Prompt diagnosis and management of carpo-metacarpal fracture-dislocations can lead to favourable outcomes.
Dr. Nikhil Jawaharlal,
International Training Fellow, Department of Trauma and Orthopaedics,
Arrowe Park Hospital, Arrowe Park Road, Wirral – CH49 5PE, UK.
E-mail: nikenahar@gmail.com
Introduction: Carpo-metacarpal joint fracture-dislocations are rare injuries. They constitute less than 1% of all hand injuries [1]. They often go unnoticed [2]. Of these, dorsal fracture-dislocations on the ulnar side are more commonly seen [3] because of the greater stabilizing dorsal structures. Volar fracture-dislocations are very rare and difficult to diagnose for which, one should have a keen eye on.
Case Report: This is a case of a 51-year-old female with a closed injury to her wrist. With clinical suspicion and appropriate radiographs fracture-dislocation of the 4th and 5th carpometacarpal joints with volar displacement was diagnosed. She underwent closed reduction and percutaneous Kirschner wire fixation, followed by 6 weeks of immobilization. At the final follow-up in 4 months, the patient was noted to have a satisfactory outcome following intense physiotherapy.
Conclusion: Fourth and fifth carpometacarpal joint fracture-dislocations of the fingers are unique; their diagnosis can be challenging and often overlooked [4], which if missed can have very poor outcomes. The functional prognosis depends on the precocity of diagnosis and appropriate reduction and vigorous rehabilitation.
Keywords: Carpometacarpal joint, fracture-dislocation, volar displacement, wrist injury.
Carpometacarpal joint fracture-dislocations are relatively infrequent injuries. They represent <1% of all the hand and wrist injuries. These usually occur in young adults with an axial loading injury to their wrist or in the elderly population with a fall injury. The dislocations can be of mainly 3 types volar, dorsal, or at times divergent. The most common type is dorsal dislocation. The direction of force mostly determines the direction of dislocation. Another argument in favor of dorsal displacement is that the dorsal ligaments have static elements and wrist extensors which act as dynamic restraints causing the failure of bone dorsally, resulting in volar ligaments being ruptured [4]. These injuries gain significance because these can be easily missed [1] as they are not readily visible in AP views and one has to have a keen eye on the lateral view due to the overlapping of all the metacarpals. Untreated/ delayed treatment of carpometacarpal fracture-dislocations leads to poor functional outcomes and chronic residual pain. These also result in decreased grip strength and this is more so prominent if the dominant hand is involved. Thus, high-quality imaging with clinical suspicion can help us in identifying such injuries and prevent long-term functional distress to patients. The following case is presented to make aware of such injuries. Furthermore, a volar fracture-dislocation is not very common and suspicion should be kept in mind. McWhorter reported the first case in 1918 [5]. The following is a case of fracture-dislocation of the 4th and 5th carpometacarpal joint in a 51-year-old female and its clinical case details and evidence base are discussed.
This is a 51-year-old right-hand dominant female, who presented to the Emergency Department with pain and swelling to the right wrist after a history of fall. She had this fall while jogging, where she tripped and fell with an outstretched hand. It was an isolated injury and no other injuries were recorded.
On examination of her right wrist, there was obvious swelling to the ulnar side of the wrist. Some bruising was present on the palmar aspect on the ulnar side of the wrist. Specific tenderness was elicited on the hypothenar eminence as well on the ulnar corner of the wrist. Furthermore, the range of motion of the wrist was restricted because of pain. The neurovascular status was intact with no distal sensory loss and she had good distal circulation with palpable radial and ulnar pulse. Her finger movements were also satisfactory.
