Post-traumatic patellofemoral autofusion is a rare cause for knee arthrofibrosis and surgeons should focus on modifiable risk factors, patient expectation management, and if necessary conversion to an open procedure in a patient with significant knee stiffness that is recalcitrant to operative management with knee arthroscopy, manipulation, and lysis of adhesions.
Dr. Thomas Herron,
Department of Orthopedic Surgery, University Hospitals Regional Medical Centers, Cleveland, Ohio, United States. E-mail: thomas.herron@uhhospitals.org
Introduction: Post-traumatic patellofemoral auto fusion is poorly described in the literature and its etiology may be multifactorial. Management options are not well published and this case report addresses a rare and complex case of patellofemoral autofusion after a patellar tendon repair with a description of our surgical approach and ultimately improvement in patient outcome and satisfaction.
Case Presentation: A 59-year-old African American female suffered an acute traumatic patellar tendon rupture that was treated with a primary repair that resulted in sequelae leading to a subsequent open procedure revealing an osseous bridge between the patella and trochlea. After osteotomy of this bridge, the patient’s range of motion improved.
Conclusion: For the appropriate management of arthrofibrosis surgeons should focus on modifiable risk factors including close follow-up with patients, patient expectation management, and consider surgical intervention such as techniques described below in recalcitrant cases to evaluate for post-traumatic sequelae including bone bridge formation.
Keywords: Patella tendon, arthrofibrosis, tendon repair.
Knee stiffness is an extremely common complication following knee surgery. The cause is typically multifactorial with biologic and genetic factors [1, 2, 3] playing a role as well as risks factors such as injury severity, delayed post-operative physical therapy, and prolonged immobilization [4]. The symptoms are most commonly diminished range of motion (ROM), persistent pain, and swelling. This leads to varying levels of functional disability due to difficulty ambulating, stair climbing, and driving [2, 4] which can have a devastating impact on the patient. Typical management of knee arthrofibrosis refractory to postoperative physical rehabilitation includes manipulation under anesthesia (MUA) as well as arthroscopic lysis of adhesions to maximize ROM [4]. Arthrofibrosis refractory to arthroscopy and MUA may undergo open treatment to evaluate the repaired construct and examine for calcifications, heterotopic ossification, or myositis ossificans which may be impeding motion [4]. Bone bridge formation, or auto fusion, of the patellofemoral joint after knee surgery from persistent and severe stiffness is a complication that is not well documented in current literature and its management options are not well defined.
A 59-year-old African American female suffered an acute traumatic patellar tendon rupture after slipping on ice at work. The patient underwent primary repair for the patellar tendon rupture 1 week later using an anterior longitudinal incision with ultra-high-strength suture tape in Krackow stitch fashion within the tendon and fixated to the patella using bone anchors. The retinaculum was repaired in a standard fashion similar to previously described techniques [5, 6]. It is generally accepted that primary repairs for patellar tendon ruptures should follow a rehabilitation protocol that includes early ROM exercises and persistent therapy for several weeks and avoid prolonged immobilization to ensure maintained ROM [7]. The general post-operative protocol for this type of surgery was intended; however, the patient’s physical therapy was delayed approximately 4 weeks due to ongoing worker’s compensation claim. Once the patient was able to initiate therapy, she participated for 3 months. On follow-up office visits every 3–4 weeks, the patient’s ROM after the patellar tendon repair did not improve beyond 20 degrees of knee flexion and five degrees knee extension with firm endpoints. 6 months after the primary patellar tendon repair the patient elected to undergo diagnostic knee arthroscopy with lysis of adhesions and MUA.
