Cutibacterium Acnes is increasingly identified as a pathogen involved in prosthetic joint infections, and positive isolated cultures must be interpreted with great caution and treated adequately.
Dr. Yuen Wen Loong Paul, Department of Orthopaedic Surgery, Changi General Hospital, Singapore. E-mail: Paulyuen.nushs@gmail.com
Introduction:Hip bipolar hemiarthroplasty is commonly done for elderly patients who suffer from femoral neck fractures, with good functional outcomes. Prosthetic acetabular protrusio is a rare complication following bipolar hemiarthroplasty and can occur in prosthetic joint infections (PJIs) due to destructive osteolysis and resorption of surrounding bone. Among PJI pathogens, Cutibacterium acnes is increasingly being implicated. In our paper, we review the current literature of C. acnes PJIs and report a unique case of C. acnes infection of hip bipolar hemiarthroplasty complicated by protrusio acetabuli.
Case Report:The patient is a 77-year-old Asian-Chinese man who suffered from left hip pain 10 years after bipolar hemiarthroplasty surgery. Radiographic evaluation showed acetabular protrusio with extensive femoral osteolysis. Subsequent intraoperative cultures revealed C. acnes infection. The patient successfully underwent antibiotic treatment and a two-staged revision total hip arthroplasty.
Conclusion:C. acnes is an increasingly recognized cause of PJIs and can cause significant morbidity. It should not be simply regarded as a contaminant of tissue or cultures. C. acnes PJIs require antibiotic treatment and early surgery with debridement and revision. This reported case presented technical challenges due to the infection resulting in prosthetic acetabular protrusio.
Keywords:Bipolar hemiarthroplasty, protrusio acetabuli, Cutibacterium acnes.
Bipolar hemiarthroplasty and total hip arthroplasty are widely accepted treatment options for displaced femoral neck fractures in the elderly with good functional outcomes [1]. Total hip arthroplasties have better functional outcomes and lower revision rates while hemiarthroplasties are preferred for lower dislocation rates and faster operative timings [2]. With an ever-aging population, there are increasing numbers of hip arthroplasties done, with longer prosthesis implantation times [3]. Naturally, there are higher numbers of prosthesis failures of which a significant portion is secondary to prosthetic joint infections (PJIs). It is imperative to diagnose PJIs as treatment strategies are profoundly different, and misdiagnosis will lead to relapse of untreated infection and prosthetic failures [3].
Acetabular protrusio is an uncommon cause of bipolar hemiarthroplasty failure. It is thought to happen in PJIs due to destructive osteolysis and resorption of surrounding bone resulting in loss of bony structure and prosthetic migration [4, 5, 6]. Surgical intervention is typically challenging, due to the possible involvement of intrapelvic vital structures including the external iliac vessels and femoral nerve, and scarring of the protruded prosthesis [4].
Among the typical pathogens causing PJIs, Cutibacterium acnes, formerly Propionibacterium acnes, is increasingly being found. C. acnes is a slow-growing, anaerobic, Gram-positive rod-shaped bacterium. It is part of normal flora of the skin, found in pilosebaceous follicles. It has been shown to persist even with adequate pre-operative skin antiseptic procedures and antibiotics [7, 8].
It is an opportunistic pathogen and can be associated with PJIs through biofilm production [9, 10]. It has low virulence and typically only results in symptoms and signs of infection months to years after surgery [9, 11]. A study by Rienmuller showed a median time from prosthesis implantation to PJI diagnosis of 44.2 months with majority diagnosed either delayed (>3 months) or late (<24 months) [11].
Recent research suggests that infections caused by C. acnes account for a larger percentage of PJIs than assumed, thought to be because of difficulties in culturing the bacteria, misinterpretation of positive results as contamination, and previously limited knowledge regarding the pathogenicity of the bacteria [12]. C. acnes has a higher incidence in prosthetic shoulder infections, but is also increasingly found in hip arthroplasties [11]. Patients with C. acnes PJIs typically present with symptoms such as pain and stiffness, and other signs such as persistent sinus tract formation or radiological loosening of implant are less common [12]. Their non-specific presentation coupled with difficulties with cultivating the bacterium on cultures make C. acnes PJIs a diagnostic challenge.
