Bilateral traumatic night stick fractures are rare, open reduction and internal fixation helps in getting good outcome.
Dr. G S Prasanna Kumar,
Department of Orthopaedics, Grant Government Medical College, Mumbai, Maharashtra, India.,
E-mail: prasannakumargs5@gmail.com
Introduction: Unilateral isolated ulna fracture secondary to trauma are common but the bilateral nightstick fractures are quite rare in the clinical scenario. These are managed conservatively or surgically depending upon the degree of displacement, location of the fracture, fracture pattern and associated injury to other bones. Proper management of these fractures helps in getting a better outcome. The purpose of the study was to present a case of bilateral traumatic isolated ulna fracture and its management.
Case Report: A 33-year-old male presented to the emergency department with complaints of pain and swelling over the dorsum of both forearms with a history of assault with a bamboo stick. The mechanism of the injury was, the patient placed his both the forearms in front of the face as a defense during the assault and sustained injury to both forearms. On examination, the patient had bilateral forearm swelling with tenderness. Bony crepitus was present over both the ulna on palpation. X-ray of both forearms (radius and ulna) revealed the fracture of both right and left ulna without any associated fractures/injuries. The patient was managed surgically with open reduction and internal fixation using a 3.5 mm locking compression plate. At present, 1-year follow-up, the patient is having complete wrist, elbow ROM and supination, pronation without any pain.
Conclusion: Bilateral traumatic Nightstick fractures of the ulna are rare and this is the first reported case of traumatic bilateral isolated ulna fracture according to author’s best knowledge and literature review. Open reduction and stable internal fixation using the principles of fracture fixation along with early mobilization helps in getting better functional outcome and prevents further complications and secondary procedures. This case is unique as it helps in identifying the mode of trauma in medico legal cases like assault in cases of bilateral ulna fracture. The mode and the mechanism of injury are different in this case.
Keywords: Nightstick fracture, surgical management, open reduction and internal fixation.
Fracture of both bone forearm, radius, and Ulna secondary to trauma is a very common scenario in clinical practice. In most of the cases, it is secondary to vehicular accidents or assault. Nightstick fracture is an isolated fracture of the ulnar shaft. The fracture got its name from the idea that a suspect struck with a police Nightstick would hold his forearm above his face in a defensive posture when struck with the police baton resulting in a fracture to the Ulna. These fractures are caused by any direct blow to the medial forearm, but can also be seen with excessive pronation or supination of the forearm [1]. In most of the cases, the fracture is unilateral in very rare situations it is found to be involving both the sides Ulnar shaft fractures are defined as those occurring between the distal aspect of the coronoid proximally and the ulnar neck distally. In most instances, the fracture is seen at the mid-shaft level. The incidence of diaphyseal fracture of the Ulna is reported to be 1–10/thousand people/year although rates vary by age and sex with incidents more common in young males. Nightstick fractures are typically closed injuries and patient present with obvious pain and lack of function in the affected extremity. These fractures are managed either conservatively with below elbow cast, functional brace [2, 3, 4] or operatively with titanium elastic nail (TENS) nailing or open reduction and internal fixation (ORIF) with plating. This case is unique because of mode of trauma was assault. The literature showed two cases of bilateral ulna fracture, one was stress fracture and other one was rheumatoid arthritis patient on steroids.
A 33-year-old male presented to the emergency with complaints of pain and swelling over the dorsum of both forearms. The patient was unable to perform any movements of the wrist and elbow. The patient had a history of assault, was attacked by an unknown person with a bamboo stick. The patient had placed his forearm in front of the face as a defense and sustained an injury to both forearms.
On examination, tenderness was present over both right and left subcutaneous border of the ulna with abrasion measuring 2*1 cm on the left side. The swelling was present in both the forearms with no distal neurovascular deficit.
