Because life-threatening injuries in pregnancy are rare, trauma care for pregnant women remains an exceptional situation for which interdisciplinary, Advanced Trauma Life Support-guided trauma management is absolutely essential.
Dr. med. Jason-Alexander Hörauf,
Department of Trauma,
Hand and Reconstructive Surgery, Hospital of the Goethe-University Frankfurt/Main,
Theodor – Stern – Kai 7. D – 60590 Frankfurt/Main.
E-mail: jason-alexander.hoerauf@kgu.de
Introduction: Major trauma is the leading non-pregnancy-related cause of maternal and fetal deaths. In particular, traffic accidents account for the majority of accident causes and present the highest mortality for the mother and fetus. Seat belt use has reduced mortality rates for both the mother and the unborn child, however, certain potential patterns of injury occur due to the restraining mechanical forces of the worn seat belts on the body. Since life-threatening injuries in pregnancy are nevertheless rare, trauma care of pregnant women continues to be an exceptional situation and a particularly stressful situation for the attending physicians, including the fact that two lives are potentially at stake.
Case Report: In this article, we report on a patient in the 37th week of pregnancy who was involved in a high-speed trauma as a front passenger of a car. Initially awake as well as responsive and hemodynamically stable, the patient’s condition deteriorated on the way to the emergency room (ER). On arrival in the ER, according to the Advanced Trauma Life Support concept, interdisciplinary consensus had to be reached between the departments involved regarding further diagnostic and therapeutic procedures. With the knowledge of the special anatomical and physiological changes in the context of pregnancy, both the mother and the child could be stabilized in order to subsequently gain further important information about the present injury pattern during the performed diagnostics and finally to be able to adequately treat the trauma sequelae.
Conclusion: Because the care of traumatic life-threatening injuries in pregnancy is rare overall, it poses a special challenge for the attending trauma team in the ER. In order to avert the fatal fate of both the mother and the unborn child, a structured, symptom and patient-oriented interdisciplinary approach is indispensable, especially in these exceptional situations, in order to achieve the best possible outcome for those affected.
Keywords: Trauma, advanced trauma life support, motor vehicle accident, pregnancy.
In 2013, 54 million people worldwide sustained injuries from motor vehicle accidents (MVAs), leading to approximately 1.2 million deaths on the worlds roads every year [1]. Hereby, pregnant women represent a special subgroup of MVA-related casualties. In the United States of America, about 130,000 women being in late pregnancy are involved in traffic accidents every year, in which MVAs are the leading cause of fetal deaths related to maternal trauma [2].
Through the (legal) implementation of supplemental restraint systems such as the usage of seatbelts or airbags, MVA-associated case fatality and mortality significantly decreased [3]. Nevertheless, the use of safety belts in MVAs, due to the restraining mechanical forces acting on the body, is associated with the development of certain injury patterns. Leading injuries are intraabdominal injuries, but thoracic injuries and bony injuries are also common [4]. In addition, the correct wearing of seat belts is of particular importance in the group of pregnant accident victims, as a lack of proper seat belt use is associated with a higher risk of adverse fetal outcome in MVAs [2].
Here, we present a pregnant woman involved as a restrained front-seat passenger in a MVA suffering from multiple trauma.
A 33-year-old woman in the 37th week of pregnancy, with no previous medical or surgical history, presented to the emergency room (ER) of our emergency department after being involved in a MVA. She was a front-seat passenger wearing a seatbelt. Since the front apron was clearly deformed, a high-speed trauma can be assumed. At the scene of the accident, the patient was awake and oriented and presented with stable vital parameters to the paramedics. Apart from neck pain, the patient did not express any other complaints. By the time of alerting the emergency ward personnel, the on call obstetricians were informed to prepare for emergency cesarian section in the ER setting. On arrival of the patient, the following specialists were in the ER: two trauma surgeons, two anesthesiologists, one intensive care pediatrician, two obstetrician, two general surgeons, and one radiologist.
The patient’s state of health deteriorated during the transfer to our emergency department. On presentation, she was somnolent and hemodynamically unstable with hypotension (80/50 mmHg) and tachycardia (150 bpm). During the first survey, an abdominal seat belt sign was detected, and Focused Assessment with Sonography for Trauma (FAST) showed free fluids in the Morrison pouch and an inhomogeneity of the spleen. The sonographic imaging of the unborn child performed by the obstetric colleagues showed significant bradycardia at about 100 bpm. After changing the patient’s position to the left side to reduce pressure on the maternal caval vein, the fetal heart rate stabilized to normal values around 140 bpm.