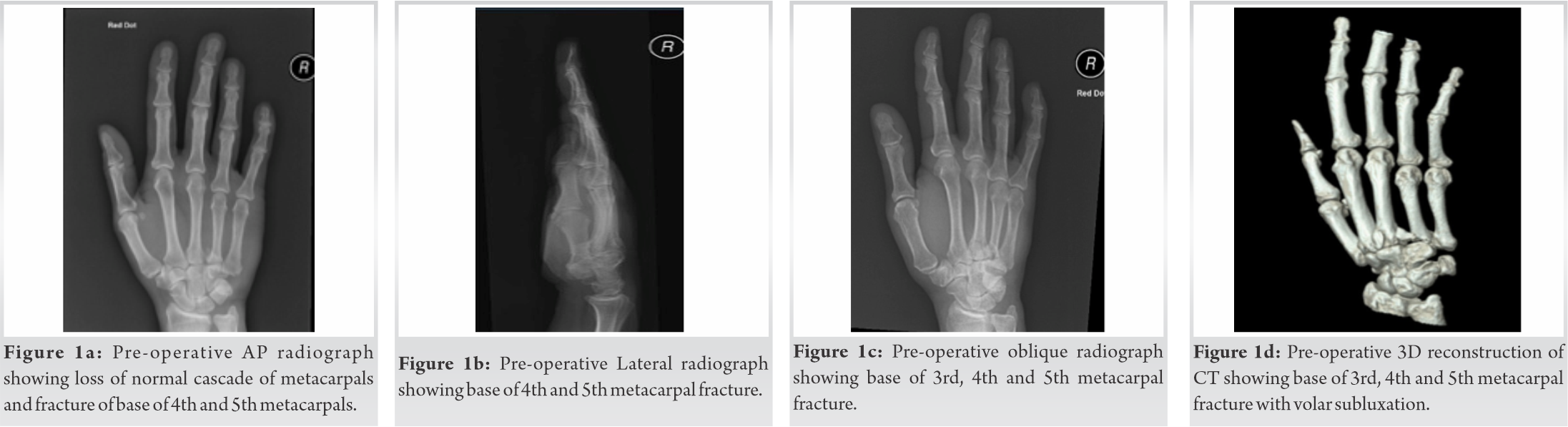
Based on the above history and clinical findings anteroposterior, lateral and oblique views of the wrist were taken. The radiographs (Fig. 1a-c) showed loss of normal metacarpal cascade and a fracture-dislocation of the 4th and 5th Carpometacarpal joint over the volar side. She was placed in an ulnar-gutter plaster of paris slab and was advised strict hand elevation while a CT scan was organized. The CT scan (Fig. 1d) confirmed the above findings along with undisplaced fractures of the 3rd metacarpal as well as the hamate bone. The 4th metacarpal had a displaced partial articular fracture of the base, associated with volar dislocation of the carpometacarpal joint. Whereas, the 5th metacarpal was just a pure volar dislocation. A decision was taken to operate on it keeping in line with the evidence, which shows chronic pain and poor functional outcome in untreated/delayed cases.
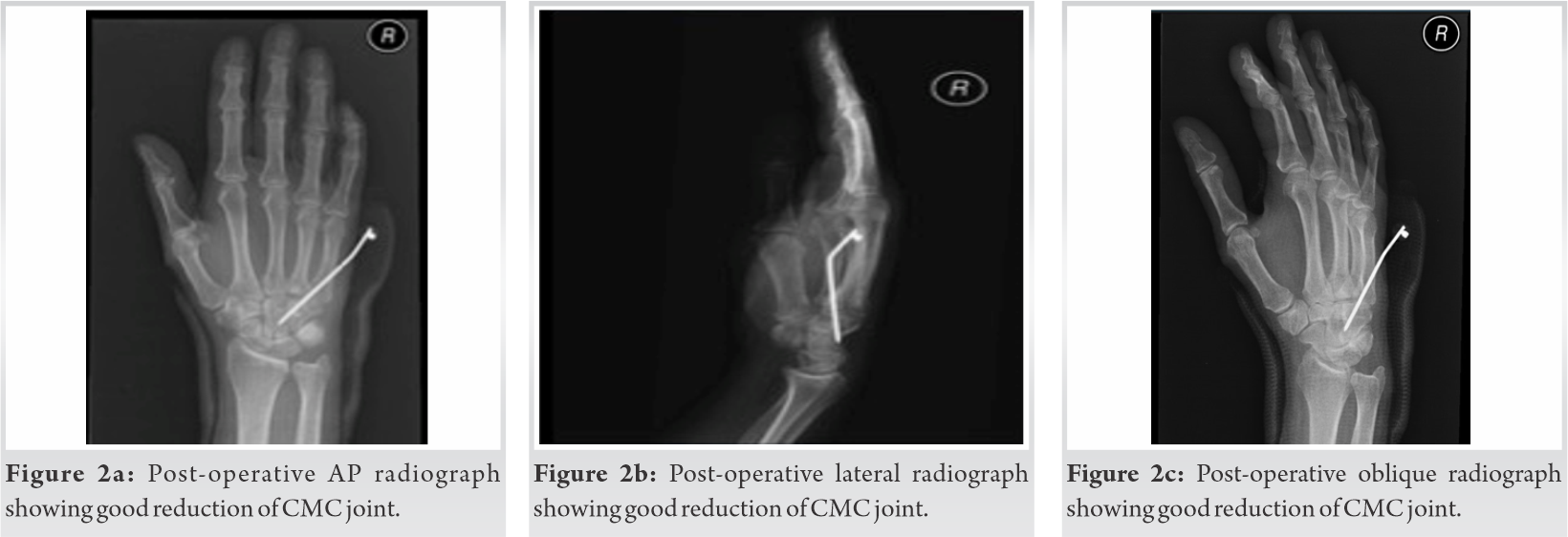
The treatment offered was closed/open reduction of the fracture-dislocation with fixation. In theatre, after appropriate traction and manipulation under anesthesia, under image intensifier, the fracture-dislocation was satisfactorily reduced in a closed manner and the 5th carpometacarpal joint was fixed with a single Kirschner wire. The 4th carpometacarpal joint also fell in place and was stable under image intensifier. The joint was well reduced in both the planes with the single wire and the fixation provided was deemed sufficient (Fig. 2a-c). She was placed in a below-elbow volar slab and was advised limb elevation along with active finger movements.
