Madura foot, commonly mistaken for the more widespread bacterial osteomyelitis, can be easily diagnosed at an earlier state by MRI to prevent complications due to delay in treatment.
Dr. Binay Kumar Sahu, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi - 110029, India. E-mail: drbinaykumarsahu@gmail.com
Introduction: Madura foot is a rare infective granulomatous foot disease. The burden of this disease has significantly declined in recent years due to better generalized living conditions. Hence, the diagnosis can be quite often missed by the new generation orthopedic surgeon for other more similar conditions. Early diagnosis and prompt treatment is crucial for better outcome and limb survival. We here present the clinical picture of three such Madura foot cases.
Case Series:In this study, three Indian males aged between 40 and 60 years of rural background presented to our department with chronic multiple discharging sinuses of the foot. They were initially treated for several months in their local health centers without any improvement. Finally, they came to our institution where they were thoroughly inspected and underwent various investigations such as magnetic resonance imaging (MRI) and histopathological examination. They were referred across various departments such as dermatology, general surgery and orthopedics, and eventually got correct diagnosis. Treatment was promptly started with oral itraconazole, an antifungal drug, and one patient undergoing additional surgical debulking of the disease which lead to gradual healing of the disease as evident by disappearance of sinuses and return of normal skin in 6-12 months.
Conclusion: Madura foot is very characteristic, although it may mimic more prevalent infectious conditions. The characteristic multiple discharging sinuses with extrusions of sulphur granules and MRI findings of “dot in circle” should clinch the diagnosis quickly. Medical therapy should be continued for at least 12 months even if there is resolution of disease in the early or mid-phase of treatment. Debulking of the disease will aid in early recovery and reduce abnormal swelling or appearance of the foot.
Keywords: Madura foot, eumycetoma, actinomycetoma, multiple discharging sinuses, dot in circle.
Madura foot is a chronic infective lesion of the skin, subcutaneous, and musculoskeletal structure of the foot. Causative organism can be a fungus, in which case it is called eumycetoma, or bacteria, where it is called actinomycetoma. The main burden of this disease is among equatorial and tropical regions. In India, this is more prevalent in the southern states. However, a few cases are reported from northern region also.
The condition has a slow and progressive course where it usually develops from a small firm painless nodule to multiple black discharging sinuses with grossly disfigured foot. It is more common in men and agricultural persons who walk bare footed leading to traumatic inoculation of contaminated soil. The classical triad is of painless swelling, draining sinuses and extrusion of grains. Discharge of sulphur granules is pathognomonic of mycetoma foot.
As in recent years, the cases of Madura Foot have significantly declined; these cases can be mistaken for the more common bacterial osteomyelitis which leads to tiring months of unyielding treatment. This is frustrating for both the clinician and the patient. This leads to many months lost to disability with major financial loss for the patient. In general, X-rays show nonspecific osteomyelitic changes of foot. Proper clinical knowledge and detailed examination is often sufficient to rule out the differentials. Diagnosis is generally made clinically featuring the triad, supported by histopathology and magnetic resonance imaging (MRI). This study will help the young orthopedic surgeon or clinician to quickly diagnose and start treatment so as to relieve the patient of disability and economic burden as early as possible.