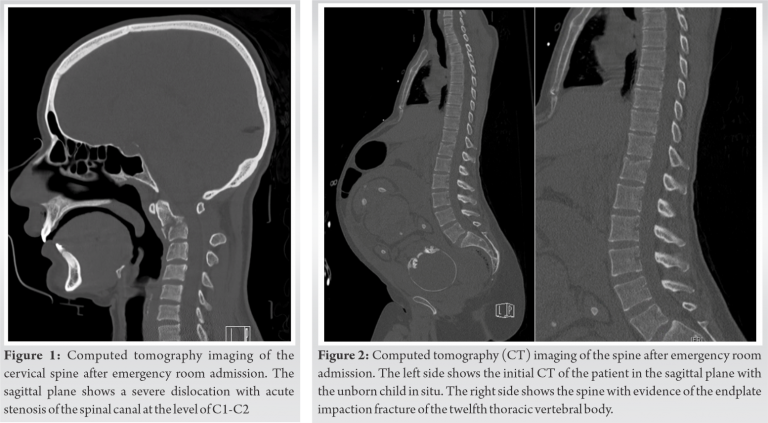
After stabilization of the patient’s circulation by administration of crystalloid fluids and catecholamines, the interdisciplinary decision to perform a whole-body computed tomography (WB-CT) without contrast medium was made. WB-CT showed a dislocated, unstable fracture of the second cervical vertebral body (type III according to Anderson and D’Alonzo [5], Fig. 1), a non-dislocated sternal fracture with serial rib fractures of costae 3–5 on the right and costae 7–12 on the left side without evidence of a pneumothorax. In addition, a splenic laceration and the suspicion of a liver laceration as well as an endplate impaction fracture (type A1.1 according to AO-classification [6]) of the twelfth thoracic vertebral body (Fig. 2).
After completion of the imaging, the patient was taken to the operating room for emergency caesarean section performed by the colleagues of the obstetric department. About 40 min after arrival in our ER, a healthy girl was born. The surgical abdominal approach then was further extended into midline laparotomy by the general surgery team to address the spleen and liver lacerations. After exploration of the spleen, a central rupture was found that extended to the periphery of the upper pole (type IV according to Moore et al. [7]), which is why the spleen was completely removed in a situation of ongoing hemodynamic instability. In addition, a decapsulation of the liver on the left side with a diffuse hemorrhage (type II according to Moore et al. [7]) was observed, which was stopped by suturing. During surgery, there was a pronounced loss of blood, so that a mass transfusion of blood and coagulation products was necessary (Table 1).
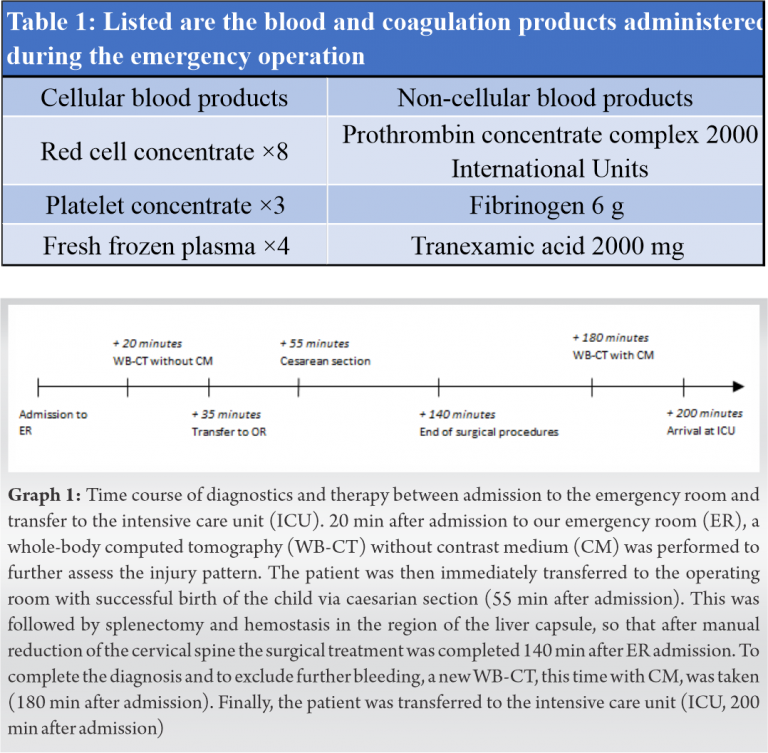
The cervical spine was reduced intraoperatively under image-intensifier control and afterwards immobilized again with a hard collar. The patient was then transferred again to WB-CT to re-evaluate the position of the cervical spine and to rule out active bleeding, this time with contrast medium. WB-CT showed no evidence of active bleeding. The position of the cervical spine was clearly improved after intraoperative reduction (Fig. 3), so that a further acute surgical intervention in the sense of damage control surgery was avoided. Subsequently, the patient was transferred to the intensive care unit (ICU) for further monitoring. In Fig. 4 the timeline of diagnostics and therapy between admission to the ER and transfer to the ICU is shown (Fig. 4).