The gold standard of C. acnes PJI treatment has not been established, but current strategies typically involve eradication of the infection with antibiotic treatment and early surgery with debridement and revision (one or two staged) [10, 13].
In our paper, we review the current literature of C. acnes PJIs and report a case of C. acnes infection of hip bipolar hemiarthroplasty complicated by protrusio acetabuli. Initial intraoperative culture specimens were negative at 48 h, but two samples grew C. acnes after undergoing extended culture. The patient successfully underwent eradication of the bacteria and eventually underwent a two-staged revision total hip arthroplasty. To the best of our knowledge, this is the first reported case of C. acnes PJI resulting in bipolar hemiarthroplasty protrusio acetabuli.
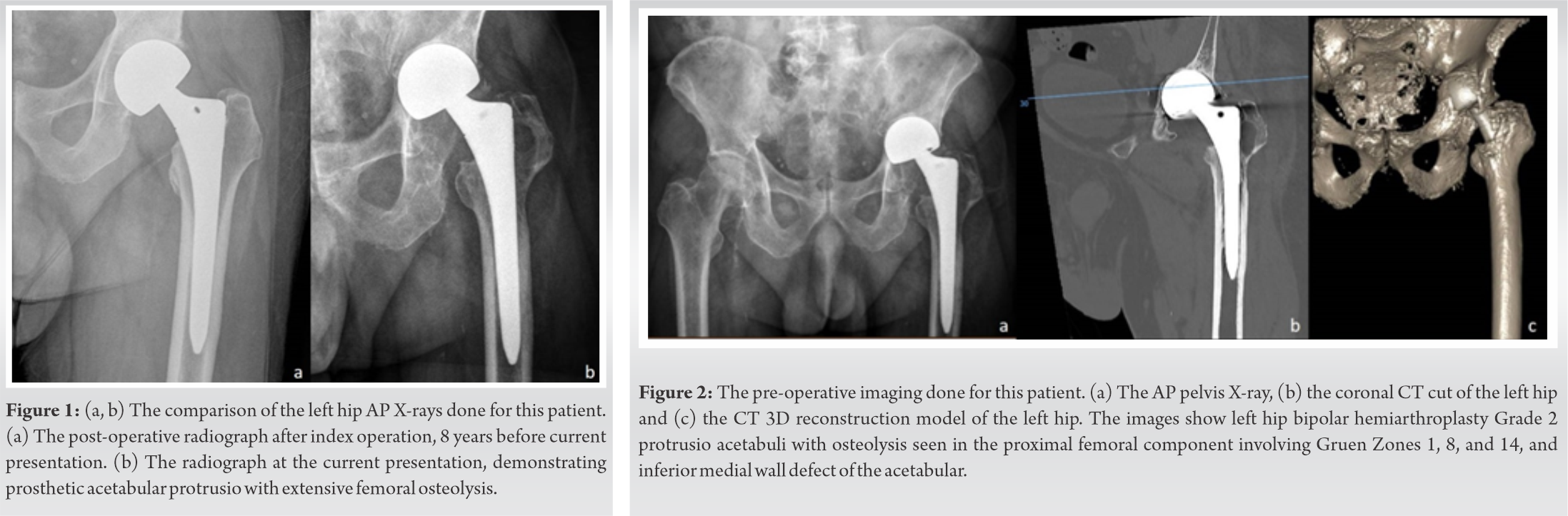
The patient was a 77-year-old Asian-Chinese ambulant retiree with comorbid of hypertension, dyslipidemia, and ischemic heart disease. He had a significant history of left hip bipolar hemiarthroplasty done in 2010 for left femoral neck fracture sustained after a mechanical fall. He was followed until 2012 where he was asymptomatic and recovering well, after which he defaulted follow-up. (Fig. 1a) shows the X-ray of his hip bipolar hemiarthroplasty at his last visit.
He presented again in May 2020 due to worsening left hip pain for a few months with noted shortening of his left leg. He denied any fever, falls, or trauma.
Clinical examination showed 10° of fixed flexion deformity over his left hip with profound stiffness in internal and external rotation of his hip. He did not have elevated temperature, wound breakdown, or sinus tracts noted.
