It's important to identify bicondylar conjoint Hoffa fracture (BCHF) as its surgical approach differs from the bicondylar Hoffa non-conjoint variant, so we highly recommend getting an non- contrast computed tomography NCCT scan with three-dimensional reconstruction in all such cases to not miss any other associated injuries.
Dr. Avinash Kumar, Department of Orthopaedics, All India Institute of Medical Sciences, Patna, Bihar, India. E-mail: dravinashk@aiimspatna.org
Introduction: Bicondylar Conjoint Hoffa fractures, where both the fractured femoral condyles joined by the bony bridge at intercondylar notch, are extremely rare with only 7 cases reported so far in the literature. We present a first case of such fracture along with patellar fracture dislocation where a fractured fragment was incarcerated between the femoral condyles.
Case Presentation:18 years old boy after road side accident presented with knee swelling and pain. Computed tomography revealed this rare combination of the fractures and was appropriately managed.
Conclusion:High index of suspicion in trauma victims with described mechanism of injury like in this report is needed to not miss the Hoffa fracture and to differentiate conjoint variety from bicondylar unconjoint and deciding appropriate surgical. Non- contrast computed tomography NCCT is a must to look for fracture geometry and associated fractures.
Keywords:Hoffa fracture, adolescent bicondylar, patellar fracture dislocation.
Hoffa’s fracture is the coronal plane fracture of the distal femur first described by Albert Hoffa in 1904 [1]. Mostly it is unicondylar involving lateral condyle because of physiological genu valgum but can be bicondylar or conjoint too depending on the mechanism of injury. Conjoint variety, where both the condylar fractures are connected by a bridge of intact bone adjacent to the intercondylar notch, is the rarest among three. Bicondylar Conjoint Hoffa fracture (BCHF), besides being a rare one, associated with other fractures makes it one of the rarest injury patterns.