Case 1
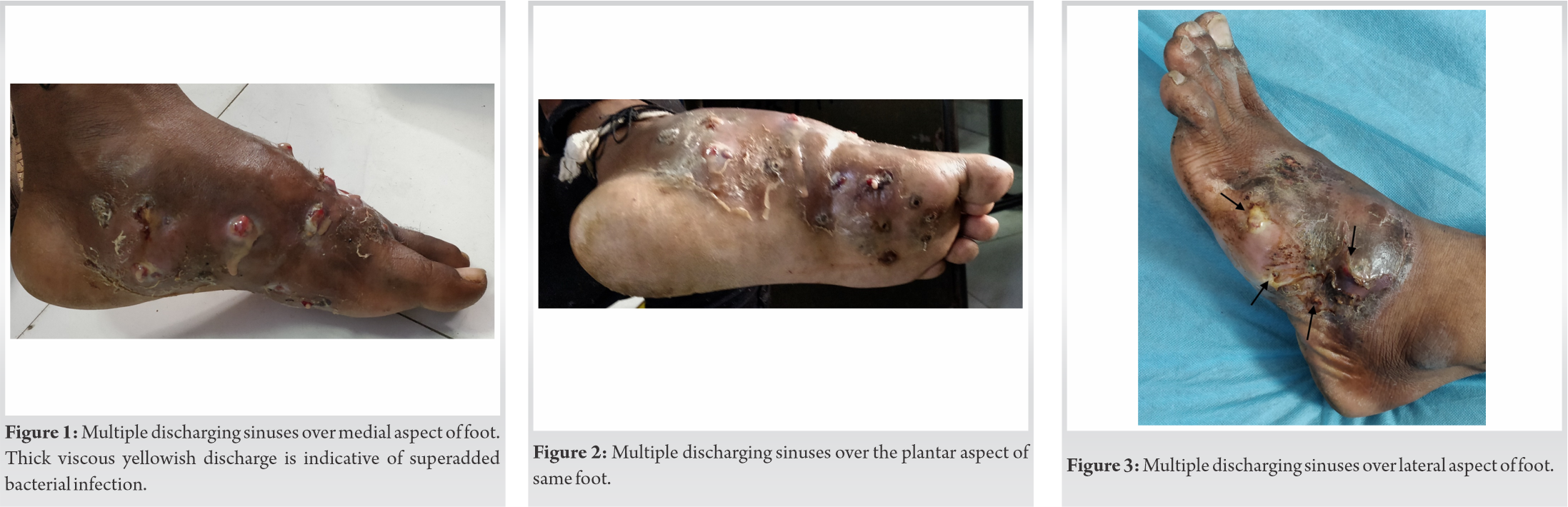
A 54 years old north Indian man presented to us with painless swelling of right foot that started 8 years back. The gradually progressive swelling was associated with multiple discharging sinuses over dorsum (Fig. 1) and sole (Fig. 2) of the foot. Patient is a farmer by profession and works in paddy fields and does not give clear history of foot trauma. Patient had previously taken several antibiotic courses irregularly for the past 3 year but no major improvement was noticed. This patient was referred to our department by dermatology department of our institution. On histopathology, it was found to be eumycetoma. Patient was then started on itraconazole 400 mg daily in two divided doses to continue for at least 12 months. Within the initial few months there was subjective improvement. There was gradual reduction of discharging sinuses evident from 3 months onwards, but the swelling was taking longer to subside. Hence, we have advised him regarding debulking of the diseased foot which he refused. Nonetheless, the skin of the foot had started looking normal at 8 months while the gross swelling and deformity had minimal improvement. Patient has been asked to continue the antifungal for another 4 months.
Case 2
A 60 years old man from northern India presented to us with painless woody swelling of right foot for the last 12 years. He is farmer by occupation. The swelling was associated with multiple draining sinuses with discharge of viscous fluid with yellow granules from the lateral aspect of foot (Fig. 3, 4). X-ray revealed major soft tissue swelling with early bony changes (Fig. 5). The patient gives a past history of traumatic loss of the 5th ray of right foot in his childhood. For the current scenario, patient was earlier treated in a local hospital for several months with different antibiotics but with no improvement happened. This patient was referred to us from the General Surgery department of our institution. Histopathological reports suggested eumycetoma. Patient also gave recent history of fever for the past few days with rapid increase in further swelling of foot. These features were suggestive of secondary acute bacterial infection. Patient has been started on itraconazole 400 mg daily in two divided doses for 8 months along with short course (10 days) of oral amoxycillin 500 mg + clavulanic acid 125 mg three daily. Fever and acute swelling subsided in 10 days. Patient underwent surgical debulking at 2 months. Sinuses disappeared and skin returned to normal at 6 months of treatment but some residual swelling of the foot persisted. More 6 months of medical therapy is advised to complete.
Case 3
A 40 years old man from north India, working as a farmer in sugarcane fields, presented to our department with insidious onset, gradually progressive painless firm swelling of right foot of 5 years duration. It was associated with multiple sinuses with scanty discharge and extrusion of black grains (Fig. 6, 7). No associated systemic features were present. The patient was initially treated in his local town by different physicians for the past 3 years. However, the disease persisted. Patient was diagnosed here based on clinical features as Madura foot. X-ray showed nonspecific osteomyelitic changes of tarsal bones (Fig. 8). MRI picture showed the characteristic multiple sinuses with ‘dot in circle’ picture (Fig. 9). Further histopathological confirmed fungal mycetoma. The patient was then started on itraconazole 400 mg in two divided doses for 12 months. At 3 months, patient became symptomatically better with marked decreased in discharge. At 6 months, he had complete resolution of discharging sinuses and the skin returned to normal. He completed his medical therapy at 12 months.