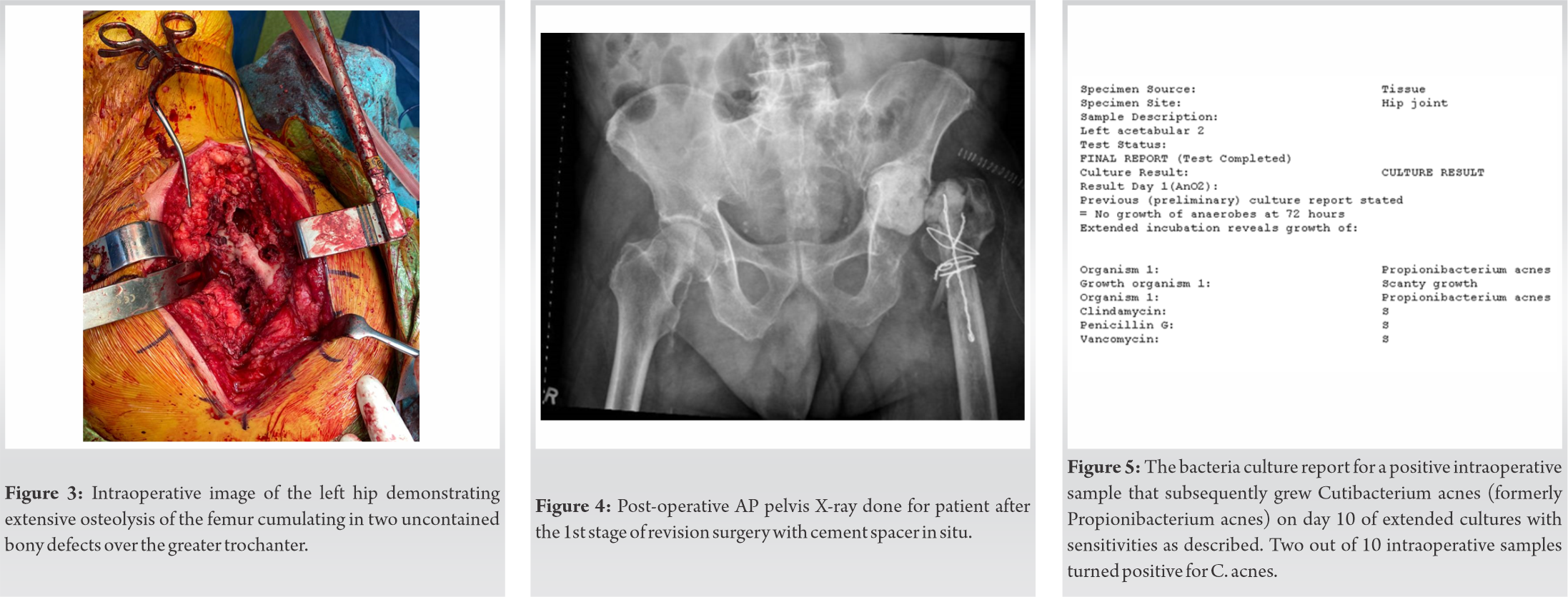
X-ray and subsequent computer tomographic (CT) evaluation showed left hip bipolar hemiarthroplasty Grade 2 (Sotelo-Garza and Charnley classification) protrusio acetabuli, osteolysis seen in the proximal femoral component involving Gruen zones 1, 8, and 14 with lateral cortical body defect (Fig. 1b and 2). Biochemical evaluation showed white cell count of 8.1 × 103/uL, ESR of 80 mm/hr, and CRP of 7.6 mg/L. Initial CT-guided left hip biopsy and sampling showed granulation tissue with no evidence of malignancy, and negative Gram stains and cultures.
In view of high index of suspicion of PJI, the patient underwent two-stage revision surgery. The first stage of the surgery involved removal of the left hip bipolar implant, debridement of biofilm, and insertion of cement spacer. The patient was positioned lateral, with posterior approach used over the previous incision scar. Intraoperative findings showed two uncontained bony defects over the greater trochanter, extensive granulation over the acetabulum and femoral canal, and intact acetabular rim with inferior medial wall defect (Fig. 3).