We hereby report a case of BCHF with associated patellar fracture dislocation with an incarcerated patellar fragment in Hoffa fracture. To the best of our knowledge, no report of such associations has been reported in literature so far. In this report, we will emphasize the mechanism of injury, astute clinical examination and its management. We will also review the literature on BCHF till date.
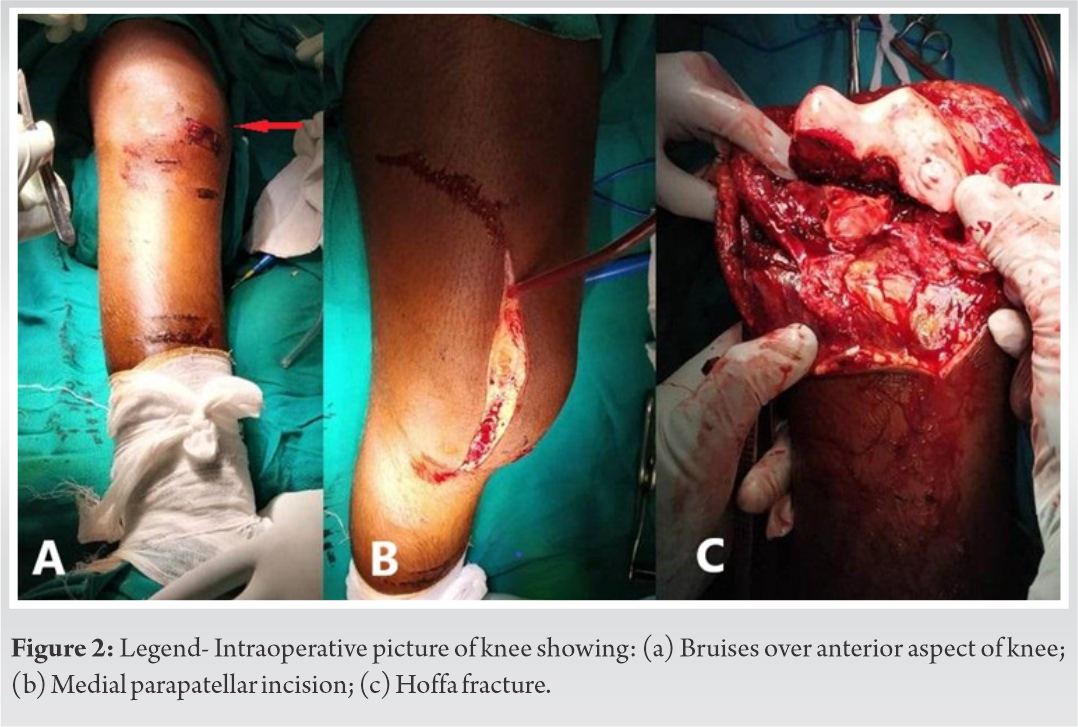
A 18 years old male sustained a direct trauma to his right knee when a car hit his bicycle; following which he developed acute pain and swelling in his right knee and was unable to bear weight on the affected limb. He was referred to our center for further management after getting his limb splinted at a primary clinic. Patient was managed following proper Advanced Trauma Life Support protocol. On examination, abrasion and gross swelling was seen over his right knee. Distal neurovascular status was normal and no signs of compartment syndrome were present. Proper radiographs and non-contrast computed tomography (NCCT) of the affected limb were obtained. Radiographs showed coronal plane fracture of distal femur. NCCT further revealed patellar dislocation with vertical fracture of patella with BCHF of distal femur with patellar fracture fragment incarcerated into it (Fig. 1) Legend- NCCT of right knee with red arrows showing: (a) Incarcerated patellar fragment into the femoral condyles, (b) Bony continuity between two fractured femoral condyles (conjoint), (c) Patellar dislocation, (d) Patellar fracture.
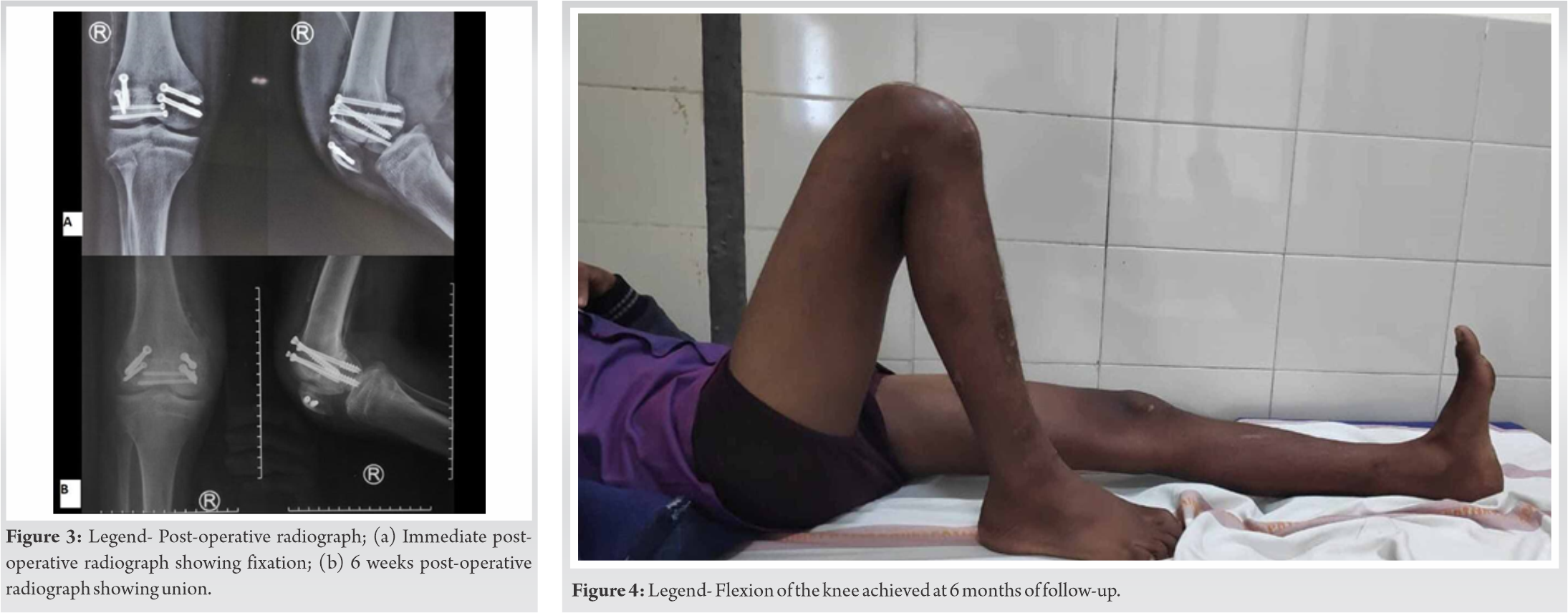
