Ultrasound guided central-line insertion should always be recommended in every case of kyphoscoliosis surgery due to its altered anatomy, and thereby, preventing a rare brachial plexus injury.
Dr. Hitesh N. Modi,
Department of Orthopaedics and Spine Surgery, Zydus Hospitals and Healthcare Research Pvt. Ltd.,
Thaltej, Ahmedabad, Gujarat, India.
E-mail: drmodihitesh@gmail.com
Introduction: Internal Jugular Venous (IJV) cannulation or central-line insertion is frequently performed during kyphoscoliosis deformity correction surgery or spine surgery with high risk. This helps monitor central venous pressure and administer medicines when required. Although many complications of IJV cannulation have been reported in the literature, its effect on brachial plexus is not known. The objective of this paper was to report a rare complication of IJV during scoliosis surgery.
Case Presentation: We reported a case of 27-year-old male who was operated for severe kyphoscoliosis correction where preoperatively IJV cannulation was done. Repeated attempts were done during IJV cannula insertion due to altered anatomy. Eventually, cannula insertion was done using ultrasound modality and surgery for correction was done. Postoperatively patient developed right upper extremity weakness and sensory loss although the clinical result of kyphoscoliosis correction was acceptable. EMG-NCV study proved it brachial plexus injury. The patient was treated with intravenous steroid and physiotherapy. The patient recovered completely within 6 months of surgery.
Conclusion: We reported a case of kyphoscoliosis deformity corrective surgery where IJV cannulation led to brachial plexus injury and was eventually recovered with medications and physiotherapy.
Keywords: Scoliosis correction, Central-line insertion, Brachial plexus injury.
Cannulation of internal jugular vein (IJV) or central-line is frequently performed in long-duration surgery for the monitoring of central venous pressure (CVP) and administration of medicines and intravenous fluids [1]. The right internal jugular vein is easily accessible and is preferred by anesthetist for the procedure. Accessing the IJV from the right side prevents the complication of pneumothorax in individuals; however, the other life-threatening complications have been reported in the literature [2, 3]. One of the rare complications is damage to the brachial plexus which has not been mentioned during spine surgery. The purpose of this article is to highlight a rare complication of central-line cannulation in the case of kyphoscoliosis deformity correction. The patient developed right upper limb palsy after surgery. Our purpose was to find the reason that results in brachial plexus injury and follow the diagnosis and recovery pattern following such rare complication.
A 27-year-old male presented to the out-patient department with complaints of deformity in back. The deformity was progressing, and he reported frequent respiratory difficulty due to restricted chest expansion. The power in all four limbs was of grade five with intact sensations. The preoperative Cobbs’ angle was 1350 (Fig. 1). The patient was informed about the procedure and surgery for kyphoscoliosis was performed under neuromonitoring guidance. The pre-operative blood investigations and chest X-ray were within the normal limits. An echocardiogram revealed ejection fraction (EF) of 60% with normal left ventricular function. The patient weighed 70 kg. He was kept nil-by-mouth (fasting) overnight and oxygen was administered through a mask while the patient was being transferred to the operation room (OR). In OR various parameters were continuously monitored throughout surgery. Direct blood pressure monitoring was performed with the left radial artery cannulation. Peripheral venous cannula was inserted before induction. When fully paralyzed after drug administration, the patient was intubated with number seven cuffed endotracheal (ET) tube. After securing the airway, he was positioned for right internal jugular cannulation (IJV). The area was cleaned and draped for the procedure under aseptic condition. A 22-gauge needle was used to locate the vein just lateral to the carotid artery at the level of the thyroid cartilage. Multiple attempts failed to locate the vessel. Hence, the landmarks were reassessed, and the procedure was performed under ultrasound guidance. The vessel was cannulated with an 18 gauge triple lumen catheter by Seldinger technique [4]. After securing the cannula with skin suture, the distal lumen was connected to a pressure transducer for central venous pressure recording and a proximal lumen for infusion of fluids.