The femoral stem was retrieved, and vancomycin-impregnated cement spacer was inserted into the acetabulum and cement dowel into the femoral canal (Fig. 4). Intraoperative cultures subsequently grew C. acnes on day 10 of extended cultures (2 out of 10 cultures, Fig. 5), sensitive to penicillin G (MIC < 0.016), clindamycin (MIC < 0.016), vancomycin (MIC < 0.5), and rifampicin (MIC < 0.002). Infectious disease specialist was consulted, and joint decision made to cover with 6 weeks of intravenous penicillin G monotherapy.
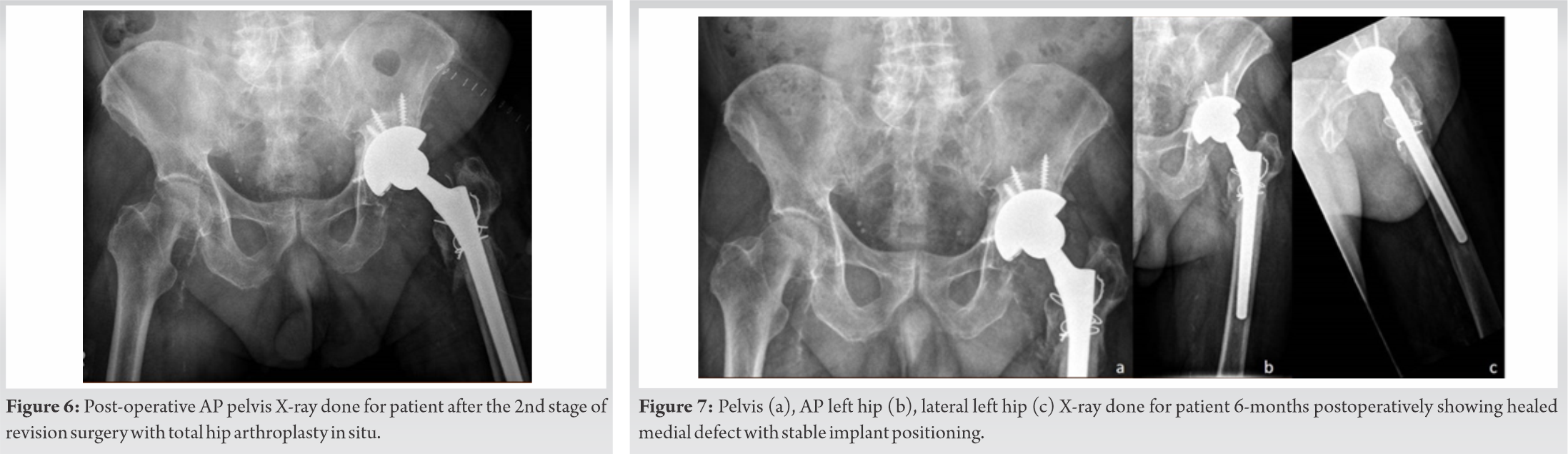
Interval CT-guided left hip biopsy was taken after antibiotics course which demonstrated negative cultures. The patient subsequently underwent 2nd stage surgery 3 months after the 1st stage, through posterior approach. The cement spacers were removed, redebrided and washout was performed. Acetabular wall medial defect was filled with cancellous bone chips, reversed reamed, and fitted with Trabecular Metal™ Acetabular Revision System cup (Zimmer Biomet) though jumbo cup technique, augmented with four screws. Femur shaft was reamed and Wagner Revision Hip Stem and femoral head inserted (Zimmer Biomet) (Fig. 6). The patient recovered well and was discharged 2 weeks post-operative.
He was reviewed 6-month postoperatively where he was recovering well, walking full weight on his left hip with healed wounds. Serial X-ray monitoring showed healed medial defect with stable implant positioning (Fig. 7).
The frequency of PJI continues to rise as more and more arthroplasty surgeries are done for an increasingly elderly population. Among the routinely involved bacterium, C. acnes has been increasingly recognized as a pathogen involved in PJIs, up to about 10% of PJIs in recent studies [10].
