Bone autograft osteosynthesis is ideal treatment for neglected gap non-union of small bones of the hand in paediatric patients.
Dr. Pankaj K. Sharma, Department of Orthopaedics, All India Institute of Medical Sciences, Bathinda, Jodhpur Romana, Mandi Dabwali Road, Bathinda - 151 001, Punjab, India. E-mail: dr.pankajkristwal@gmail.com
Introduction:Traumatic injuries of to hand are not uncommon in the pediatric population and most of them are managed by conservative means and rarely surgical intervention required. There is a very rare incidence of delayed union or non-union in these fractures and found a very few numbers of sporadic cases documented in English literature.
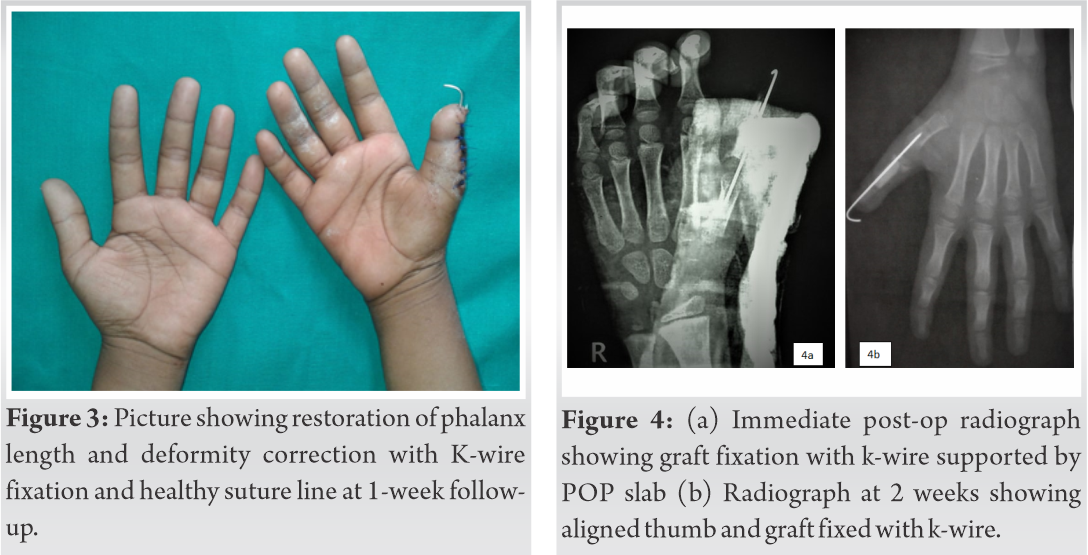
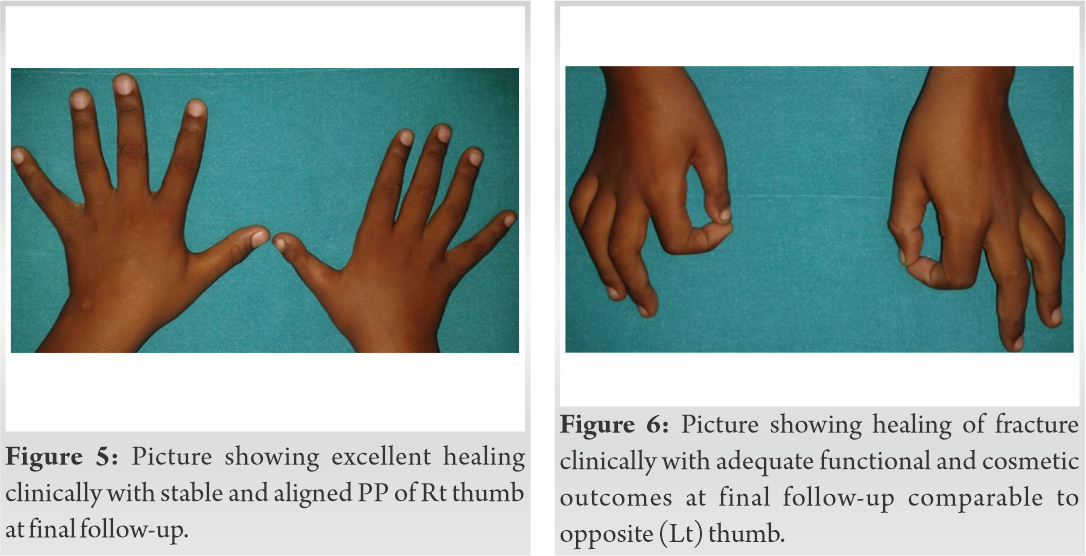
Case Report:We described delayed presentation of post-traumatic gap non-union of proximal phalanx of thumb in a child who presented with severe disability of hand especially writing and grasping. He was managed as open reduction, tibial strut bone grafting, and internal fixation with crossed Kirchner wire and followed for a period of minimum of 2 years. The fracture united radiologically and healed well clinically, whereas functional outcomes were excellent. There was no difficulty in writing and activity of daily living with operated hand while having comparative cosmetic appearance to other hand.