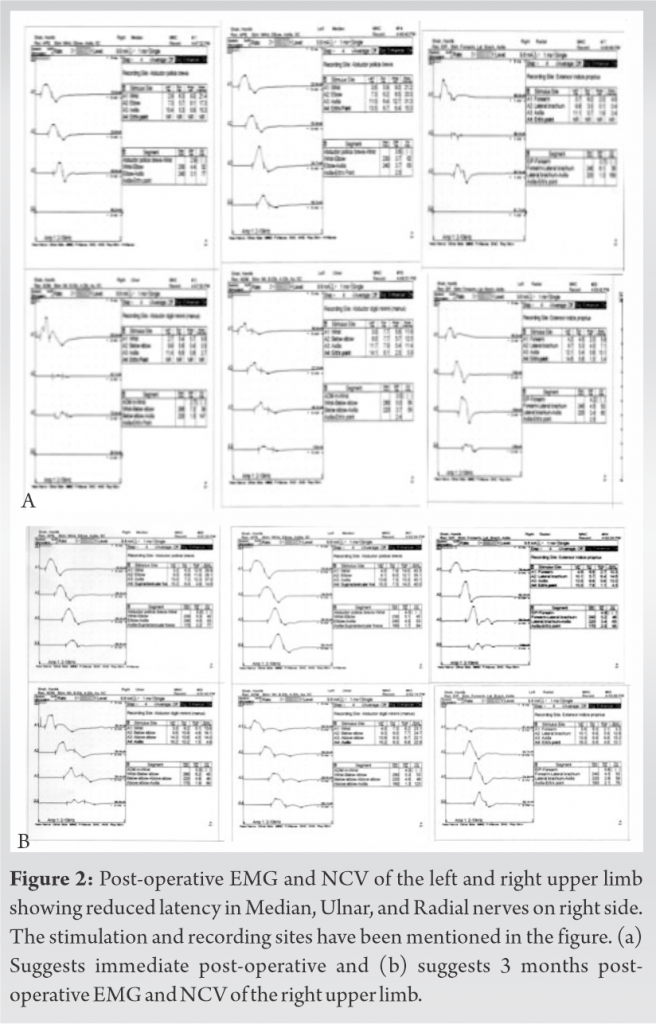
The patient was given prone position with both arms in 900 flexion and padded over soft gel cushions to prevent any compression injury. Peripheral pulsations were confirmed in all four limbs before the surgery. Baseline motor-evoked potentials (MEP) were checked before surgery. Surgery was performed with pedicle screw insertion, corrective osteotomy at the apex and correction of deformity [5] using rod-derotation and cantilever technique (Fig. 1). The intraoperative neuromonitoring (IONM) data were maintained throughout the surgery. Intraoperative blood pressure was maintained with a mean arterial pressure of 80 during the entire surgery. Three units of packed cell volume (PCV) were infused during surgery. The surgery and anesthesia were otherwise uneventful, and he was transferred to the intensive care unit (ICU) for elective post-operative care. On clinical neurological assessment next morning postoperatively, his power in the right upper limb had reduced to grade one with hypoesthesia below C5 dermatome. The neurology in all other limbs was same as the pre-operative stage. Immediate post-operative CT scan did not show any malposition of screws or any abnormality of the cervical spine. IJV sutures were also checked which did not suggest possibility of injury due to needle prick of suturing needle. A neurologist was consulted immediately. Electromyography and nerve conduction study (EMG-NCV) of both upper limbs was performed within 24 h after the completion of surgery, which showed brachial plexus injury on the right side (Fig. 2a). After explaining the event to patient and his relatives, he was treated with physiotherapy protocol with electric nerve stimulation of affected limb and intravenous steroids (intravenous methylprednisolone 1 g once daily for five days. This was followed by oral steroid administration (methylprednisolone 8 mg thrice a day) for 5 days. Besides steroids, he was given vitamin B-complex supplements, and the dynamic radial splint was applied. He started improving power in terms of flickering and against gravity in 5 days following surgery. At the time of discharge after a week of surgery his power in the right wrist, elbow, and shoulder was Grade 2 and Grade 4 in fingers. He eventually showed full recovery of neurology in the right upper limb 6 months following the primary surgery. EMG-NCV study of the both upper limbs was performed at 3 months of follow-up showed complete recovery in the pattern (Fig. 2b). At the final follow-up, powers in all limbs were grade five with normal sensations. His deformity in back has reduced to an acceptable level and can perform daily activities without support. He also returned to his job that included working on computers and typing for 8 h a day.
