The technique of fashioning osteochondral allograft described in our case series can provide good graft incorporation and functional outcome in patients with Reverse Hill Sach’s lesion.
Dr. Vivek Dubey, Department of Trauma and Orthopaedics, Watford General Hospital, West Hertfordshire Hospitals NHS Trust, Watford, United Kingdom. E-mail: vvk7878@gmail.com
Introduction:Posterior glenohumeral joint dislocations with associated bony lesions are challenging to treat; namely, reverse Hill-Sachs’s lesions increase humeral head excursion predisposing to recurrent dislocations. To add to the complexity of management, posterior shoulder dislocations are often missed on plain radiographs, leading to chronicity in presentation.
Case Report:We describe here our technique in our case series of three patients. Case I, 32 years, gentleman, presented 3 days after injury. He had a locked posterior dislocation of shoulder which he sustained while he fell asleep and hit a glass table. Shoulder was not reducible in emergency department. Reverse Hill- Sachs’s lesion involved 40% of humeral head. Case II, a 54- years- old gentleman, a keen gym trainer . Following sudden withdrawal of diazepam, he woke up lying on the floor and started experiencing shoulder pain. He presented a week following the injury. The dislocated shoulder could not be reduced in emergency department. Bony defect involved 50% of humeral head. Case III, 45 years gentleman who fell off from bike, presented on the same day to the emergency department. The dislocated shoulder was reduced. Defect size was 40% of humeral head. A thorough physical and radiological examination was performed to evaluate the lesion. Delto-pectoral approach was utilized for surgical exposure. Once fully assessed, the lesion is outlined and an oscillating saw is used to create uniform edges - – a regular “orange slice”- shaped defect. The prepared defect size is measured. Calcium phosphate cement is used to fill the defect and form a mould that represents the dimensions of allograft required to recreate the native sphericity of the humeral head. This mould then acts as a reference when fashioning the osteochondral femoral allograft to make sure this fits the defect anatomically. Once the graft is prepared, it is placed into the defect in the correct orientation and fixed in situ using headless screws. We utilized the same technique in all our patients.
Conclusion:Reconstruction with osteochondral allograft is a promising technique to help shoulder surgeons achieve good outcomes for these patients. We propose a novel technique for fashioning allograft to anatomically fill the defects from bone loss, aiming to restores the native sphericity of the humeral head.
Keywords:Reverse Hill- Sachs’'s lesion, posterior glenohumeral dislocation, osteochondral, allograft.
Posterior dislocations of shoulder are uncommon, constituting only 2–4% of glenohumeral dislocations and are often missed [1, 2]. About 50% of these occur with an impaction fracture of the anteromedial aspect of the humeral head (reverse Hill-Sachs lesion or McLaughlin lesion) [3, 4]. These bony defects in the humeral head can lead to refractory glenohumeral instability. Increasing sizes of defect are increasingly challenging to manage [5, 6].
Treatment options for smaller lesions include transfer of the subscapularis tendon alone (McLaughlin) or with the lesser tuberosity along with the anterior capsular attachments (modified McLaughlin), to fill the bony defects [7]. For large, engaging reverse Hill-Sachs lesions involving more than 40% of the humeral head, hemiarthroplasty can be used in suitable patients [8].
Larger lesions up to 40% of the humeral head articular surface, especially in younger patients, can fall between the groups described above, leaving surgeons with some uncertainty about optimal management. However, in this group, reconstruction with osteochondral allograft is a promising operative solution [9]. The allograft can be from femoral head, humeral head, or talus [10, 11]. It is challenging to restore the sphericity of native humeral head with this allograft of variable source and dimensions. We present our surgical technique in fashioning the allograft in a way that best restores the native humeral head.
