Low force mechanisms can lead to hip dislocations in young children and every child complaining knee pain must be correctly investigated!
Dr. Andrea Cosentino, Department of Orthopaedic, Franz Tappeiner Hospital, Via Rossini, Meran, Italy. E-mail: andrea.cosentino@sabes.it
Introduction:Evaluation of pain in children after trauma can sometimes be difficult; in particular, a knee pain in a child could originate from the hip, until evidence of the contrary. Often is the low-energy trauma that leads to a joint dislocation in children. Furthermore, the present guidelines state that a hip dislocation in a child should be replaced within 6 (maximum 12) hours, to reduce the risk of avascular necrosis (AVN) of the femoral head.
Case Presentation:After falling during sports activity at the kindergarten, a 5-years-old boy was taken to the emergency room of a small hospital with severe pain in his right knee. After the visit and the instrumental diagnosis, he was afterward discharged with the diagnosis of contusion of the thigh. After a week of pain and inability to load despite the analgesic therapy, he was accompanied to our hospital, from which the diagnosis of hip dislocation emerged and then reduced in short sedation. The next day he underwent to a magnetic resonance imaging (MRI) examination and pelvic-podalic cast immobilization. At the following check-ups, he had no more pain and the active ROM was complete. A long-term control after 5 years showed a complete and painless active ROM and the MRI showed a normal growth of the bone, without any sign of AVN of the femoral head.
Conclusion: Despite the long waiting period and going against the guidelines, the child recovered his full daily and physical activity, without necrosis of the femoral head, growth disorder, or dysmetria in the lower limbs.
Keywords: Avascular necrosis, hip dislocation, pediatric orthopedic.
A hip dislocation in a child can also occur as a result of a minor trauma. However, it is always essential to examine the hips in a child complaining of knee pain after low-energy trauma, to rule out any pathology of the hip like for example SCFE or hip dislocation.
According to the present guidelines, traumatic hip dislocations should be reduced within 6 h (maximum 12 h), always under sedation to achieve maximum muscle relaxation. We present the case of a 5-year-old boy who complained right knee pain after a low-energy trauma during kindergarten activities, which came to our attention a week after the trauma.
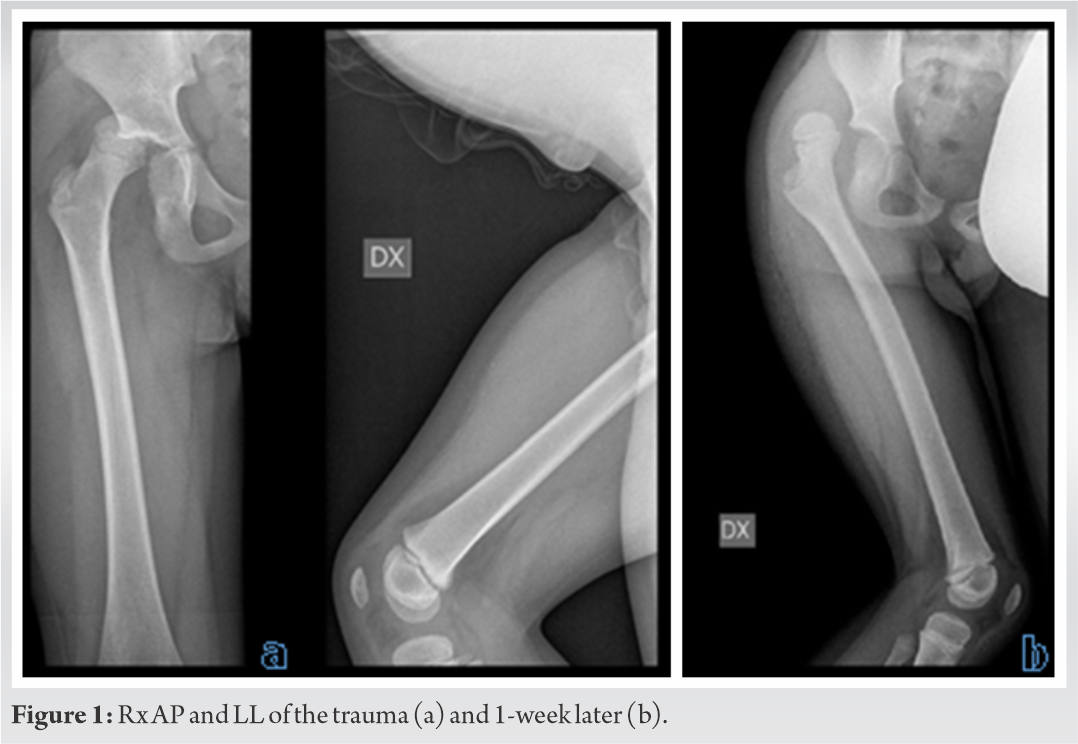
A 5-year-old boy comes to the emergency room of our hospital a week after trauma to his right leg during kindergarten activities, falling with his leg turned backward. Immediately after the trauma, he was taken to the hospital closest to his home, where an X-ray of the entire femur was performed. Despite the clear X-ray findings (Fig. 1a), the patient was discharged with the diagnosis of contusion of the thigh and with the therapy of functional rest and analgesics, when needed.