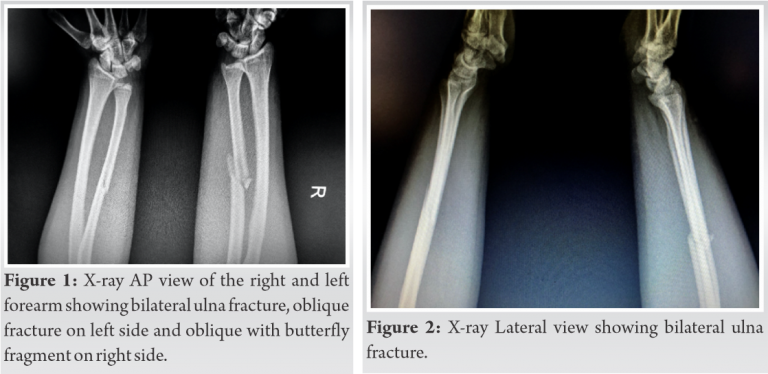
X-ray both forearms (radius ulna with wrist and elbow) AP and lateral views showed isolated ulna shaft fracture with butterfly fragment on the right side and oblique ulna fracture on the right side with no associated fracture of the radius on both the sides and no other injuries (Fig. 1, 2). X-ray of both the wrists and elbow were normal. The patient was initially managed with above elbow plaster of Paris slab, limb elevation and analgesics. As the patient was young active male and in view of early mobilization, we planned for open reduction and internal fixation of both the ulna fractures.

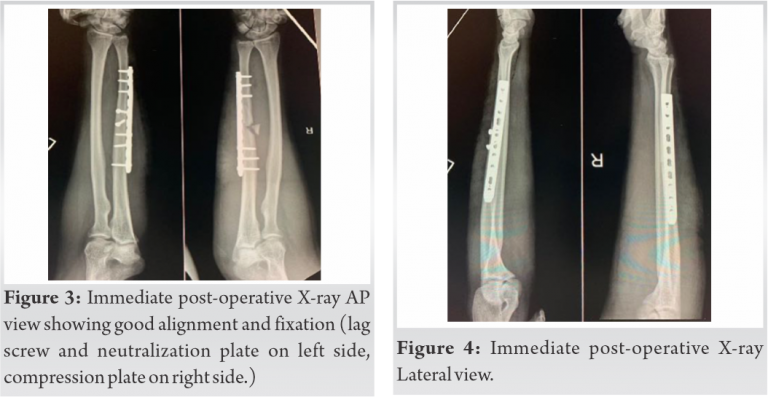
Under general anesthesia, tourniquet and with all aseptic precautions, the patient was operated in the supine position with forearm resting on the side support attached to the table on both sides. Right-sided ulna fracture was operated first taking incision over the subcutaneous border of ulna and between flexor and extensor carpi ulnaris muscle. Fracture site was identified, cleaned and reduced anatomically with butterfly fragment left in situ without disturbing the soft tissue or devitalizing the fragment. The fracture was fixed with 10 holes 3.5 mm locking compression plate (LCP) in compression mode with 6 bicortical screws. Left-sided ulna fracture was fixed with 2 lag screws and 10 holes 3.5 mm LCP as neutralization plate. Hemostasis was achieved and the wound was closed in layers. Both the nightstick fractures were operated on the same day and in one setting. The immediate postoperative radiograph of the both the forearms AP and Lateral views showed good fracture reduction with alignment (Fig. 3, 4). Wrist and elbow range of motion was started from the 2nd day of surgery. The patient was followed up regularly every month. At present, 1-year follow-up, the patient is having no pain at the fracture and having complete wrist, elbow and forearm rotatory movements (Fig. 5, 6). Follow-up X-ray of both the forearms AP and Lateral view showed primary bone healing on the left side and secondary healing on the right side (Fig. 7, 8).
