the presented case. Closed reduction is usually curative with the support of muscle relaxant effect of general anesthesia even in bone impacted locked dislocations. A stable DRUJ with preserved stabilizing tissues may provide favorable results without prolonged immobilization after closed reduction and early initiation of rehabilitation. For the exact management algorithm of the injury, higher number of case series is necessary.
UVD can be detected easily with rigorous physical examination and X-ray evaluation. At the emergency department, forearm rotations should be evaluated in patients with a painful wrist. Early physical rehabilitation can be initiated when reduction is stable even if in the presence of partial thickness soft-tissue stabilizers of drug. Our case also shows the efficacy of non-surgical treatment in stable injuries after reduction, like most of the cases previously reported on this subject.
References
- 1.Tsismenakis T, Tornetta P 3rd. Galeazzi fractures: Is DRUJ instability predicted by current guidelines? Injury 2016;47:1472-7. [Google Scholar]
- 2.Kumar A, Iqbal MJ. Missed isolated volar dislocation of distal radio-ulnar joint: A case report. J Emerg Med 1999;17:873-5. [Google Scholar]
- 3.Sonohata M, Mine H, Tsuruta T, Mawatari M. Traumatic volar dislocation of the distal ulna with a fracture of the ulnar styloid. Hand Surg 2012;17:383-6. [Google Scholar]
- 4.Bouri F, Fuad M, Abdolenour AE. Locked volar distal radioulnar joint dislocation. Int J Surg Case Rep 2016;22:12-4. [Google Scholar]
- 5.Werthel JD, Masmejean E, Silvera J, Boyer P, Schlur C. Acute isolated volar dislocation of the distal radio-ulnar joint: Case report and literature review. Chir Main 2014;33:364-9. [Google Scholar]
- 6.Gofton WT, Gordon KD, Dunning CE, Johnson JA, King GJ. Soft-tissue stabilizers of the distal radioulnar joint: An in vitro kinematic study. J Hand Surg Am 2004;29:423-31. [Google Scholar]
- 7.Slattery D, Gohil S, Hogan G. A case report and the literature review: Volar dislocation of the DRUJ and stabilization using mini-suture anchors. Eur J Orthop Surg Traumatol 2013;23 Suppl 2:S203-5. [Google Scholar]
- 8.Larrivée S, Matthewson G, Barron L. Closed reduction of an acute volar dislocation of the distal radio-ulnar joint by a modified technique. Case Rep Orthop 2018;2018:4289406. [Google Scholar]
- 9.Giangarra CG, Chandler RW. Case report complex volar distal radioulnar joint dislocation occurring in a Galeazzi fracture. J Orthop Trauma 1989;3:76-9. [Google Scholar]
- 10.Kashyap S, Fein L. Surgical correction of recurrent volar dislocation of the distal radioulnar joint. Clin Orthop 1991;266:85-9. [Google Scholar]