Conclusion:Non-union of phalanx fractures are very rare in the pediatric population whereas excellent clinical and functional outcomes can be achieved with adequate stable fixation and autologous bone grafting.
Keywords:Gap non-union, proximal phalanx, fracture, skeletally immature, tibial strut graft
Hands are vitally important for daily routine works with a wide variety of functions, i.e., touching, grasping, feeling, holding, manipulating and caressing, etc., and while the thumb is the cornerstone for all these functions [1]. The phalangeal fractures are often neglected or regarded as trivial minor injuries thus and managed conservatively [2]. The proximal phalanx (PP) of the fingers is fractured more frequently than the middle and distal phalanges. Stiffness and malunion are complications of phalanx fractures while the incidence of non-union is rare and accounting for <1% [3], [4], [5]. Compound fractures can lead to segmental loss of bone and are associated with severe morbidity in long term. Complications and morbidities related to thumb are unavoidable and need to be addressed and managed adequately [1], [2]. There is number of modalities to manage these fractures but the literature has no uniformity with respect to providing guidance to surgeon for specific pattern of fractures [2], [6]. There is a scarcity of medical literature related to the treatment of gap non-union of PP of the thumb and the forms of treatment discussed below for fracture patterns in these fractures is surgeon experience based.
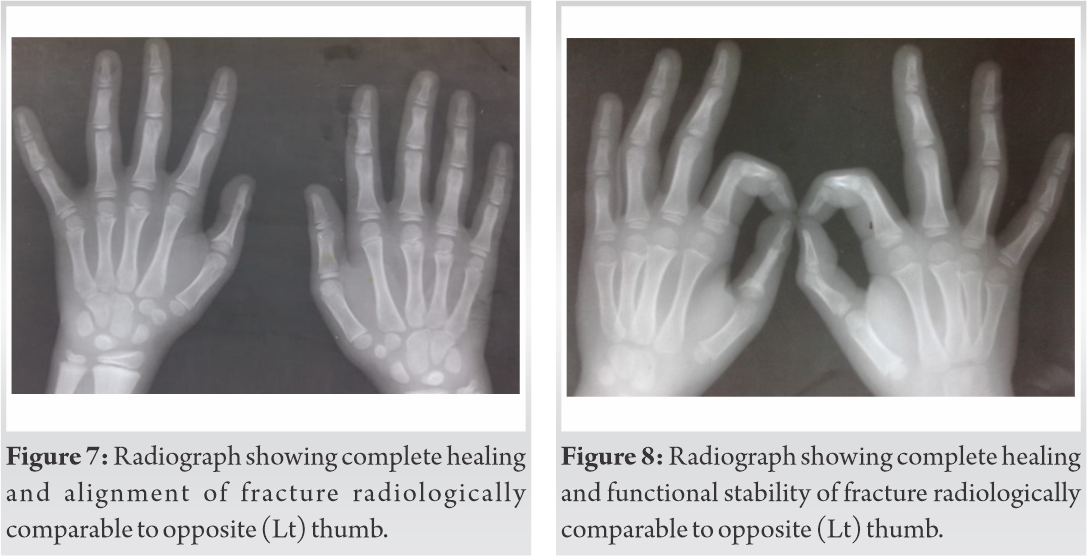
A 10-year-old child was brought to the orthopedics department in a tertiary care center with complaining of flail thumb of the right hand (dominant limb) and having difficulty in writing for the last 6 months duration. He had a past history of roadside accident having a compound fracture of PP right thumb with bone loss and treated as conservative means with wound debridement and closure without restoring limb length. On examination, obvious deformity and shortening was visible with intact distal neurovascular function and healthy scar over the wound. Bone discontinuity was apricated as a palpable gap percutaneously while thumb was unstable/flail with intact tendons. There was no fixed deformity and passive movements of the thumb were adequate. Clinical presentation of both hands is illustrated in (Fig. 1), showing deformity and instability shortening of the right thumb.True size radiographs of both hands were taken to calculate the actual length of PPs. It revealed gap non-union PP of the right thumb with preserved small articular cartilages at both ends as shown in (Fig. 2a). Traction radiographs of both hands showing gap non-union of PP right thumb in (Fig. 2b).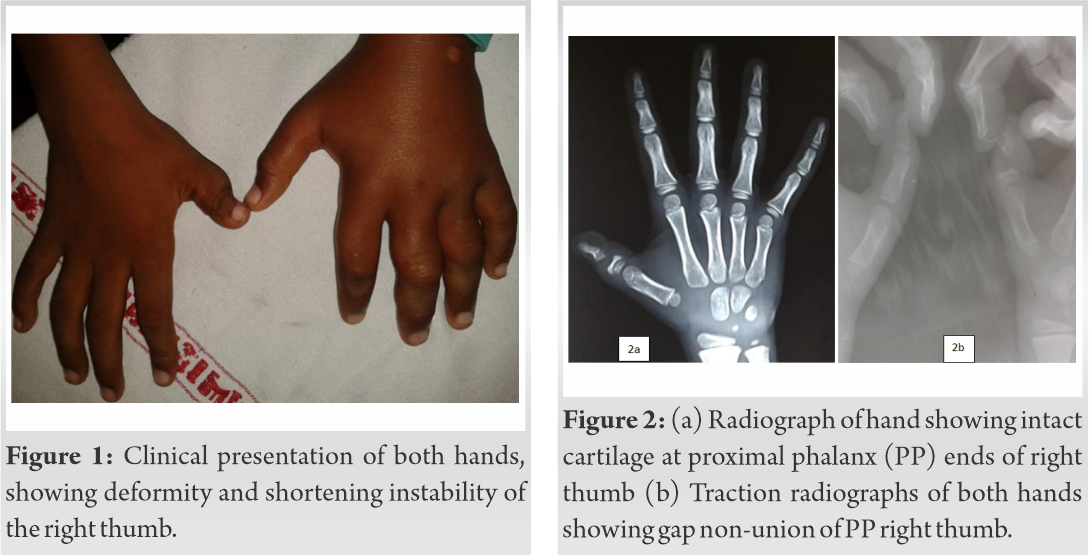