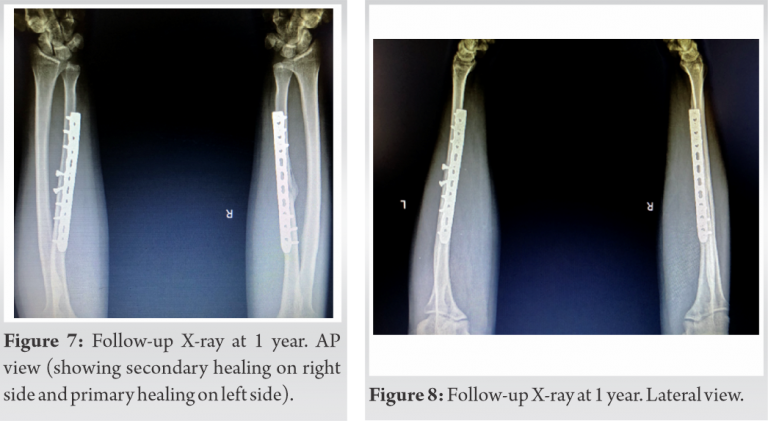
The fractures of the forearm bones are common in clinical practice but isolated fracture of ulna on both sides is very rare and so proper decision should be taken in such cases. Proper examination of the patient should be done. Injury to the elbow or wrist should be assessed and DRUJ integrity to be assessed, Monteggia and Galeazzi fracture to be ruled out. The decision about the conservative management and operative management to be taken after considering patients age, demands, comorbidity if any and importantly the fracture displacement. Fracture with no displacement or minimal displacement with more than 50% contact can be managed conservatively, given the low degree of surrounding periosteal and interosseous membrane damage associated with non-displaced fractures [5]. Conservative management includes above elbow or below elbow cast, functional bracing, and displaced fracture to be managed operatively with either ORIF with plating [6, 7] or intramedullary nailing using TENS [8, 9]. We prefer ORIF and plating in adults, as it helps anatomical fracture reduction and early mobilization. Many studies support mobilization in functional brace rather than immobilizing in below elbow or above elbow cast/slab, to avoid unnecessary discomfort to the patient. In postoperative period early mobilization of wrist and elbow should be initiated and active forearm motion should be initiated after suture removal, as tolerated. Weight lifting to be initiated gradually as tolerated starting with 2 kg and increasing thereafter. Stable fracture fixation helps in early mobilization, which in turn helps in getting better functional outcome. Repeat X-ray to be taken at 2–3 weeks interval to see and assess for the signs of the union on X-rays also see for clinical signs of the union. In adults classically, nonunion is of greatest concern in the management of isolated fractures of the ulnar shaft; however, it appears that rates of nonunion may be lower than previously thought. For non-operatively managed fractures, nonunion rate ranging from 2% to 4% is seen. In nightstick fractures that were managed surgically, the nonunion rate was 0–2% for fractures treated with plate fixation, while fractures treated with intramedullary fixation had a 5% rate of nonunion [10]. Proper execution of fracture fixation principles like compression in transverse fractures, use of lag screw and neutralization plate in oblique fracture and bridge platting in comminuted fractures helps in preventing non-union along with stable fixation. In case of fracture with butterfly fragment, one can do primary fixation and compress the butterfly fragment to the main fragment using vicryl suture, it helps to maintain the contact between two fragments till the fracture union. Another way is not to disturb the soft tissue attachment of the butterfly fragment, which eventually heals by secondary healing as happened in our case. While doing the ORIF, the choice of the implant can be DCP or LC-DCP. Or LCP, almost all have shown similar results. The anatomical restoration of ulnar alignment (in length, rotation, and axis) has to be the primary goal of surgical treatment to regain an unrestricted elbow and wrist function [11]. Dorsal placement of plate causes higher posterior impingement problems and soft tissue irritation, which may require implant removal latter [12, 13]. We did not find any reported cases of isolated traumatic bilateral ulna fracture in the literature, but there are two reported cases of bilateral ulna stress fractures without any trauma, one in an old patient with rheumatoid arthritis on steroids [14] and another is a bilateral ulna stress fracture in a young weight lifter [15]. Both the patients were managed with conservative management.