She was reviewed at 2 weeks and the X-rays showed satisfactory alignment. She was then referred to our hand therapists who then worked on her to improve her functional range of motion of the fingers and its strength. We reviewed her again at 4 weeks and the follow-up X-rays were satisfactory with no specific complaints.
At the end of 6 weeks, the follow-up radiographs were satisfactory and the Kirschner wire was removed in the outpatient department. The volar slab was also discarded. Her range of motion of wrist was good albeit some stiffness and there was minimal stiffness in her fingers. The carpometacarpal joint was also stable and she was told to resume her normal activities other than axial loading activities of her upper limb for another 4 weeks along with the involvement of hand therapists. The hand therapists initiated focused exercises with active-assisted wrist range of motion and strengthening exercises.
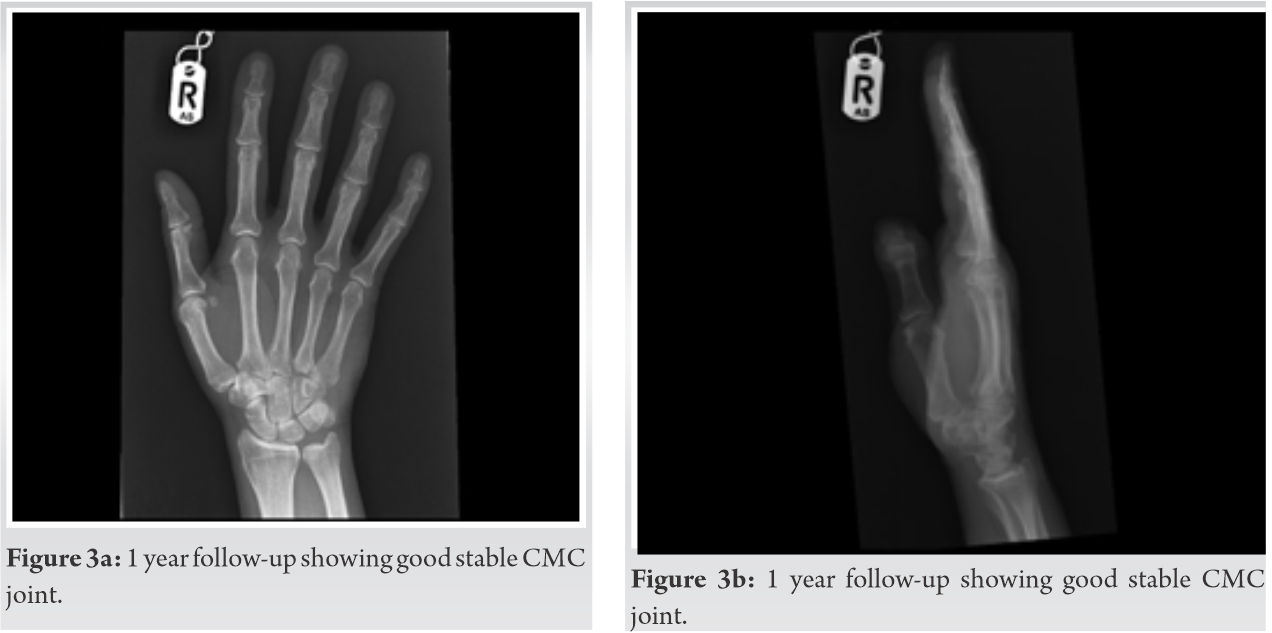
At one year follow-up, the check radiographs were satisfactory (Fig. 3a, 3b) and the patient was noted to have full range of wrist and finger movements with grip strength comparable to the contra-lateral side (Fig. 4a-f). She also went back to her pre-injury activity levels with no discomfort.