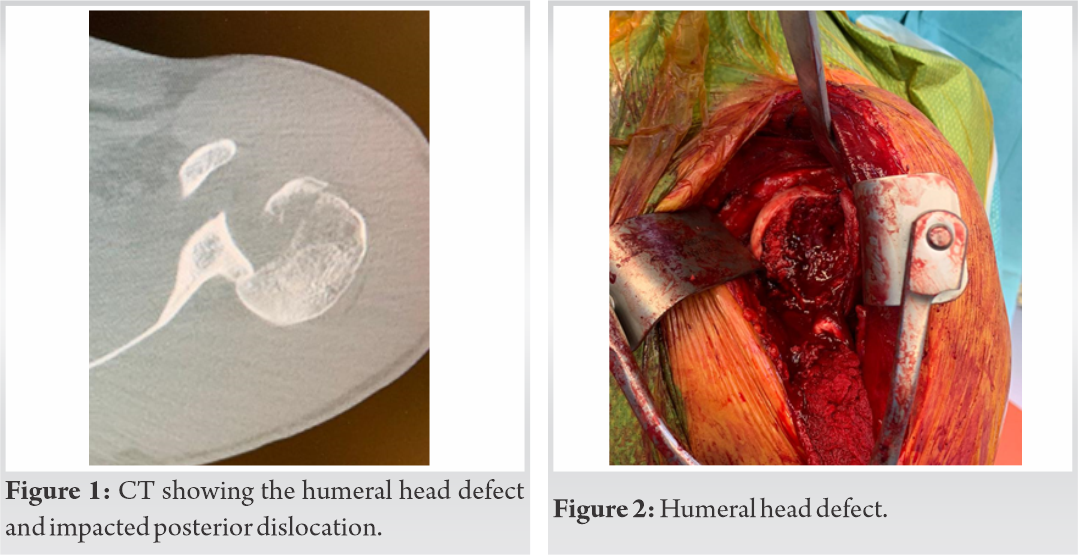
A physical examination of the shoulder is performed preoperatively. Apprehension in abduction is suggestive of a bony lesion. A comprehensive radiographic evaluation using X-ray, CT (Fig. 1), and MRI is conducted preoperatively to accurately evaluate the presence, volume, and orientation of the reverse Hill-Sachs lesion.
Our patients are given a general anesthetic, then placed in the beach chair position. An examination under anesthetic is performed to establish range of motion, the degree of instability, and the point of engagement of the reverse Hill-Sachs lesion. The shoulder is prepared and draped in a sterile fashion. A deltopectoral approach is used, through a 7 cm incision from the coracoid process extended distally. This is followed by dissection through subcutaneous tissue then fascia.
Establishment of the deltopectoral interval is facilitated by identification of the cephalic vein, coracoid, and the conjoint tendon. Tracing the conjoint tendon distally reveals an inverted V-shaped interval between pectoralis major and deltoid. The interval between the deltoid and pectoralis is then developed by blunt dissection. The distal attachment of pectoralis major is divided in its upper one-third.