After routine evaluation and resuscitation of the patient, he was taken up for surgery. Under epidural anesthesia with the patient in supine position, upper thigh pneumatic tourniquet was applied. After part preparation, painting and draping, knee joint was approached using medial parapatellar approach (Fig. 2) Legend- Intraoperative picture of knee showing: (a) Bruises over anterior aspect of knee, (b) Medial parapatellar incision, (c) Hoffa fracture. Medial patello-femoral ligament (MPFL) was found to be torn along with a rent in the medial retinaculum. After incising the deep fascia, part of the quadriceps tendon was also found to be torn from the upper pole of patella. As the knee was flexed, Hoffa fracture was identified and the patellar fragment was incarcerated between it. The Patellar fragment was dis-impacted from the fracture ends. BCHF was reduced and held with reduction clamps and provisionally secured with K-wires and fixed with three 6.5 mm and a 4 mm partially threaded cannulated cancellous screws (PTCS) from anterior to posterior. Then, patella fracture was reduced and fixed with two 4 mm PTCS (Fig. 3) Legend- 3: Post-operative radiograph; (a) Immediate post-operative radiograph showing fixation; (b) 6weeks post-operative radiograph showing union.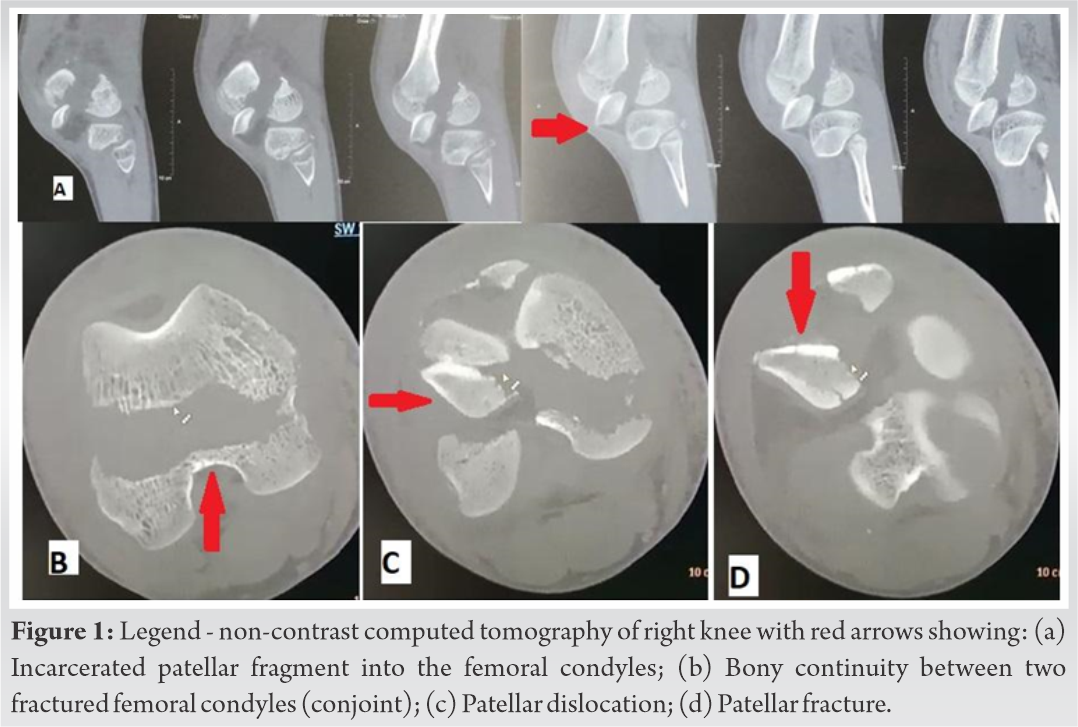
Quadriceps strengthening exercise and active range of motion exercise was started from postoperative day 1 (POD1). Patient was discharged on POD 5 with advice of protected non weight bearing mobilization. The patient was followed at 2 weeks, 4 weeks and 6 weeks intervals. He was advised full weight bearing after radiological union. Patient attained 130° of flexion with no extension lag at 6 months, and there was complete union of all the fractures. (Fig. 4) Legend- Flexion of the knee achieved at 6 months of follow-up.