Carpometacarpal joint injuries are rare injuries associated with high local kinetic energy trauma [6]. They usually have an axial loading force on the joint of impact. Wedge articulation of the index metacarpal with the trapezium and trapezoid, and the “keystone” such as the articulation of the 3rd metacarpal with capitate gives its stability [7]. The rounded articulation of the 4th and 5th metacarpals with hamate gives rise to greater mobility and this prejudices these joints during trauma, leading to disruptions [8]. Overloading of the axial force through the fourth finger axis is transmitted to the carpus resulting in fracture and shortening of the metacarpals [9].
Fracture-dislocations can happen either dorsally or volarly. Most common are the dorsal side because of the direction of force of injury. Volar fracture-dislocations are very rare in occurrence. There have been only a few case reports of such injuries. In the acute presentation, the wrist at the ulnar side will be grossly swollen. Waugh and Yancy gave a classic description of this injury -as a “spade” type of deformity [10].
A careful neurologic evaluation is invaluable. Volar to the fifth carpometacarpal joint, lies the deep motor branch of the ulnar nerve. This then passes around the hook of the hamate. It is susceptible to injury in both dorsal and volar types of carpometacarpal fracture-dislocations [11]. This can in turn result in some muscle weakness of the medial interossei. There has also been a case report of acute carpal tunnel syndrome in a volar carpometacarpal dislocation.
Fifteen of the 21 patients in Henderson and Arafa series were missed initially in their case series report [2]. This highlights the fact that neglected and incorrect diagnoses are very frequent in metacarpal base injuries of the hand. A number of factors contributed to these delayed diagnoses. Some of them were due to inappropriate radiological reading, inferior quality of radiographs, and at times in the hands of an inexperienced resident. Cain et al. reported that oblique hand and wrist Xrays to be one of the best initial methods for assessment in 4th and 5th carpometacarpal joint injuries [12]. CT scans are the paramount modality to view these complex injuries. These scans gives us detailed view of the fracture-dislocations and their morphology, which will help us in planning the appropriate treatment modality. These also help in highlighting the other occult injuries, like hamate fractures.
Treatment of these injuries is still debatable because the literature consists chiefly of anecdotal reports or at the maximum a few studies containing small group of patients [8]. Steinmetz et al. have produced one of the largest retrospective reviews of carpometacarpal joint injuries [13]. They reported about 165 cases over a 10-year period spanning 2005 to 2015. Out of 165 patients, 164 of them had dorsal displacement and only one patient had volar displacement. Some people advocate that open reduction should be done in such fractures. In addition to this, there are minimal studies comparing different treatment methods in such injuries.
Even though many studies recommend open reduction and internal fixation in cases of fracture-dislocation, in this case, we got satisfactory reduction with closed manipulation and we were able to maintain the reduction with pinning. This was more so possible because of the early diagnosis and management in this patient. Studies indicate that patients taken to theater in the initial ten days of injury have more chances of having a closed procedure. Open reduction has its own advantages of direct vision, drainage of local hematoma, and also prevention of tendons being transfixed [14] but if closed reduction is possible- it has tremendous advantages in reducing post-operative morbidity and facilitating speedy rehabilitation.
Physiotherapy of hand and wrist joints is an indispensable part of this injury management to circumvent postoperative stiffness. Feehan recently emphasized that early controlled mobilization of the hand was essential to reduce post-injury complications of the hand [15]. Several complications have been reported in the literature in mis-managed cases, including residual hand pain, stiffness, decrease in gripping power, persistent subluxations, and at times, secondary displacements. Complications can also arise as a result of prolonged immobilization, namely stiffness of small joints in the hand, tendon adhesions, and muscle weakness. Dowden meanwhile has highlighted that early controlled motion must be balanced with necessary immobilization at areas of injury (i.e., fractures and dislocations) [16]. This will ensure that satisfactory healing ensues.