Nerve injuries after internal jugular cannulations have been reported in the past [6]. These included Horner’s syndrome, accessory nerve injury and permanent paralysis of C5-7 and phrenic nerve [3, 6]. However, this is the first case report which discusses the injury to brachial plexus after central venous line insertion in a case of spinal deformity correction. The patient in this case report had developed a transitional injury of brachial plexus which improved with time. There are several factors which may contribute to brachial plexus injury in a case of long-standing spine surgery. Stretching, compression, and hyper abduction of the arm are a few to enlist [7]. In this case report, the arms were carefully positioned with adequate padding with soft gel cushions during surgery in the same manner as it has been done in numerous surgeries performed in the past. Shoulders were supported to avoid the hanging situation which may sometimes stretch the brachial plexus. Hence, the reason being over-stretching of the arm was ruled out. Another study (Briscoe) had reported brachial palsy due to extravasation of fluids after central venous cannulation [6]. Although the incidence of such cases is less, the possibility was also ruled out after a CT scan of the involved area. The absence of any collection or hematoma in the vicinity of the cannula placement was also confirmed on ultrasound. Sutures marks around the cannula were also confirmed to rule out any possible injury due to the needle in our case. In our opinion, a direct injury would be the most likely cause as there were multiple failed attempts at locating the vessel before ultrasound was used to cannulate it. The brachial plexus is found in close proximity to the internal jugular vein and both course through the outer scalene groove [4, 8]. In a few studies, it has been reported that the upper trunk of brachial plexus gets damaged when the needle is placed too laterally [8]. In another study by Hickey et al., about 13% of individuals have somatosensory evoked potential changes during central venous cannulation without any post-operative sequelae [9]. Neurological assessment of the involved nerve root after such a procedure may be helpful. Motor-evoked-potential (MEP) and somatosensory evoked potential (SSEP) assessment of cervical roots on the site of venous cannulation may provide to be beneficial by preventing the delay in detection and management of such an injury [10]. Moreover, patients who require multiple attempts for insertion of the cannula should be closely followed-up. Whenever suspected, immediate post-operative EMG and NCV are helpful [10]. In our case, we have investigated injury in form of EMG/NCV within 24 h of the surgery. This should be followed by early medical management including steroid use and passive mobilization and electrical stimulation along with physiotherapy protocol [11]. The same treatment protocol was followed in our case too. Although the success rate of IJV cannulation using anatomical landmarks is 95%, various parameters such as obesity, neck deformity, and inability to lie flat may make the procedure difficult [12, 13]. Ultrasound may be of help in such cases to prevent brachial plexus injury [12, 14]. It was an important learning point from our case to use USG from the beginning while inserting IJV cannulation if anatomical landmarks are altered. From this case onward, we strictly kept a policy of using USG guided IJV cannulation in every case of spinal deformity at our institution. We recommend using USG for IJV cannulation whenever there is doubt about anatomical landmarks. Another important aspect to be identified is whether the neuropathy is purely sensory or motor. Whenever the neuropathy is purely sensory, it is safe to wait for a week and recovery occurs in this time period [15]. Our patient had both sensory and motor nerve involvement, and hence, the neurologist was immediately consulted. Immediate EMG and NCS were conducted within 24 h of surgery which showed brachial plexus injury. The patient was treated with intravenous steroids and physiotherapy protocol with repeat EMG and NCV after 3 months. Repeat EMG and NCV have confirmed the complete recovery pattern.
Brachial plexus injury is a rare complication of IJV cannulation and should be specially taken care of in patients with spinal deformities. Ultrasound guidance should be used from the beginning while inserting IJV cannulation in such patient due to altered anatomical landmarks. Pre-operative counseling for USG guided IJV cannulation and possible complications should also be included. This helps in preventing repeated punctures and possibility of brachial plexus injury. Immediate post-operative EMG and NCS are helpful along with neurologist consult in case of associate motor deficits. Such patients usually show acceptable recovery with the use of intravenous steroid, splints, electrical stimulation, nutritional supplements, and vigorous physiotherapy.