Madura foot has been known to mankind since long time. The name Madura foot is derived from the south Indian city of Madura where it was said to be first reported in early nineteenth century [1]. The picture of this chronic infection has been described by many early writers of the twentieth century as done by Tribedi and Mukherjee in 1939 [2]. They described the condition as that of an emaciated patient with a foot disfigured and pitted by numerous discharging sinuses. At that time, the feasible treatment was amputation of the part. Later on, in around early 1960s, various case series were published on Madura foot as done by Oyston where he discussed the clinico-radiological as well as pharmacological aspect of the condition. Nevertheless, surgery, mainly amputation, was the most preferred choice of treatment at that time period. The study discussed the limited role of drugs such as dapsone and tetracycline [3].
Nowadays, Madura foot is mainly encountered in the poor countries of the tropics or equatorial region. Few cases in the western world are also reported mainly in the migrant population [4]. The patients are generally out of work for a prolonged time period due the disease which bears a heavy economic cost to the family especially in countries such as India and other developing nations.
Madura foot develops as a chronic infective lesion of the foot mainly after traumatic inoculation with contaminated soil, seen mostly in agricultural workers who walk bare footed [5]. Madura foot can be classified grossly into two subgroups – Actinomycetoma and Eumycetoma. The former is a gram positive filamentous bacterial infection while the latter is caused by true fungi. Most common location of infection is foot, accounting for about 70% [6]. Other sites of infection such as back, arm, leg and hand are also reported. Immunocompromised persons are more prone to suffer this condition. In general, there is no major systemic involvement like fever, constitutional symptoms expect in cases with secondary bacterial infection. No direct reports of death have been attributed to this condition.
The incubation period is a prolonged one, sometimes up to 5 years [7]. Early in the disease, patient usually present with a painless firm swelling of the foot. Following this, the classical triad is visible consisting of chronic induration, draining sinuses and discharging granules. Blackish granules are characteristic of fungal etiology, whereas white/yellow granules may suggest either bacterial or fungal [8]. In early stages, the disease is confined to subcutaneous tissues but gradually it spreads to the skeletal structures. Histopathologically, features of non-specific chronic granulomatous inflammation are seen. Centrally, the granulomata contain small microabscesses which are characterized by numerous neutrophils and the causative agents, which in turn are surrounded by granulation tissue containing acute and chronic inflammatory cells. Extruded granules on microscopy reveal the organism which can be differentiated by lactophenol. Thin filaments represent actinomycetes and thicker hyphae represent fungal infection.
X-ray features are typical of soft tissue swelling, cortical erosions and thickening, periosteal reaction, bony lucencies, joint destruction, osteopenia, and sometimes “moth eaten appearance” with bone lysis are seen. MRI can clinch early diagnosis of the condition. The highly specific “dot in circle” sign is characteristic of early soft tissue infection [9]. Newer techniques of diagnosis like DNA sequencing guide in identifying the causative organism. A case report was published where Madura foot negative on culture was finally diagnosed with amplification and sequence analysis of fungal ribosomal DNA segments [10].
Clinical diagnosis of Madura foot should not be very difficult when classical multiple discharging sinuses with extrusion of grains in a moderate to grossly swollen foot are present. Such striking are these features that the young orthopedic surgeon once having seen it shall be able to diagnose clinically other cases of Madura foot quite easily. Diagnosis should be confirmed further by histopathological analysis. Superadded acute bacterial infection can intensify the sign and symptoms. Such a patient presents with a painful discharging foot with or without associated fever.
Treatment of Madura foot is quite cumbersome and takes a prolonged time. It usually consists of medical and surgical therapy. Initially, treatment consists of a lengthy course of antifungal/antibacterial depending on whether its eumycetoma/actinomycetoma. Fungal mycetoma is reported to be more resistant to medical therapy with higher recurrence rate, sometimes more than 50% [8]. On the other hand, actinomycetoma has a good prognosis with cure rates of more than 50% with medical therapy [11]. Early diagnosis and start of medical therapy limits extensive bony involvement and subsequent deformity. Commonly used drugs for actinomycetoma are combination of cotrimoxazole plus amikacin (Welsh regimen), which is successful in about 90% cases [12]. Other drugs such as dapsone, rifampicin, and tetracycline are also effective [13]. For eumycetoma, azole derivatives are effective. Fungal mycetoma is more resistant to medical therapy requiring prolonged course and combination with surgical debulking for residual disease. Resistant cases of both types, ones with secondary bacterial infection and grossly disfigured foot generally require radical procedures like amputation. There is no standard timeline duration for medical treatment. Response is checked clinically as well as radiologically. Decrease in swelling of foot with gradual disappearance of sinuses and nodules, return of normal skin, and X-ray features of absorption of sclerosed bones, reappearance of normal bony trabeculae with improving bone density are suggestive of successful treatment.