Due to the persistence of the symptoms, the patient after a week was taken to the emergency room of our hospital, where he presented the right lower limb internally rotated and shortened. An X-ray was then repeated confirming the diagnosis of hip dislocation (Fig. 1b).
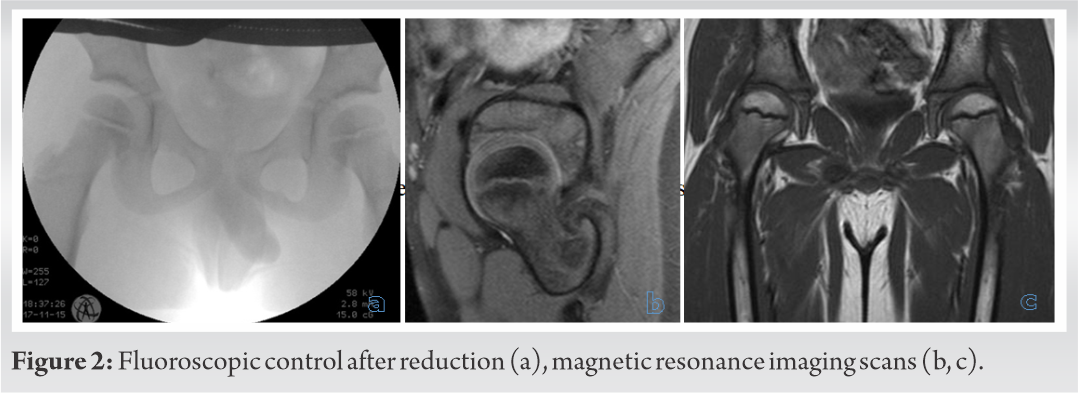
The child was immediately taken to the operating room where sedation and reduction were planned. Once the maximum sedation was reached, we proceeded to the closed reduction of the dislocation with the leg in cautious flexion, light and continuous traction for about 5 min and external rotation, confirmed by the fluoroscopic image obtained in the operating room.
The child remained under observation for 3 days in the pediatric department, the time necessary to perform a magnetic resonance imaging (MRI) to evaluate the state of the femoral head and to immobilize the hip joint with a pelvic-podalic cast (Fig. 2).
1 month after the reduction, a follow-up visit with X-ray was performed. The cast was removed and the child clinically moved the hip well, slightly painful at the highest degrees of motion and a slight limp remained.
A new clinical check-up was performed after 3 months, where this time the child presents full load and complete ROM, he has also resumed his sporting activity without limitations.
Six months after the reduction, a new visit was made, this time with MRI of the hip. Clinically, the child still had no pain; the right hip was perfectly comparable to the left hip. In the MRI, the femoral head appeared normal, with no signs of avascular necrosis (AVN).
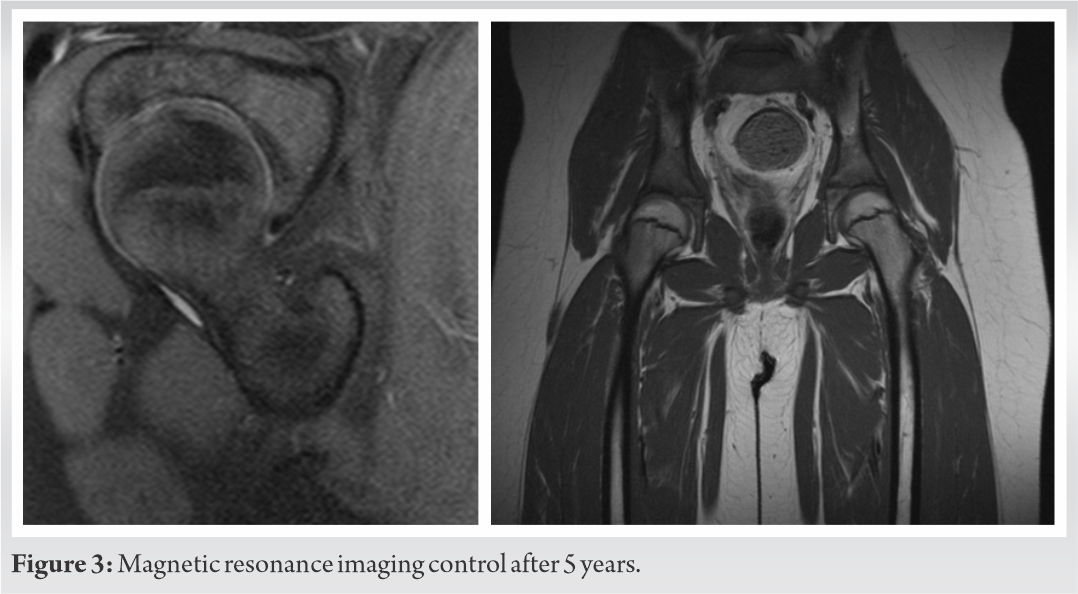
We decided to perform furthers checkup 1 year and 5 years after the trauma, again with additional MRIs, to exclude definitively a long-term necrosis and to control the clinical function of the involved hip. Also at those check-ups, the child presented no symptoms, the legs hadn’t no discrepancy in terms of length, active and passive ROM and weight bearing, as well as the MRIs were similar to the previous (Fig. 3).