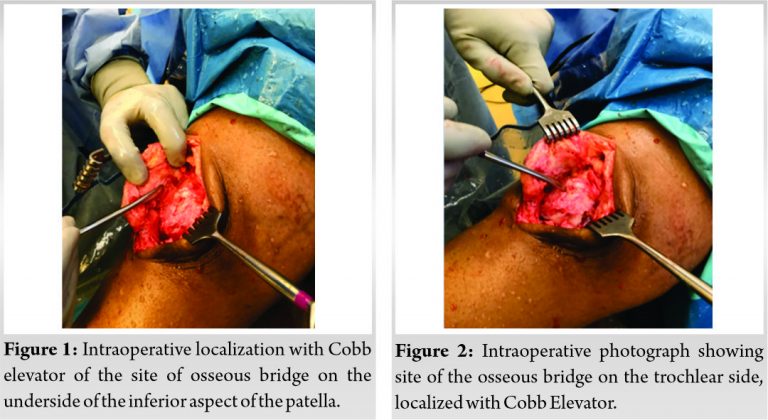
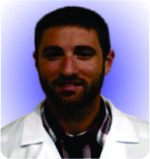
During diagnostic arthroscopy, the trocar was placed through medial and lateral portals, breaking up adhesions in the process. The patient’s ROM remained unchanged after this intervention. While attempting to enter the patellofemoral joint, the trocar repeatedly hit a firm endpoint at the inferior pole of the patella and was unable to pass through what was suspected adhesions. Intraoperative fluoroscopy was utilized to identify and localize any osseous abnormalities and to confirm portal placement. After confirming accurate portal placement and finding that the trocar was unable to be passed despite fluoroscopic guidance, the procedure was converted to an open arthrotomy through a medial arthrotomy incision in order to expose the knee joint for better visualization. A bone bridge was noted in the inferior patellofemoral joint adjacent to the repaired patella tendon. An osteotome was used to break apart the patellofemoral bone bridge (Fig. 1, 2). Further lysis of adhesions and manipulation of the knee was performed and the patient fixed 20-degree contracture immediately improved to 90 degrees of flexion, most significantly enhanced following osteotomy of the bone bridge.
The patient began therapy immediately after the second procedure. At 6 week follow-up, the patient had 50 degrees of knee flexion and knee extension at five degrees. She was prescribed a Dynasplint to help improve ROM and continued to work with therapy for several more weeks. Her ROM declined, and at the 3, 4, and 5-month post-op follow-up it remained at 25–30 degrees of knee flexion. The patient was referred to a joints specialist for possible total knee arthroplasty, however, given her poor preoperative ROM, it was determined to be an inadequate solution at that point in time. The patient continued to work consistently with therapy, and at 18 months post-operatively, she has a documented ROM at 60–70 degrees of knee flexion with a significant decline in pain since preoperative evaluation.
Arthrofibrosis is not an uncommon complication of major knee surgery with multifactorial components coming from both the nature of the injury and the postoperative course. It is considered standard practice to advance the ROM after major surgery as soon as it is reasonably possible. However in our case, after primary patellar tendon repair, the patient had a delay in physical therapy initiation of 4 weeks. Prolonged immobilization from knee surgery is a well-documented cause of motion loss, Hooper and Walton demonstrated motion loss in up to 46% of patients with a mobilization delay of only 2 weeks [8]. Thus our delay of 4 weeks likely played a major role in the development of arthrofibrosis and subsequent poor results from therapy once it was initiated. A true osseous bridge would have been unlikely to form had the patient been actively performing ROM as the strain through the site would have made bone formation highly improbable [9]. Furthermore, cognitive components of compliance and pain avoidance may have also played a role in reduced participation with therapy once it had been initiated [10]. It has been noted previously that an increase in attention to the pain symptoms and catastrophizing of pain may significantly influence the person’s motivation [11]. Regardless of our proposed mechanisms for the significant loss of ROM our biggest concern was adequate treatment once the patient re-presented to us with her initial loss of motion.