C. acnes-associated PJIs continue to be a challenge to diagnose and treat. It has an indolent and non-specific clinical presentation, with symptoms of pain and stiffness as main complains, difficult to differentiate from normal post-operative pain, and stiffness. Biochemical markers such as CRP and leukocytosis are also generally not useful, as they are often not markedly raised [10].
C. acnes is known to be a slow-growing bacterium, difficult to culture and identify. Longer culture incubation times up to 15 days and sonication of removed implants are strategies to improve detection [11, 12]. It is recommended to take at least three samples, and optimally more than 5–6 periprosthetic intraoperative tissues for culture to improve the diagnostic rates and exclusion of contamination from skin. In our case, the cultures only returned positive on day 10 of extended cultures.
Isolation of C. acnes from cultures must be interpreted with great caution instead of empirically labeling as a contaminate of tissue or cultures. C. acnes has been increasingly recognized as a pathogen involved in PJIs and can result in significant soft-tissue damage and unstable implants [10, 12]. Correlation with clinical and histopathological criteria is critical when reviewing positive cultures for C. acnes [14]. In our case, C. acnes was the implicated pathogen resulting in extensive femur and acetabular osteolysis and ultimately acetabular protrusio.
Till date, there is not clear guideline with regard to the management of C. acnes PJI. Treatment generally follows the principles of PJI management including antibiotic treatment and early surgery with debridement and revision. Conservative managements may be considered for cases up to 1 month from contamination.
C. acnes is typically susceptible to a wide spectrum of antibiotics including beta-lactams, quinolones, clindamycin, and rifampicin [15]. Recent study by Khassebaf et al. showed that combination antimicrobial therapy was generally not synergistic and had an indifferent effect on isolates of C. acnes, and combination therapy with rifampicin with benzylpenicillin had an additive effect [9, 12]. Resistance to clindamycin is also shown to be increasing [16]. The current studies suggest a course of 3–6 months of total antibiotic treatment with 2–6 weeks of intravenous antibiotics, with present IDSA guidelines recommending 4–6 weeks of initial treatment with either penicillin G or ceftriaxone monotherapy [16, 17].
Cornerstones of surgical treatment include clearance of biofilm, irrigation, debridement, and synovectomy, and either one- or two-staged implant revision [10, 13]. Studies have shown about 86% success rates for the treatment of C. acnes PJI, comparable to PJIs caused by other pathogens [10, 18].
There is no definitive evidence to favor single- versus two-staged revision procedures, but two-staged procedures are more favored for chronic difficult to treat cases, especially for concerns of wound complexity and soft-tissue involvement in protrusio cases [6, 19].
Implant acetabular protrusio cases are technically challenging, as there is often extensive scarring of the protruded implants and possible involvement of the intrapelvic structures such as external iliac artery and femoral nerve [4]. This makes pre-operative imaging of the pelvic structures important, including obtaining CT scans of the pelvis and femoral angiogram. Other key considerations for protrusio cases include the need for bone grafting the medial acetabular defect to restore bone stock and provide medial buttress for the acetabular cup. In this case, the defect was anteromedial, and there was sufficient rim to accept a hemispherical cup. The senior author decided to fill the defect with cancellous bone chips and used a large trabecular metal hemispherical cup for his reconstruction. The cup integrated successfully at 6 months and the patient was able to full weight-bearing and regain his mobility.
In our case report, we describe the successful treatment of a rare case of C. acnes PJI resulting in bipolar hemiarthroplasty acetabular protrusio through two-staged revision surgery and antibiotic treatment.
PJIs continue to increase as more arthroplasty surgeries are done for an increasingly elderly population. We report a PJI case which contributes to literature on C. acnes infections and prosthetic acetabular protrusio.
C. acnes is increasingly recognized as a pathogen involved in PJIs and can cause extensive soft-tissue damage and unstable implants. Positive isolated cultures from periprosthetic tissue should not be simply labeled as a contaminant and must be correlated to the clinical and histopathological picture.