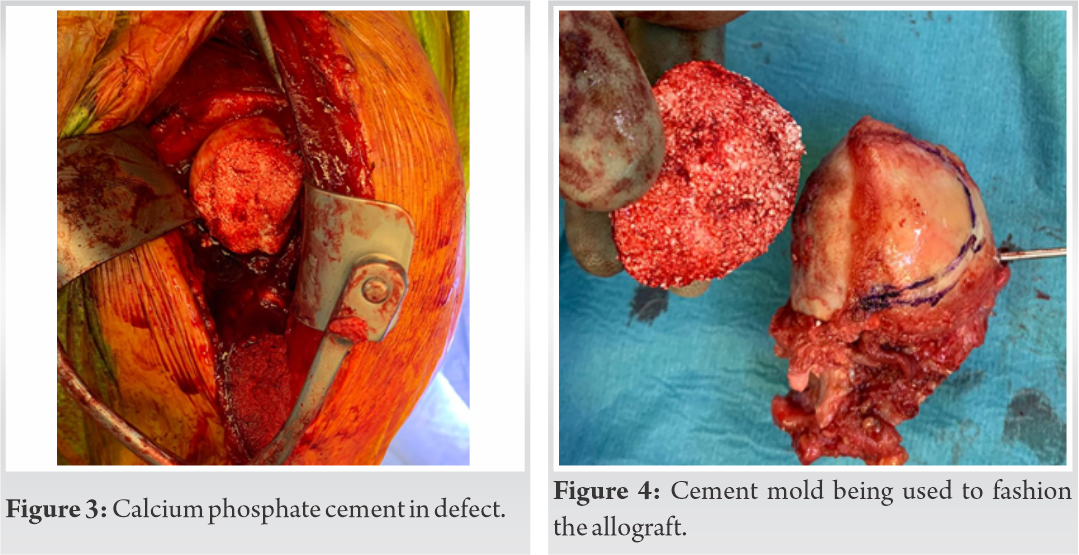
The superior one-third to one-half of the subscapularis tendon is identified and reflected off the bone. It is then then tagged with a 2 Vicryl suture to facilitate repair when closing. Finally, a T-shaped capsulotomy is performed to expose the humeral head and to visualize and evaluate the defect. Evaluation of the Hill-Sachs lesion (Fig. 2) is facilitated by placement of the shoulder in abduction and external rotation.
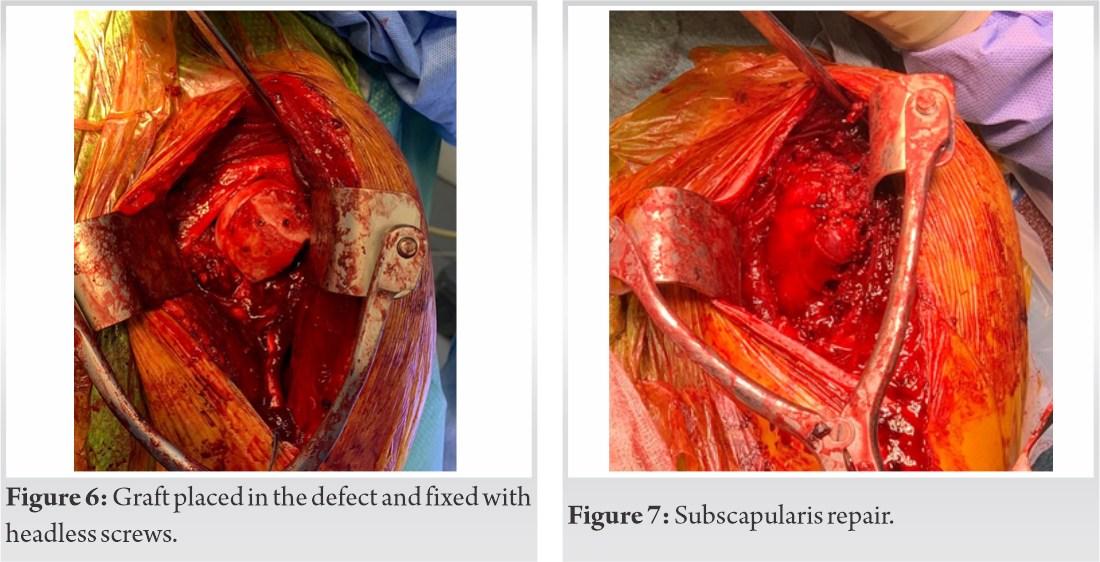
Once fully assessed, the lesion is outlined and an oscillating saw is used to create uniform edges – a regular “orange slice”-shaped defect. The prepared defect size is measured with a ruler, including width, length, and depth. In our case example, the width, length, and depth of the lesion measured 17 mm × 38 mm × 12 mm, respectively. Calcium phosphate cement is used to fill the defect and form a mold that represents the dimensions of allograft required to recreate the native sphericity of the humeral head (Fig. 3).
This mold then acts as a reference when fashioning the osteochondral femoral allograft (Fig. 4, 5) to make sure this fits the defect anatomically.