Brachial plexus injury during spine surgery can happen due to root stretching as well as central line insertion which should be kept in mind. Injuries due to excessive stretching of root can be controlled with proper padding and avoiding excessive stretching of arm. Brachial plexus injury due to central line cannulation should be avoided using ultrasound guided insertion of cannula in every case of spinal deformity, and thus avoiding repeated punctures due to altered anatomy.
References
- 1.Akaraborworn O. A review in emergency central venous catheterization. Chin J Traumatol 20;3:137-40. [Google Scholar]
- 2.Kollar G, Alizadeh H, Gulyas E. Nurse style of central vein? Our experience in the peripherally inserted central venous catheter. Orv Hetil 158;22:856-63. [Google Scholar]
- 3.Nowak LR, Duda K, Mizianty M, Wilczek M, Bieda T. Horner syndrome after unsuccessful venous port implantation by cannulation of the right internal jugular vein. Anaesthesiol Intensive Ther 47;4:336-8. [Google Scholar]
- 4.Tan J, Liu L, Xie J, Hu L, Yang Q, Wang H. Cost-effectiveness analysis of ultrasound-guided Seldinger peripherally inserted central catheters (PICC). Springerplus 5;1:2051. [Google Scholar]
- 5.Chan A, Parent E, Narvacan K, San C, Lou E. Intraoperative image guidance compared with free-hand methods in adolescent idiopathic scoliosis posterior spinal surgery: A systematic review on screw-related complications and breach rates. Spine J 2017;17:1215-29. [Google Scholar]
- 6.Brisco CE, McDonald WI. Extensive neurological damage after cannulation of internal jugular vein. Br Med J 1974;1:314. [Google Scholar]
- 7.Ferrero-Manzanal F, Lax-Perez R, Lopez-Bernabe R, Betancourt-Bastidas JR, de Onzono-Perez AI. Traction injury of the brachial plexus confused with nerve injury due to interscalene brachial block: A case report. Int J Surg Case Rep 2016;27:78-82. [Google Scholar]
- 8.Yuan KM, Liu EC, Li P, Shangguan WN, Li J, Lian QQ. Anatomic variations of neck vessels and the course of pediatric internal jugular veins. Paediatr Anaesth 2017;27:1003-9. [Google Scholar]
- 9.Hickey C, Gugino GL, Anglio LS, Mark JB, Son SL, Maddi R, et al. Intraoperative somatosensory evoked potential monitoring predicts peripheral nerve injury during cardiac surgery. Anesthesiology 1993;78:29-35. [Google Scholar]
- 10.Labrom RD, Hoskins M, Reilly CW, Tredwell SJ, Wong PK. Clinical usefulness of somatosensory evoked potentials for detection of brachial plexopathy secondary to malpositioning in scoliosis surgery. Spine (Phila Pa 1976) 2005;30:2089-93. [Google Scholar]
- 11.Vaish A, Ahmed S, Shetty A. Remote physiotherapy monitoring using the novel D+R therapy iPhone application. J Clin Orthop Trauma 2017;8:21-4. [Google Scholar]
- 12.Keenan SP. Use of ultra sound to place central lines. J Crit Care 2002;17:126-37. [Google Scholar]
- 13.Jung CW, Jalilov G, Song IK, Kim EH, Kim HS, Kim JT, et al. Position and relative size of the vertebral artery according to age: Implications for internal jugular vein access. Paediatr Anaesth 2017;27:997-1002. [Google Scholar]
- 14.Mohan VK, Nisa N. Importance of sonography for guiding central venous cannulation in patients with neurofibromatosis. Turk J Anaesthesiol Reanim 2017;45:169-71. [Google Scholar]
- 15.Warner MA, Warner ME. Ulnar neuropathy, incidence outcome and risk factors in sedated or anaesthetised patients. Anesthesiology 1994;81:1332-40. [Google Scholar]