References
- 1.Wang F, Zhang H, Zhang Z, Ma C, Feng X. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: A meta-analysis. BMC Musculoskelet Disord 2015;16:229. [Google Scholar]
- 2.Fahad S, Khan MZ, Aqueel T, Hashmi P. Comparison of bipolar hemiarthroplasty and total hip arthroplasty with dual mobility cup in the treatment of old active patients with displaced neck of femur fracture: A retrospective cohort study. Ann Med Surg 2019;45:62-5. [Google Scholar]
- 3.Portillo ME, Salvadó M, Alier A, Sorli L, Martínez S, Horcajada JP, et al. Prosthesis failure within 2 years of implantation is highly predictive of infection. Clin Orthop Relat Res 2013;471:3672-8. [Google Scholar]
- 4.Stiehl JB. Acetabular prosthetic protrusion and sepsis. Case report and review of the literature. J Arthroplasty 2007;22:283-8. [Google Scholar]
- 5.Adenikinju A, Slover JD, Egol KA. Rapid acetabular chondrolysis following hemiarthroplasty of the hip: A poor prognostic sign. Case Rep Orthop 2019;2019:7328526. [Google Scholar]
- 6.Lim JB, Ang CL, Pang HN. Acetabular prosthetic protrusio after bipolar hemi-arthroplasty of the hip: Case report and review of the literature. J Orthop Case Rep 2016;6:28-31. [Google Scholar]
- 7.Phadnis J, Gordon D, Krishnan J, Bain GI. Frequent isolation of Propionibacterium acnes from the shoulder dermis despite skin preparation and prophylactic antibiotics. J Shoulder Elbow Surg 2016;25:304-10. [Google Scholar]
- 8.Renz N, Mudrovcic S, Perka C, Trampuz A. Orthopedic implant-associated infections caused by Cutibacterium spp.-A remaining diagnostic challenge. PLoS One 2018;13:e0202639. [Google Scholar]
- 9.Khassebaf J, Hellmark B, Davidsson S, Unemo M, Nilsdotter-Augustinsson Å, Söderquist B. Antibiotic susceptibility of Propionibacterium acnes isolated from orthopaedic implant-associated infections. Anaerobe 2015;32:57-62. [Google Scholar]
- 10.Boisrenoult P. Cutibacterium acnes prosthetic joint infection: Diagnosis and treatment. Orthop Traumatol Surg Res 2018;104:S19-24. [Google Scholar]
- 11.Rienmüller A, Borens O. Propionibacterium prosthetic joint infection: Experience from a retrospective database analysis. Eur J Orthop Surg Traumatol 2016;26:429-34. [Google Scholar]
- 12.Zappe B, Graf S, Ochsner PE, Zimmerli W, Sendi P. Propionibacterium spp. in prosthetic joint infections: A diagnostic challenge. Arch Orthop Trauma Surg 2008;128:1039-46. [Google Scholar]
- 13.Lavergne V, Malo M, Gaudelli C, Laprade M, Leduc S, Laflamme P, et al. Clinical impact of positive Propionibacterium acnes cultures in orthopedic surgery. Orthop Traumatol Surg Res 2017;103:307-14. [Google Scholar]
- 14.Aubin GG, Portillo ME, Trampuz A, Corvec S. Propionibacterium acnes, an emerging pathogen: From acne to implant-infections, from phylotype to resistance. Med Mal Infect 2014;44:241-50. [Google Scholar]
- 15.Crane JK, Hohman DW, Nodzo SR, Duquin TR. Antimicrobial susceptibility of Propionibacterium acnes isolates from shoulder surgery. Antimicrob Agents Chemother 2013;57:3424-6. [Google Scholar]
- 16.Achermann Y, Goldstein EJ, Coenye T, Shirtliffa ME. Propionibacterium acnes: From commensal to opportunistic biofilm-associated implant pathogen. Clin Microbiol Rev 2014;27:419-40. [Google Scholar]
- 17.Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, et al. Diagnosis and management of prosthetic joint infection: Clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis 2013;56:1-25. [Google Scholar]
- 18.Jacobs AM, van Hooff ML, Meis JF, Vos F, Goosen JH. Treatment of prosthetic joint infections due to Propionibacterium. Acta Orthop 2016;87:60-6. [Google Scholar]
- 19.Gramlich Y, Hagebusch P, Faul P, Klug A, Walter G, Hoffmann R. Two-stage hip revision arthroplasty for periprosthetic joint infection without the use of spacer or cemented implants. Int Orthop 2019;43:2457-66. [Google Scholar]