The goal of reconstruction is to recreate a smooth articular surface and fill the reverse Hill-Sachs defect. Once fixation is complete, leveling between the graft and native humeral head is verified to ensure complete anatomic restoration throughout shoulder range of motion. Internal and external rotation of the shoulder is performed to confirm optimal positioning of the graft. The partially detached subscapularis tendon is identified by the tagging stitch, and the subscapularis is repaired through use of a double-row technique along with anterior capsule (Fig. 7).
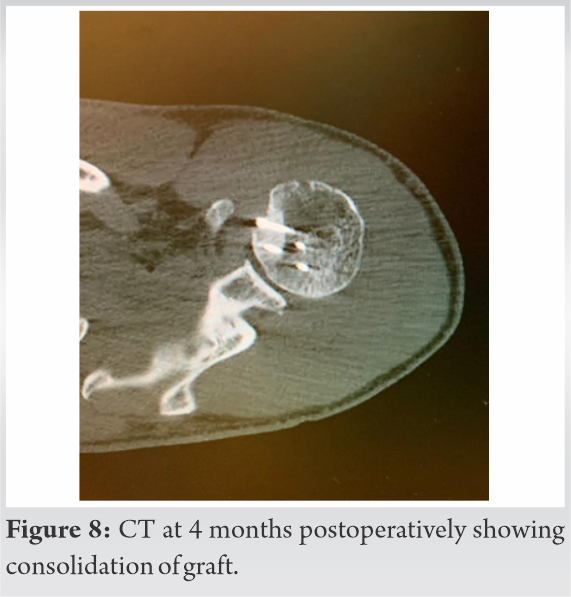
CT scan was done for patient at 6 months following the procedure, showing a near full incorporation of the allograft. The patients were followed up at 2 weeks after surgery for wound review, then at 6 weeks, 3 months, 6 months, and 18 months to assess their progress throughout the process of rehabilitation. We used the following physiotherapy protocol for our patients –
First 2 weeks: Only elbow and wrist exercise
2nd–6th weeks: Passive assisted flexion to 90° and external rotation up to 30°
After 6 weeks: Full gradual range of movements (active assisted)
No loading with weights for 6 months following surgery.
In cases of recurrent posterior dislocations, humeral bone loss and reverse Hill-Sachs lesions can result in refractory glenohumeral instability that is difficult to treat [12]. Yamamoto et al. [13] introduced the concept of the glenoid track. Through this concept, engagement is associated with recurrent instability. The surgical treatment goal for Hill-Sachs lesions is to prevent engagement of the lesion [14].
Surgical options to correct an engaging reverse HS lesion can be largely categorized into non-anatomic and anatomic reconstruction. Non-anatomic options include the McLaughlin and modified McLaughlin procedures [15]. Anatomic procedures have been described in the literature for larger lesions, aiming to restore the normal contour of the humeral articular cartilages [16, 17]. There were initially attempts to elevate the areas of anterior impaction in reverse Hill-Sachs lesions. However, due to the loss of integrity in the subchondral bone and persistent damage to the articular cartilage with these techniques, many have begun to favor anatomic reconstruction with osteochondral allograft 12, 13].
In our technique, the use of calcium phosphate cement provides us with a mold, which is exactly the same shape as the prepared defect. When the mold is used as a reference to fashion the allograft, the final graft will have the same three-dimensional measurements as the defect. This anatomical reconstruction restores the congruity and sphericity of the humeral head, at the same time providing viable cartilage. On regular follow-up, our patients had good clinical outcome at 18 months after surgery (Fig. 9a, b, c).
We recommend the use of a calcium phosphate cement mold and fresh frozen osteochondral femoral allograft to fill the humeral head defect accurately (<40%) in young patients with reverse Hill-Sachs lesions. This technique has proven beneficial in providing an anatomical reconstruction and good functional outcome in our patients (Fig. 9a, b, c).