Hoffa fractures, according to Orthopedic Trauma Association classification, are classified into B3 coronal fractures with B3.2 as unicondylar Hoffa fractures and B3.3 as bicondylar Hoffa fractures [2]. BCHFs are not explicitly classified in the system though they are generally placed under B3.3. Hoffa fractures are classified into Unicondylar, bicondylar and conjoint variants. Since the mechanism of fracture is different, we also back the proposed subclassifications by Ul Haq et al. where B3.3 was subclassified into Bicondylar Unconjoint Hoffa Fractures and BCHFs.
The mechanism of injury is not known clearly yet. Although shearing forces to the posterior femoral condyles have been postulated, it’s also proposed that both direct impact and indirect shear with twisting mechanisms may be the mechanisms [3]. Axial loading on a flexed/hyperflexed knee produces required posterior shearing force to cause Hoffa fracture [3]. In our case, we presumed that the impact was direct as ascertained by the presence of abrasions and bruises over the anterior aspect of the knee. Lesser the flexion increases the probability of fracture line to be close to posterior femoral cortex and hence the possibility of conjoint variety while hyperflexion will produce Bicondylar Unconjoint fracture [4]. This can explain the conjoint variety in our patient whose knee would be semi-flexed while riding the bicycle. This reported case presents an unusual unique fracture pattern, as in addition to BCHF there is a vertical split fracture of patella along with its dislocation due to incomplete quadriceps rupture and MPFL tear. Therefore, this fracture pattern cannot be only due to posterior directed force or an axial force; hence, we propose that there must be rotational component to place the patella eccentrically in front of lateral femoral condyle to cause vertical split fracture which would have further caused rupture of MPFL, medial retinaculum along with partial avulsion of quadriceps tendon.
This is the first reported case after thorough search and review of literature where BCHF was associated with patella dislocation along with vertical fracture of the patella, and hence, this proposed mechanism explains all the injuries associated with our case. The BCHF reported till date have been reviewed in Table 1, which accounts for a total 8 reported cases including our case [4, 5, 6, 7, 8, 9, 10]. Out of these, 3 are pediatric BCHFs.
Being a high velocity injury, it is usually associated in 37.5% of the patients with multiple other fractures in the ipsilateral limb or other parts of body that makes them prone to be misdiagnosed [11]. Undiagnosed Hoffa fractures may lead to long term disability [12]. Hence, we recommend to have a high index of suspicion for these fractures while attending any trauma patients with swelling around the knee. Identifying Hoffa fractures on plain radiographs remains a challenge due to overlap of the anterior part of the femoral condyles on the anteroposterior (AP) view radiograph [13] and difficulty in getting true lateral views of traumatized knee. Even on true lateral views, minimally displaced fractures are missed [14]. Therefore, NCCT of the knee is of paramount importance not only in fracture identification but also in outlining the fracture pattern, in planning the surgical approach and also in keeping the armamentarium ready before proceeding for the fixation. Many authors have suggested NCCT scan with 3D reconstruction to be the investigation of choice for Hoffa fractures which we also propagate [15].