Diagnosis of Madura foot should be easy when clinical triad of subcutaneous nodules, discharging sinuses and grains are present. However, if the classical multiple discharging sinuses with granules are missing then the diagnosis of Madura foot can be mistaken for other more common chronic conditions such as neoplasms, neuropathic foot, implant related osteomyelitis, chronic bacterial infection, or tuberculosis [14]. MRI finding of “dot in circle” is characteristic and should differentiate Madura foot from above mentioned conditions with further confirmation on biopsy.
Madura foot although being a rare disease can be easily diagnosed by gross clinical features with further confirmation by histopathology. The patient is generally of rural background, especially farmer with long standing history. These patients require special attention as the disease is associated with heavy economic cost. The clinical features are so striking that the young orthopedic surgeon once having seen it shall be able to recognize further cases in his/her career quite easily. Early diagnosis and treatment is of utmost importance for quick recovery and preventing further deformity as well as need for radical procedures like amputation. Medical therapy should be continued for at least 12 months even if there is resolution of disease in the early or mid-phase of treatment. Debulking of the disease will aid in early recovery and reduce abnormal swelling or appearance of the foot. A multidisciplinary approach with team consisting of orthopedic surgeons, general surgeons, dermatologists, pathologists, and sometimes plastic surgeons are required for proper management of this tiring condition. For the new orthopedic surgeon or clinician who has not seen madura foot cases will confuse the condition to more common conditions such as tuberculosis, neoplasms, neuropathic foot, and chronic implant related infections; this study sought to guide them in making quick diagnosis and starting effective treatment.
Madura foot is a chronic debilitating disease which can be readily diagnosed based on the striking clinical triad of painless swelling, draining sinuses and extrusion of grains, and MRI finding of “dot in circle.” Treatment with antifungals should be continued for at least 12 months even if the disease has resolved earlier.
References
- 1.Magana M. Mycetoma. Int J Dermatol 1984;23:221-36. [Google Scholar]
- 2.Tribedi BP, Mukherjee BN. Actinomycotic and mycotic lesions, with special reference to madura foot. Br J Surg 1939;27:256-65. [Google Scholar]
- 3.Oyston JK. Madura foot: A study of twenty cases. Bone Joint J 1961;43-B:259-67. [Google Scholar]
- 4.El Muttardi N, Kulendren D, Jemec B. Madura foot-mind the soil. J Plast Reconstr Aesthet Surg 2010;63:e576-8. [Google Scholar]
- 5.Relhan V, Mahajan K, Agarwal P, Garg VK. Mycetoma: An update. Indian J Dermatol 2017;62:332. [Google Scholar]
- 6.Foltz KD, Fallat LM. Madura foot: Atypical finding and case presentation. J Foot Ankle Surg 2004;43:327-31. [Google Scholar]
- 7.El Muttardi N, Kulendren D, Jemec B.Madura foot-mind the soil. J Plast Reconstr Aesthet Surg 2010;63:e576-8. [Google Scholar]
- 8.Ching BY, Maraczi G, Urbina D. Madura foot. A case presentation. J Am Podiatr Med Assoc 1991;81:443-7. [Google Scholar]
- 9.Sarris I, Berendt AR, Athanasous N, Ostlere SJ, OSIRIS Collaborative Study Group. MRI of mycetoma of the foot: Two cases demonstrating the dot-in-circle sign. Skelet Radiol 2003;32:179-83. [Google Scholar]
- 10.Yera H, Bougnoux ME, Jeanrot C, Baixench MT, De Pinieux G, Dupouy-Camet J. Mycetoma of the foot caused by Fusarium solani: Identification of the etiologic agent by DNA sequencing. J Clin Microbiol 2003;41:1805-8. [Google Scholar]
- 11.Lupi O, Tyring SK, McGinnis MR. Tropical dermatology: Fungal tropical diseases. J Am Acad Dermatol 2005;53:931-51. [Google Scholar]
- 12.Welsh O, Al-Abdely HM, Salinas-Carmona MC, Fahal AH. Mycetoma medical therapy. PLoS Neglected Trop Dis 2014;8:e3218. [Google Scholar]
- 13.Salim AO, Mwita CC, Gwer S. Treatment of Madura foot: A systematic review. JBI Database System Rev Implement Rep 2018;16:1519-36. [Google Scholar]
- 14.NGoldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K. Fitzpatrick’s Dermatology in General Medicine. 8th ed. New York: McGraw & Hill; 1999. [Google Scholar]