Volar carpometacarpal fracture-dislocations are uncommon injuries. Missing such injuries can lead to serious functional restriction, especially if the dominant hand is involved. Meticulous examination and high-quality radiographs with suspicion can lead to early diagnosis and appropriate management of such cases. These are unstable injuries, which can be treated by closed or open reduction, but fixation will be necessary. Active hand rehabilitation is a key to good functional recovery.
Volar carpometacarpal dislocations are very rare injuries and diagnosis can be difficult. Loss of normal metacarpal cascade in radiographs should prompt further imaging that can lead to an early diagnosis and appropriate management favoring a good outcome.
References
- 1.Sharma AK, John JT. Unusual case of carpometacarpal dislocation of all the four fingers of ulnar side of hand. Med J Armed Forces India 2005;61:188-9. [Google Scholar]
- 2.Henderson JJ, Arafa MA. Carpometacarpal dislocation: An easily missed diagnosis. J Bone Joint Surg Br 1987;69:212-4. [Google Scholar]
- 3.Prokuski LJ, Eglseder WA Jr. Concurrent dorsal dislocations and fracture-dislocations of the index, long, ring, and small (second to fifth) carpometacarpal joints. J Orthop Trauma 2001;15:549-54. [Google Scholar]
- 4.Hani R, Jeddi I, Berrada MS. Divergent dislocation of the carpometacarpal joints: A case report. J Med Case Reports 2018;12:157. [Google Scholar]
- 5.McWhorter GL. Isolated and complete dislocation of the fifth carpometacarpal joint: Open operation. Surg Clin Chicago 1918;2:793-6. [Google Scholar]
- 6.Mabee JR, Lee TJ, Halus S. Dorsal dislocation of the four ulnar metacarpals. Am J Emerg Med 1997;15:408-11. [Google Scholar]
- 7.Yoshida R, Shah MA, Patterson RM, Buford WL Jr., Knighten J, Viegas SF. Anatomy and pathomechanics of ring and small finger carpometacarpal joint injuries.J Hand Surg Am 2003;28:1035-43. [Google Scholar]
- 8.Vandeweyer E, Botero L, Coessens BC. Dorsal carpometacarpal dislocation of ulnar fingers. A case report. Acta Chirurgica Belgica 2002;102:279-80. [Google Scholar]
- 9.Kural C, Başaran SH, Ercin E, Bayrak A, Bilgili MG, Baca E. Fourth and fifth carpometacarpal fracture dislocations. Acta Orthop Traumatol Turc 2014;48:655-60. [Google Scholar]
- 10.Waugh RL, Yancey AG. Carpometacarpal dislocations. J Bone Joint Surg 1948;30:397-404. [Google Scholar]
- 11.Domingo A, Font L, Saz L, Arandes JM. Isolated radial palmar dislocation of the fifth carpometacarpal joint with ulnar neuropathy assoc iated: Successful treatment with closed reduction and internal fixation. Eur J Orthop Surg Traumatol 2009;19:101-7. [Google Scholar]
- 12.Cain JE Jr., Shepler TR, Wilson MR. Hamatometacarpal fracture-dislocation: Classification and treatment. J Hand Surg Am 1987;12:762-7. [Google Scholar]
- 13.Steinmetz G, Corning E, Hulse T, Fitzgerald C, Holy F, Boydstun S, et al. Carpometacarpal fracture-dislocations: A retrospective review of injury characteristics and radiographic outcomes. Hand (N Y) 2021;16:362-7. [Google Scholar]
- 14.Pundkare GT, Patil AM. Carpometacarpal joint fracture dislocation of second to fifth finger. Clin Orthop Surg 2015;7:430-5. [Google Scholar]
- 15.Feehan LM. Early controlled mobilization of potentially unstable extra-articular hand fractures. J Hand Ther 2003;16:161-70. [Google Scholar]
- 16.Dowden JW. The principle of early active movement in treating fractures of the upper extremity. 1924. Clin Orthop Relat Res 2006;442:83-6 [Google Scholar]