Different extensile approaches and dual approach have been described in literature for bicondylar hoffa fractures like Gerdy tubercle osteotomy combined with anterior lateral parapatellar approach by Lee et al. [16], Swashbuckler approach by Dua et al. [14]. We decided to approach the fracture using the medial parapatellar approach as the medial retinaculum was already torn and patella was laterally dislocated obscuring the correct site of lateral arthrotomy.
Fixation of Hoffa fractures are usually done by either PTCS depending on the fracture comminution [3, 11] and rarely plate fixation is required. In a biomechanical study by Jarit et al., it was shown that postero anterior (PA) screw configurations make biomechanically stronger constructs than AP screws [17]. However, the placement of screws in the PA plane is risky as damage to neurovascular structures can happen. In our case, since the distance of the fracture line from the posterior femoral cortex was less, we were able to achieve proper lag effect from AP direction without any risk of damaging neurovascular structure. We recommend that if the stock of bone is enough posteriorly to accommodate either 16 mm or 32 mm thread of cannulated cancellous screw it is safer to go from AP direction instead of PA direction. Ul Haq et al. demonstrated that fixation with two screws is better than one screw and using two 6.5 mm partially threaded cancellous screws provided better mechanical advantage than two 3.5 mm fully threaded screws [4]. Excess number of screws will decrease the area of bone to bone healing and can also have deleterious effects on the articular cartilage. Plate fixation is not commonly used with Hoffa fractures, it is mainly done to produce a buttress or anti-glide function when placed posteriorly and neutralizing deforming forces when placed laterally or medially. Plate fixation can be useful in fractures having extension into metaphysis proximally with a beak. Combination of plate fixation with screw fixation has better mechanical stability compared to only screw fixation in conditions such as comminuted Hoffa fracture and osteoporosis [18, 19].
Rehabilitation postoperatively is as important as the quality of fixation. There is no clear consensus in literature regarding rehabilitation and mobilization of bicondylar Hoffa fracture patients. Calmet et al. advised immobilization for 6 weeks followed by range of motion exercises and weight bearing at 6 weeks [20]. There are many others reports recommending initial period of immobilization for 2 weeks followed by gradual range of motion exercises and full weight bearing to be achieved by 2–3 months [4, 5, 13, 14]. Early knee mobilization is essential to prevent knee stiffness. Initial period of immobilization and physiotherapy should be balanced to protect the soft tissue repair and prevent knee stiffness at the same time.
In conclusion, we want to emphasize on having high index of suspicion in trauma victims with above described mechanism of injury to not miss the Hoffa fracture and to differentiate conjoint variety from bicondylar unconjoint as former can be treated by single approach owing to presence of a bony bridge between two condylar fragments while the later may require dual approach. NCCT is a must to look for fracture geometry and associated fractures to avoid surprise in the operating room. Soft tissues around the patella and femoral condyles should be inspected before starting the definitive fixation of the obvious fractures.
It’s important to identify BCHF as its surgical approach differs from the bicondylar Hoffa non conjoint variant. We highly recommend getting a NCCT scan with three dimensional reconstructions in all such cases to not miss any other associated injuries.