When severe stiffness remains after continued therapy, arthroscopic lysis of adhesions with manipulation of the knee remains an accepted treatment option [4]. Therefore, our first attempt to improve the patient’s ROM was the standard of care, and it was only intraoperatively that it became apparent to our team that a true osseous bridge had formed. After a thorough review of the literature, only one article pertained to the post-traumatic auto fusion of the knee that occurred after severe trauma. The authors performed an elective total knee arthroplasty for the patient where the patient went from zero degrees knee flexion to 90 degrees postoperatively, significantly improving the quality of life of the patient [12]. The case we discuss is different, as the patellofemoral auto fusion was an unexpected finding and had not been evident radiographically and despite the fact that our patient did not return to baseline, our surgical intervention did improve her ROM dramatically and pain has significantly reduced.
Given that this is an extremely uncommon event and an unexpected finding our suggestions at this time are for the surgeon to identify post-operative stiffness early, encourage aggressive adherence to physical therapy as soon as is safe and engage with the patient about any concerns that may affect their ability to perform rehab early and with frequent follow-up. In addition, patients that form a true osseous bridge will still benefit from a salvage procedure such as ours as our patient has continued to gain ROM in the postoperative period and is approaching the commonly accepted functional ROM for her knee [13].
Arthrofibrosis refractory to arthroscopy and MUA may undergo open treatment to evaluate and examine for calcifications which may be impeding motion..
References
- 1.Skutek M, Elsner HA, Slateva K, Mayr HO, Weig TG, van Griensven M, et al. Screening for arthrofibrosis after anterior cruciate ligament reconstruction: Analysis of association with human leukocyte antigen. Arthroscopy 2004;20:469-73. [Google Scholar]
- 2.Usher KM, Zhu S, Mavropalias G, Carrino JA, Zhao J, Xu J. Pathological mechanisms and therapeutic outlooks for arthrofibrosis. Bone Res 2019;7:9. [Google Scholar]
- 3.Watson RS, Gouze E, Levings PP, Bush ML, Kay JD, Jorgensen MS, et al. Gene delivery of TGF-β1 induces arthrofibrosis and chondrometaplasia of synovium in vivo. Lab Invest 2010;90:1615-27. [Google Scholar]
- 4.Magit D, Wolff A, Sutton K, Medvecky MJ. Arthrofibrosis of the knee. J Am Acad Orthop Surg 2007;15:682-94. [Google Scholar]
- 5.Capiola D, Re L. Repair of patellar tendon rupture with suture anchors. Arthroscopy 2007;23:906.e1-4. [Google Scholar]
- 6.Bushnell BD, Byram IR, Weinhold PS, Creighton RA. The use of suture anchors in repair of the ruptured patellar tendon: A biomechanical study. Am J Sports Med 2006;34:1492-9. [Google Scholar]
- 7.Volk WR, Yagnik GP, Uribe JW. Complications in brief: Quadriceps and patellar tendon tears. Clin Orthop Relat Res 2014;472:1050-7. [Google Scholar]
- 8.Hooper GJ, Walton DI. Reconstruction of the anterior cruciate ligament using the bone-block iliotibial-tract transfer. J Bone Joint Surg Am 1987;69:1150-4. [Google Scholar]
- 9.Claes L. Biomechanical principles and mechanobiologic aspects of flexible and locked plating. J Orthop Trauma 2011;25 Suppl 1:S4-7. [Google Scholar]
- 10.Breslow MJ. Neuroendocrine responses to surgery. In: Breslow MJ, Miller CF, Rogers MC, editors. Perioperative Management. St. Louis, MO: CV Mosby; 1990. p. 180-93. [Google Scholar]
- 11.Lukkahatai N, Saligan LN. Association of catastrophizing and fatigue: A systematic review. J Psychosom Res 2013;74:100-9. [Google Scholar]
- 12.Kumar N, Poswal P. Total knee arthroplasty in long standing post-traumatic isolated bony ankylosis of patellofemoral joint. J Arthrosc Joint Surg 2017;4:149-51. [Google Scholar]
- 13.Rowe PJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait Posture 2000;12:143-55. [Google Scholar]