The Hand is one of the most frequently common injured part of the body in the pediatric and adolescent age group [2], [3], [4]. The border rays, i.e. the little finger and the thumb, are injured the most commonly among all injured fingers (52.2% and 23.4%, respectively) [5]. Children aged <10 year has low incidence of thumb fracture, but a steep rise is noted after the age of 10 years especially in male children [6], [7], [8]. Crush injuries are commoner in toddlers and associated mostly commonly with closing door caught while recreational sports usually affect an older child usually [7], [8]. The hand has unique anatomy than others which consists of mobile small bones, surrounded by ligaments and tendons in a complex interaction, favors for early and excellent healing resulting or adequate functioning and of hand resulting less complications [8]. The goal of any treatment is to have children return quickly to their daily leisure and academic activities. Uncomplicated, undisplaced, and stable fractures can be managed conservatively by reposition, casting, splinting, or early motion; with smaller follow-up [9], [10]. Surgical treatment is indicated either in severe displaced and irreducible fractures or if it is unstable after reduction or associated with substantial soft tissue trauma to stabilize enough to permit healing, to allow micromotion, and permitting endosteal or periosteal callus formation with early mobilization [11], [12]. Reduced bone fragments are fixed by an internal or external devices in form of osteosynthesis modalities including K-wire, mini plate system, and mini JESS systems [11], [12]. There is a great variation in the reported incidences of post-operative infection (0-8%), malunion (0-28%), and non-union (0-9%) [10], [13], [14].
Post-traumatic bone loss and delayed presentation due to compound fracture predisposed to non-union in the present case. Excellent bone healing needs adequate bone contact and stable fixation while no contact between the fracture fragments caused by segmental bone loss precludes such healing in this case. For segmental bone loss of fracture either allograft or corticocancellous autograft of cortico-cancellous bone is advised but allograft has a higher incidence of non-union or delayed union than autograft [15], [16]. The gold standard for reconstruction of large bone defects is the use of autogenous bone harvested from iliac crests graft or fibular strut grafts, used for filling bone gaps of segmental loss of bone [16]. The patient was skeletally immature and the gap was large, so we used a proximal tibial strut corticocancellous graft in the present scenario. Functional results were good and about 80 % comparable to the opposite thumb (80%) functions (pinching/grasping) in our case. He was able to performing all routine activities including writing and able to do daily routine work with no morbidity at graft harvesting site.