References
- 1.Hoffa A. Lehrbuch der Frakturen und Luxationen. 4th ed. Stuttgart: Ferdinan Enke Verlag; 1904. p. 453. [Google Scholar]
- 2.Müller ME, Nazarian S. Classification of fractures of the femur and its use in the A.O. index (author’s transl). Rev Chir Orthop Reparatrice Appar Mot 1981; 67:297-309. [Google Scholar]
- 3.Lewis SL, Pozo JL, Muirhead-Allwood WF. Coronal fractures of the lateral femoral condyle. J Bone Joint Surg Br 1989;71:118-20. [Google Scholar]
- 4.Ul Haq R, Modi P, Dhammi I, Jain AK, Mishra P. Conjoint bicondylar Hoffa fracture in an adult. Indian J Orthop 2013;47:302-6. [Google Scholar]
- 5.Lal H, Bansal P, Khare R, Mittal D. Conjoint bicondylar Hoffa fracture in a child: A rare variant treated by minimally invasive approach. J Orthop Traumatol 2011;12:111-4. [Google Scholar]
- 6.Kishan R, Saibaba B, Kumar V, Aggarwal S. Conjoined bicondylar coronal plane fracture of the distal femur associated with incarcerated patella. BMJ Case Rep 2016;2016:2015213579. [Google Scholar]
- 7.Harna B, Goel A, Singh P, Sabat D. Pediatric conjoint Hoffa’s fracture: An uncommon injury and review of literature. J Clin Orthop Trauma 2017;8:353-4. [Google Scholar]
- 8.Harna B, Dutt Dwivedi D, Pippal HK, Sabat D. Bicondylar conjoint Hoffa’s fracture with patella entrapped in the fracture: A rare case report. J Clin Orthop Trauma 2018;9:S35-8. [Google Scholar]
- 9.Julfiqar, Huda N, Pant A. Paediatric conjoint bicondylar Hoffa fracture with patellar tendon injury: An unusual pattern of injury. Chin J Traumatol 2019;22:246-8. [Google Scholar]
- 10.Khera R, Agrawal A. Conjoint bicondylar Hoffas fracture with ipsilateral femur and tibia shaft fracture in pediatric patient. Int J Orthop 2019;5:275-7. [Google Scholar]
- 11.Ostermann PA, Neumann K, Ekkernkamp A, Muhr G. Long term results of unicondylar fractures of the femur. J Orthop Trauma 1994;8:142-6. [Google Scholar]
- 12.Papadopoulos AX, Panagopoulos A, Karageorgos A, Tyllianakis M. Operative treatment of unilateral bicondylar Hoffa fractures. J Orthop Trauma 2004;18:119-22. [Google Scholar]
- 13.Neogi DS, Singh S, Yadav CS, Khan SA. Bicondylar Hoffa fracture? A rarely occurring, commonly missed injury. Injury Extra 2008;39:296-8. [Google Scholar]
- 14.Dua A, Shamshery PK. Bicondylar Hoffa fracture: Open reduction internal fixation using the swashbuckler approach. J Knee Surg 2010;23:21-4. [Google Scholar]
- 15.Hak DJ, Nguyen J, Curtiss S, Hazelwood S. Coronal fractures of the distal femoral condyle: A biomechanical evaluation of four internal fixation constructs. Injury 2005;36:1103-6. [Google Scholar]
- 16.Lee SY, Niikura T, Iwakura T, Sakai Y, Kuroda R, Kurosaka M. Bicondylar Hoffa fracture successfully treated with headless compression screws. Case Rep Orthop 2014;2014:139897. [Google Scholar]
- 17.Jarit GJ, Kummer FJ, Gibber MJ, Egol KA. A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B). J Orthop Trauma 2006;20:273-6. [Google Scholar]
- 18.Sun H, He QF, Huang YG, Pan JF, Luo CF, Chai YM. Plate fixation for Letenneur type I Hoffa fracture: A biomechanical study. Injury 2017;48:1492-8. [Google Scholar]
- 19.Trikha V, Das S, Gaba S, Agrawal P. Analysis of functional outcome of Hoffa fractures: A retrospective review of 32 patients. J Orthop Surg (Hong Kong) 2017;25:2309499017718928. [Google Scholar]
- 20.Calmet J, Mellado JM, García Forcada IL, Giné J. Open bicondylar Hoffa fracture associated with extensor mechanism injury. J Orthop Trauma 2004;18:323-5. [Google Scholar]