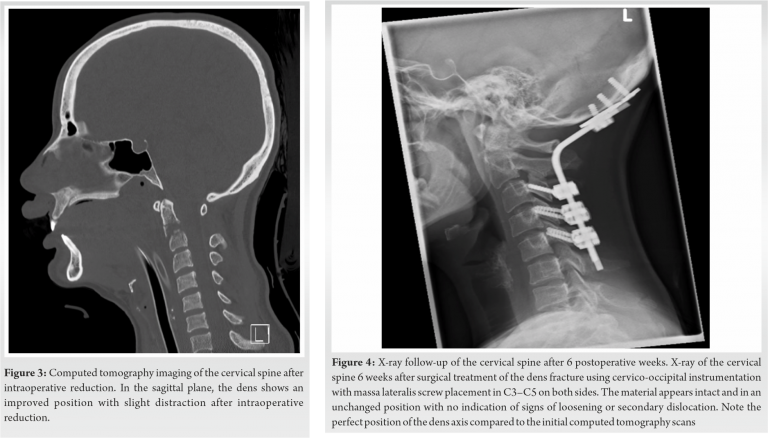
Four days later, the unstable fracture of the second cervical vertebra was surgically treated without any problems using cervico-occipital instrumentation of cervical vertebrae C3/4/5 to the occiput.
On the 7th day, the laboratory chemical infection parameters showed an increase, with febrile temperatures up to 39°C and impairment of oxygenation. In the performed X-ray of the thorax, the suspicion of an infiltrate in the left upper and lower lobe showed up most likely in the sense of a nosocomial pneumonia. Therefore the calculated postoperative antibiotic therapy was escalated. In addition, progressive pleural effusion was observed on the left side, so that a negative liquid balance was additionally attempted by means of loop diuretics. As a result of the measures initiated, the pulmonary infiltrates as well as the pleural effusion on the left side were regressive, so that the patient could be successfully extubated after about two weeks post-trauma and a few days later transferred to the intermediate care unit.
After extubation, a movement-dependent pain in the left knee was noticed, whereby the internal structures of the knee appeared intact during the physical examination. The imaging performed revealed a non-displaced depression fracture of the dorsolateral tibial plateau. Despite the existing fracture of the left tibial head, the physiotherapeutically guided mobilization on the walking frame improved daily, so that the patient could be discharged 3½ weeks after the trauma. During the follow-up in our outpatient department, X-ray control of the cervical spine after 6 postoperative weeks showed an anatomical reduction without signs of loosening or a secondary dislocation (Fig. 5), so that the Miami J cervical collar could be removed.
After admission to the ER, both mother and unborn child presented hemodynamically compromised. Therefore, according to the Advanced Trauma Life Support (ATLS) concept, in case of existing circulatory instability of either the mother or the unborn child, time-consuming diagnostics should have been omitted and upon sonographic evidence of intra-abdominal free fluid and the suspicion of splenic rupture, surgical treatment should have been performed promptly in the sense of the guiding principle “Treat first what kills first” [8]. In the supine position, especially in late pregnancy, the enlarged uterus may cause compression of the inferior vena cava, which in turn leads to interruption of venous return to the heart with a consecutive decrease in cardiac output [9]. Turning the patient onto the left side of the body resulted in sufficient decompression of the inferior vena cava, which resulted in a temporary improvement of the circulatory situation. Therefore, the interdisciplinary team decided to extend the diagnostics by a WB-CT scan, in particular, to focus on the cervical spine in case of preclinical complaints leading there. In order to save valuable time, additional contrast medium was not administered. Due to the severe and highly unstable cervical vertebral fracture shown on the CT, the subsequent intubation could be performed with special caution, in order to minimize cervical spine displacement and prevent further harm. In addition, the gain of image information allowed accurate reduction of the dislocated cervical vertebral fracture after successful completion of the surgical procedures.