We did not find any documentation in medical literature contributing similar kind of segmental gap non-union in PP of thumb. Patankar et al. achieved complete remodeling and functional restoration over the 5 months in atrophic non-union of PP of thumb by using external fixator and while correcting corrected deformity gradually followed by bone grafting and compression with the similar fixator [3]. Applying and maintaining external fixator is a cumbersome and time-consuming procedure for small bones which may further increase stiffness of adjacent joints [2], [6]. Al-Qattan et al. documented union and adequate functional outcomes after bone grafting and fixation with K-wires in non-union of subcapital fracture of PP of thumb [4]. Both authors used iliac cancellous bone autograft for healing as there was not a substantial bone gap, while we harvested subperiosteal proximal tibial bone graft for filling segmental large bone gap at non-union site.
Gap non-union of phalanges of pediatric thumb is a rare entity and can be managed with corticocancellous grafting and fixation. Tibial strut corticocancellous graft can be used as a good osteoconductive, structural, and as well as osteoinductive option for this entity gap non-union in phalanx of child to achieve union. Good cosmetic and functional outcome can be achieved even in gap non-union of small bones of hand in children with no morbidity at graft harvesting site.
Post-traumatic gap non-union of the phalanx is a rare entity in children. Strut Tibial corticocancellous bone autograft and fixation with k-wires can be utilized adequately even in delayed presentation in this age group.
References
- 1.1. Douglas G. Smith MD. Grasping the importance of our hands. Motion 2006;16:1. [Google Scholar]
- 2.2. Feller R, Kluk A, Katarincic J. Pediatric phalanx fractures: Evaluation and management. In: Abzug J, Kozin S, Zlotolow D, editors. The Pediatric Upper Extremity. New York: Springer; 2015. [Google Scholar]
- 3.3. Patankar H, Patwardhan D. Nonunion in a fracture of the proximal phalanx of the thumb. J Orthop Trauma 2000;14:219-22. [Google Scholar]
- 4.4. Al-Qattan MM, Hashem FK, Rasool MN, Elshayeb A, Hassanain J. A unique fracture pattern of the proximal phalanx in children: Fractures through the phalangeal neck with an attached dorsal bony flange. Injury 2004;35:1185-91. [Google Scholar]
- 5.5. Al-Qattan MM, Cardoso E, Hassanain J, Hawary MB, Nandagopal N, Pitkanen J. Nonunion following subcapital (neck) fractures of the proximal phalanx of the thumb in children. J Hand Surg Br 1999;24:693-8. [Google Scholar]
- 6.6. Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: Preferred methods of stabilization. J Am Acad Orthop Surg 2008;16:586-95. [Google Scholar]
- 7.7. Swenson DM, Yard EE, Collins CL, Fields SK, Comstock RD. Epidemiology of US high school sports-related fractures, 2005-2009. Clin J Sport Med 2010;20:293-9. [Google Scholar]
- 8.8. Ozanne-Smith J. Child accident and injury prevention research in other than road accidents. Part 2: Finger Jam injuries to children in doors. (Monash University Accident Research Centre). Hazard 1993;14:6. [Google Scholar]
- 9.9. Boyer JS, London DA, Stepan JG, Goldfarb CA. Pediatric proximal phalanx fractures: Outcomes and complications after the surgical treatment of displaced fractures. J Pediatr Orthop 2015;35:219-23. [Google Scholar]
- 10.10. Stans AA. Complications of fractures in children. In: Mencio GA, Swiontkowski MF, editors. Green’s Skeletal Trauma in Children E-Book. 5th ed. Philadelphia, PA: Saunders, Elsevier Health Sciences; 2014. p. 119-21. [Google Scholar]
- 11.11. Vadivelu R, Dias JJ, Burke FD, Stanton J. Hand injuries in children: A prospective study. J Pediatr Orthop 2006;26:29-35. [Google Scholar]
- 12.12. Valencia J, Leyva F, Gomez-Bajo GJ. Pediatric hand trauma. Clin Orthop Relat Res 2005;432:77-86. [Google Scholar]
- 13.13. Chew EM, Chong AK. Hand fractures in children: Epidemiology and misdiagnosis in a tertiary referral hospital. J Hand Surg Am 2012;37:1684-8. [Google Scholar]
- 14.14. Nofsinger CC, Wolfe SW. Common pediatric hand fractures. Curr Opin Pediatr 2002;14:42-5. [Google Scholar]
- 15.15. Lindley SG, Rulewicz G. Hand fractures and dislocations in the developing skeleton. Hand Clin 2006;22:253-68. [Google Scholar]
- 16.16. Brinker MR, O’Connor DP. Nonunions: Evaluation and treatment. In: Browner BD, Jupiter JB, Krettek C, Anderson PA, editors. Skeletal Trauma. 5th ed. Philadelphia, PA: Elsevier, Saunders; 2015. [Google Scholar]