Traumatic hip dislocation is a rare condition with a bad prognosis due to potential complications in children. THD usually occurs as a result of low energy traumas such as simple falls and sport injuries in children under the age of ten [1].
As described by Yuksel and Albay [2] and Hung [3], the most frequent complications are a sciatic nerve injury, followed by the AVN of the femoral head, because the vascular supply to the proximal epiphyseal plate of the femur can be disrupted.
Greater risk of AVN is seen with older aged children (>10 years), high-energy trauma and prolonged dislocation time (>6 h).
The right management of those dislocations foresees a timely and correct reduction as one of the best means to reduce complications; in detail, the reduction should occur within 4–6 h from the trauma. A reduction after 6 h is associated with increased risk of AVN, despite in literature there are some meta-analyses that demonstrate that there are no differences between early (<6 h from the time of injury) over late (>6 h from the time of injury) reduction in traumatic hip dislocation and preventing osteonecrosis of the femoral head [2, 3, 4, 8, 10].
A closed reduction should be performed as soon as possible: For children, many advocate the reduction in the Operating Room under general anesthesia and optimal muscle relaxation, because of the high risk of injuring the proximal femur growth plate during the reduction. Fluoroscopy should be performed to ensure proper reduction [2]. Various reduction techniques have been successfully used for children; often just a gentle longitudinal traction is successful. Reduction in the Emergency Department in sedation may be considered if the Operating Room isn’t immediately available thus prolonging dislocation time is prospected, or an adequate muscle relaxation can be achieved with safe and deep sedation [2, 5]. An open reduction should be considered in fracture-dislocation or after unsuccessful closed reduction attempts (max. 2 attempts) [5, 9].
After an open or closed reduction is always mandatory a post-reduction imaging [5]. The standard AP pelvis and frog leg lateral view of hip are often done. Plain films and CTs can be inadequate to evaluate the pediatric acetabulum and its associated structures, so MRI is advocated for [6, 7].
Post-reduction immobilization is also mandatory but, at the moment, the duration of immobilization, a non-weight bearing status and partial weight being status is debated [2, 3]. The immobilization immediately following reduction is required to allow the surrounding soft tissues to heal adequately.
Despite the delayed diagnosis and against the timing suggested by the guidelines, our presented child with a traumatic hip dislocation has no growth-related problem.
It´s always to remember that not only high-energy traumas produce a hip dislocation but often also low force mechanisms can lead to hip dislocations in young children. At the same time, do not forget to look for other associated injuries!
The growth plates are fragile! If the Operation room is available, that may be the best place for the child! If it is not available, make sure you can safely relax the muscles and then you should be super gentle!
References
- 1.Başaran SH, Bilgili MG, Erçin E, Bayrak A, Öneş HN, Avkan MC. Treatment and results in pediatric traumatic hip dislocation: Case series and review of the literature. Ulus Travma Acil Cerrahi Derg 2014;20:437-42. [Google Scholar]
- 2.Yuksel S, Albay C. Early reduction of pediatric traumatic posterior hip dislocation is much more important than the treatment procedure. Pediatr Emerg Care 2019;35:e206-8. [Google Scholar]
- 3.Hung NN. Traumatic hip dislocation in children. J Pediatr Orthop B 2012;21:542-51. [Google Scholar]
- 4.Morris AC, Yu JC, Gilbert SR. Arthroscopic treatment of traumatic hip dislocations in children and adolescents: A preliminary study. J Pediatr Orthop 2017;37:435-9. [Google Scholar]
- 5.Baker JF, Leonard M, Devitt BM, Queally JM, Noel J. Traumatic hip dislocation in a 3-year-old girl. Pediatr Emerg Care 2011;27:1178-9. [Google Scholar]
- 6.Thanacharoenpanich S, Bixby S, Breen MA, Kim YJ. MRI is better than CT scan for detection of structural pathologies after traumatic posterior hip dislocations in children and adolescents. J Pediatr Orthop 2020;40:86-92. [Google Scholar]
- 7.Hearty T, Swaroop VT, Gourineni P, Robinson L. Standard radiographs and computed tomographic scan underestimating pediatric acetabular fracture after traumatic hip dislocation: Report of 2 cases. J Orthop Trauma 2011;25:e68-73. [Google Scholar]
- 8.Mortimer JA, Dzus A. Delayed diagnosis of hip dislocation in a young child. Can Fam Physician 2016;62:815-7. [Google Scholar]
- 9.Mehlman CT, Hubbard GW, Crawford AH, Roy DR, Wall EJ. Traumatic hip dislocation in children. Long-term followup of 42 patients. Clin Orthop Relat Res 2000;376:68-79. [Google Scholar]
- 10.Ahmed G, Shiraz S, Riaz M, Ibrahim T. Late versus early reduction in traumatic hip dislocations: A meta-analysis. Eur J Orthop Surg Traumatol 2017;27:1109-16. [Google Scholar]