MVAs account for approximately 60% of blunt trauma during pregnancy, with blunt abdominal trauma being the most common cause of maternal and fetal death [10]. Injuries to the spleen and liver are particularly prevalent because they are exposed closer to the thoracic wall by the expanded uterus, whereas injuries to intestinal organs are less prevalent, possibly because of the protection afforded by the enlarged uterus [11]. Free intra-abdominal fluid with a high suspicion of splenic rupture was already detected in the FAST performed in the ER. Goodwin et al. demonstrated a sensitivity of approximately 80% for the detection of free fluid in pregnant trauma patients [12], a rate comparable to that of non-pregnant trauma patients, which underlines the high importance of ultrasound diagnostics as a rapid, non-invasive and valuable tool in the assessment of pregnant trauma patients.
In addition to the severe splenic injury, the patient also suffered a critical injury of the cervical spine with an unusual fracture pattern, especially concerning the direction of dislocation. We found an unstable Anderson III situation with dislocation of C1 and dens axis in the anterior direction. With respect of the trauma history and direction of dislocation of C1 in relation to C2, hyperflexion of the cervical spine was probably the cause of the C2 fracture. The accompanying dislocations of the facet joints of C1 and C2 can possibly be explained, in addition to the flexion load, by an additional tensile stress that acts on the cervical spine during a frontal accident through the upper body restrained by the safety belt. McElhaney et al. reported that such loads can induce bilateral dislocations of the cervical facet joints [13]. During pregnancy, there is an increase in the laxity of the pelvic joints, and it is suggested that the hormone relaxin, which reaches its peak at the end of pregnancy, has a decisive impact therein [14]. An alteration in tensile strength of the ligamentous structures due to hormonal changes might be responsible for the unusual degree of dislocation of the facet joints of the cervical spine in this case. Additionally, the patient sustained a combination injury of an endplate impaction fracture of the 12th thoracic vertebral body and a non-displaced sternal fracture. Recently, Krinner et al. revealed that almost every third patient with a sternal fracture also has a bony injury to the spine, with this injury pattern occurring especially in MVAs [15]. In severe frontal collisions, the transmission of force from the upper part of the safety belt in the shoulder area to the torso can cause the curved thoracic spine to be stretched and thus generate axial compression with simultaneous flexion load, resulting in compression fractures or even burst fractures [16]. Here, flexion-compression forces of the upper thorax appear to act on the lower thorax (and vice versa), leading to the combined fractures of the sternum and spine. If the patient’s condition permits, relevant injuries to the axial skeleton should therefore be identified as part of the primary diagnosis in order to prevent further damage.
Even if the (correct) wearing of the seat belt can lead to specific injury consequences (see above) in the context of a high-energy traumas like MVA, wearing seat belts significantly reduces the maternal and fetal mortality rate [17]. However, pregnant women are less likely to wear a safety belt than non-pregnant women because of fears of (supposedly) harmful consequences, and this may be because improperly worn seat belts are associated with an increased rate of complications for the mother and unborn child [18]. It is assumed that adequate primary prophylaxis in the sense of patient education could prevent about half of all fetal losses in MVAs by the regular wearing of safety belts [2]. It is therefore necessary to provide pregnant women with information on the correct use of seat belts during early pregnancy in order to protect both the mother and the fetus.
After extubation, the patient complained of motion-dependent left knee pain. The radiographic imaging performed showed an initially missed non-displaced fracture of the tibial plateau. During high-energy traumas such as MVA, particularly axial forces are exerted on the tibial plateau, which can lead to compression fractures [19]. Injuries are more frequently missed in the periphery of the extremities, especially in unconscious/intubated or circulatory unstable patients [20]. This case demonstrates that a second or third survey is absolutely essential after the life-threatening injuries have been addressed.
Here, we report on a multiply injured pregnant woman who was involved in a MVA as a belted passenger. The patient suffered from life-threatening severe internal injuries and a pronounced fracture of the upper cervical spine. Optimal ER management under ATLS-conditions led to the best possible care including emergency cesarean section to save the child, emergency laparotomy and splenectomy to save the mother, with all procedures performed under cervical spine protection to prevent further harm. Furthermore, the present example illustrates that despite the steady improvement in road safety systems over the last decades, MVAs can be associated with a serious risk to the life and limb of road users. It is therefore all the more important that existing safety systems, such as the correct wearing of seat belts, are used strictly to prevent life-threatening injuries.
Since life-threatening injuries in pregnancy are rare, trauma care of pregnant women continues to be an exceptional situation and a particularly stressful situation for the attending physicians, because there are always two lives potentially at stake. Therefore interdisciplinary, ATLS-guided trauma management is essential for a favorable outcome.