Bilateral traumatic Nightstick fractures of the ulna are rare and this is the first reported case of traumatic bilateral isolated ulna fracture according to authors’ best knowledge and literature review. Open reduction and stable internal fixation using the principles of fracture fixation along with early mobilization helps in getting better functional outcome and prevents further complications and secondary procedures. This case is unique as it helps in identifying the mode of trauma in medico legal cases like assault in cases of bilateral ulna fracture. The mode and the mechanism of injury is different in this case.
Although traumatic bilateral nightstick fractures are rare, history, clinical examination, and radiological investigations help in the diagnosis. Conservative or surgical management depends on age, displacement of the fracture and associated co morbidities. Fixation of both the ulna fractures in the same setting helps in preventing anaesthesia related morbidity to the patient, decreases the hospital stay and also helps in early mobilization.
References
- 1.Ali M, Clark DI, Tambe A. Nightstick fractures, outcomes of operative and non-operative treatment. Acta Medica (Hradec Kralove) 2019;62:19-23. [Google Scholar]
- 2.Altner PC, Hartman JT. Isolated fractures of the ulnar shaft in the adult. Surg Clin North Am 1972;52:155-70. [Google Scholar]
- 3.du Toit FP, Grabe RP. Isolated fractures of the shaft of the ulna. S Afr Med J 1979;56:21-5. [Google Scholar]
- 4.Sarmiento A, Latta LL, Zych G, McKeever P, Zagorski JP. Isolated ulnar shaft fractures treated with functional braces. J Orthop Trauma 1998;12:420-4. [Google Scholar]
- 5.Dymond IW. The treatment of isolated fractures of the distal ulna. J Bone Joint Surg Br 1984;66:408-10. [Google Scholar]
- 6.Anderson LD, Sisk TD, Tooms RE, Park WI. Compression-plate fixation in acute diaphyseal fractures of the radius and ulna. J Bone Joint Surg Am 1975;57:287-97. [Google Scholar]
- 7.Chapman MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute fractures of the diaphyses of the radius and ulna. J Bone Joint Surg Am 1989;71:159-69. [Google Scholar]
- 8.Boriani S, Lefevre C, Malingue E, Bettelli G. The Lefevre ulnar nail. Chir Organi Mov 1991;76:151-5. [Google Scholar]
- 9.Zanasi R, Franceschini R, Rotolo F, Romano P, Galmarini V, Zanasi L. Intramedullary osteosynthesis. 4. Kuntscher nailing in the ulna. Ital J Orthop Traumatol 1990;16:369-78. [Google Scholar]
- 10.Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: A systematic review. Injury 2000;31:565-70. [Google Scholar]
- 11.Siebenlist S, Buchholz A, Braun KF. Fractures of the proximal ulna: Current concepts in surgical management. EFORT Open Rev 2019;4:1-9. [Google Scholar]
- 12.Ries C, Wegmann K, Meffert RH, Muller LP, Burkhart KJ. Double-plate osteosynthesis of the proximal ulna. Oper Orthop Traumatol 2015;27:342-56. [Google Scholar]
- 13.Hackl M, Mayer K, Weber M, Staat M, van Riet R, Burkhart KJ, et al. Plate osteosynthesis of proximal ulna fractures-a biomechanical micromotion analysis. J Hand Surg Am 2017;42:834.e1-7. [Google Scholar]
- 14.Venkatachalam S, Dixon P. Spontaneous bilateral distal ulna fracture: An unusual complication in a rheumatoid patient. J Orthop Traumatol 2011;12:119-22. [Google Scholar]
- 15.Steunebrink M, de Winter D, Tol JL. Bilateral stress fracture of the ulna in an adult weightlifter: A case report. Acta Orthop Belg 2008;74:851-5. [Google Scholar]