The authors believe that our described technique of using cement mold to fashion the allograft and fill the humeral head is promising. This will help the surgeon obtain a congruent humeral head and hence treat the posterior glenohumeral instability.
References
- 1.1. Martinez AA, Calvo A, Domingo J, Cuenca J, Herrera A, Malillos M. Allograft reconstruction of segmental defects of the humeral head associated with posterior dislocations of the shoulder. Injury 2008;39:319-22. [Google Scholar]
- 2.2. Walch G, Boileau P, Martin B, Dejour H. Unreduced posterior luxations and fractures-luxations of the shoulder. Apropos of 30 cases. Rev Chir Orthop Reparatrice Appar Mot 1990;76:546-58. [Google Scholar]
- 3.3. Khayal T, Wild M, Windolf J. Reconstruction of the articular surface of the humeral head after locked posterior shoulder dislocation: A case report. Arch Orthop Trauma Surg 2009;129:515-9. [Google Scholar]
- 4.4. Diklic ID, Ganic ZD, Blagojevic ZD, Nho SJ, Romeo AA. Treatment of locked chronic posterior dislocation of the shoulder by reconstruction of the defect in the humeral head with an allograft. J Bone Joint Surg Br 2010;92:71-6. [Google Scholar]
- 5.5. Shah N, Tung GA. Imaging signs of posterior gleno-humeral instability. AJR Am J Roentgenol 2009;192:730-5. [Google Scholar]
- 6.6. Patrizio L, Sabetta E. Acute posterior shoulder dislocation with reverse Hill-Sachs lesion of the epiphyseal humeral head. ISRN Surg 2011;2011:851051. [Google Scholar]
- 7.7. McLaughlin HL. Posterior dislocation of the shoulder. J Bone Joint Surg Am 1952;24:584-90. [Google Scholar]
- 8.8. Barlow JD, Abboud J. Surgical options for the young patient with glenohumeral arthritis. Int J Shoulder Surg 2016;10:28-36. [Google Scholar]
- 9.9. Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs “remplissage”: An arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy 2008;24:723-6. [Google Scholar]
- 10.10. Provencher MT, Sanchez G, Schantz K, Ferrari M, Sanchez A, Frangiamore S, et al. Anatomic humeral head reconstruction with fresh osteochondral talus allograft for recurrent glenohumeral instability with reverse Hill-Sachs lesion. Arthrosc Tech 2017;6:e255-61. [Google Scholar]
- 11.11. Scheffer HJ, Quist JJ, van Noort A, van Oostveen DP. Allograft reconstruction for reverse Hill-Sachs lesion in chronic locked posterior shoulder dislocation: A case report. J Med Cases 2012;3:89-93. [Google Scholar]
- 12.12. Cofield RH. Bone grafting for glenoid bone deficiencies in shoulder arthritis: A review. J Shoulder Elbow Surg 2007;16 Suppl 5:S273-81. [Google Scholar]
- 13.13. Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: A new concept of glenoid track. J Shoulder Elbow Surg 2007;16:649-56. [Google Scholar]
- 14.14. Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu JJ, Bernhardson A, et al. The Hill-Sachs lesion: Diagnosis, classification, and management. J Am Acad Orthop Surg 2012;20:242-52. [Google Scholar]
- 15.15. Martetschläger F, Padalecki JR, Millett PJ. Modified arthroscopic McLaughlin procedure for treatment of posterior instability of the shoulder with an associated reverse Hill-Sachs lesion. Knee Surg Sports Traumatol Arthrosc 2013;21:1642-6. [Google Scholar]
- 16.16. Fuchs B, Jost B, Gerber C. Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am 2000;82:16-25. [Google Scholar]
- 17.17. Gerber C, Lambert SM. Allograft reconstruction of segmental defects of the humeral head for the treatment of chronic locked posterior dislocation of the shoulder. J Bone Joint Surg Am 1996;78:376-82. [Google Scholar]