References
- 1.Peden M. Global collaboration on road traffic injury prevention. Int J Inj Contr Saf Promot 2005;12:85-91. [Google Scholar]
- 2.Klinich KD, Flannagan CA, Rupp JD, Sochor M, Schneider LW, Pearlman MD. Fetal outcome in motor-vehicle crashes: Effects of crash characteristics and maternal restraint. Am J Obstet Gynecol 2008;198:450.e1-9. [Google Scholar]
- 3.Kwak BH, Ro YS, Shin SD, Song KJ, Kim YJ, Jang DB. Preventive effects of seat belt on clinical outcomes for road traffic injuries. J Korean Med Sci 2015;30:1881-8. [Google Scholar]
- 4.Masudi T, McMahon H, Scott J, Lockey A. Seat belt-related injuries: A surgical perspective. J Emerg Trauma Shock 2017;10:70-3. [Google Scholar]
- 5.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am 1974;56:1663-74. [Google Scholar]
- 6.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 1994;3:184-201. [Google Scholar]
- 7.Moore EE, Shackford SR, Pachter HL, McAninch JW, Browner BD, Champion HR, et al. Organ injury scaling: Spleen, liver, and kidney. J Trauma 1989;29:1664-6. [Google Scholar]
- 8.The ATLS Subcommittee, American College of Surgeons’ Committee on Trauma, International ATLS Working Group. Advanced trauma life support (ATLS®): The ninth edition. J Trauma Acute Care Surg 2013;74:1363-6. [Google Scholar]
- 9.Marx GF. Aortocaval compression syndrome: Its 50-year history. Int J Obstet Anesth 1992;1:60-4. [Google Scholar]
- 10.Mattox KL, Goetzl L. Trauma in pregnancy. Crit Care Med 2005;33 Suppl 10:S385-9. [Google Scholar]
- 11.Pearlman MD, Tintinalli JE, Lorenz RP. A prospective controlled study of outcome after trauma during pregnancy. Am J Obstet Gynecol 1990;162:1502-10. [Google Scholar]
- 12.Goodwin H, Holmes JF, Wisner DH. Abdominal ultrasound examination in pregnant blunt trauma patients. J Trauma 2001;50:689-93; discussion 694. [Google Scholar]
- 13.McElhaney JH, Nightingale RW, Winkelstein BA, Chancey VC, Myers BS. Biomechanical aspects of cervical trauma. In: Nahum AM, Melvin JW, editors. Accidental Injury. New York: Springer; 2002 [cited July 12, 2020]. Pp. 324-73. Available from: http://link.springer.com/10.1007/978-0-387-21787-1_15 [Google Scholar]
- 14.Vøllestad NK, Torjesen PA, Robinson HS. Association between the serum levels of relaxin and responses to the active straight leg raise test in pregnancy. Man Ther 2012;17:225-30. [Google Scholar]
- 15.Krinner S, Schmitt S, Grupp S, Hennig FF, Langenbach A, Schulz-Drost S. Häufigkeit und altersverteilung sternovertebraler kombinationsverletzungen: Analyse aus routinedaten deutscher krankenhäuser 2005-2012. Unfallchirurg 2018;121:642-8. [Google Scholar]
- 16.Pintar FA, Yoganandan N, Maiman DJ, Scarboro M, Rudd RW. Thoracolumbar spine fractures in frontal impact crashes. Ann Adv Automot Med 2012;56:277-83. [Google Scholar]
- 17.Vladutiu CJ, Marshall SW, Poole C, Casteel C, Menard MK, Weiss HB. Adverse pregnancy outcomes following motor vehicle crashes. Am J Prev Med 2013;45:629-36. [Google Scholar]
- 18.Johnson HC, Pring DW. Car seatbelts in pregnancy: The practice and knowledge of pregnant women remain causes for concern. BJOG 2000;107:644-7. [Google Scholar]
- 19.Elsoe R, Larsen P, Nielsen NP, Swenne J, Rasmussen S, Ostgaard SE. Population-based epidemiology of tibial plateau fractures. Orthopedics 2015;38:e780-6. [Google Scholar]
- 20.Fitschen-Oestern S, Lippross S, Lefering R, Besch L, Klüter T, Schenzer-Hoffmann E, et al. Missed foot fractures in multiple trauma patients. BMC Musculoskelet Disord 2019;20:121. [Google Scholar]










