Whenever any swelling is present around any joint always suspect rare infections like mycetoma and tumor like lesions.
Dr. Nandlal Bharwani, C/O Dr. Chandan Prakash Bharwani Near Maloo Guest House, Gangashahar, Bikaner, Rajasthan, India. E-mail: nandlalbharwani21@gmail.com
Introduction:It is a form of chronic granulomatous infection involving skin, subcutaneous tissue, and skeletal system. The authors report a case of mycetoma presenting as knee swelling.
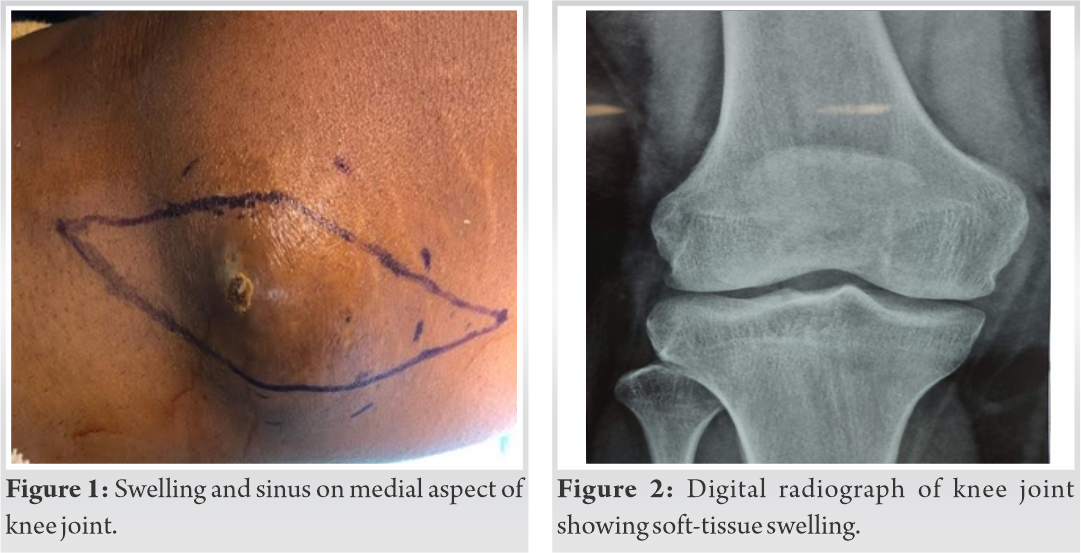
Case Report:A 25year old male presented to outdoor with painless swelling around medial aspect of the right knee joint with intermittent discharge of black granules from sinus since 6 months. The patient reported for mycetoma around knee joint belongs to Stage-B as per “Staging-classification of mycetoma.”
Conclusion:Knee mycetoma is a very rare presentation. Wide surgical excision and medical treatment are considered as gold standard.
Keywords:Knee joint, eumycetoma, sinues.
Maduramycosis or Madura foot is a common terms used for mycetoma [1]. It is a form of chronic granulomatous infection involving skin, subcutaneous tissue, and skeletal system [2]. The characteristic features of mycetoma are painless mass in subcutaneous region, grains, and multiple sinus formation. It is caused by bacteria (Actinomycetoma) and fungi (Eumycetoma) [2]. Males are commonly affected then females (Males:Females -3-4:1) as they are prone to injury while working in farms and fields [3].
Lower limb is involved more frequently and accounts for around 75% of the lesions [4]. Although mycetoma can affect any part, foot involvement is common in people who work barefooted in fields or farmyards [5]. Proper history, clinical examination, and diagnostic modalities such as digital radiographs and magnetic resonance imaging (MRI) help in defining the character of lesions and involvement of surrounding structures.
Fine-needle aspiration cytology, histopathological examination (HPE), Gram’s staining, and molecular investigations help in confirming the diagnosis.
Location, extent of the disease, and causative agent help in deciding the treatment plan and the outcome. Gold standard treatment is surgical and medical treatment, where medical treatment aims at making surgery feasible, reduces recurrence, and helps in healing [6, 7, 8, 9].
If not approached properly, it can lead to tissue destruction, deformities, superadded bacterial infections, and other fatal complications.
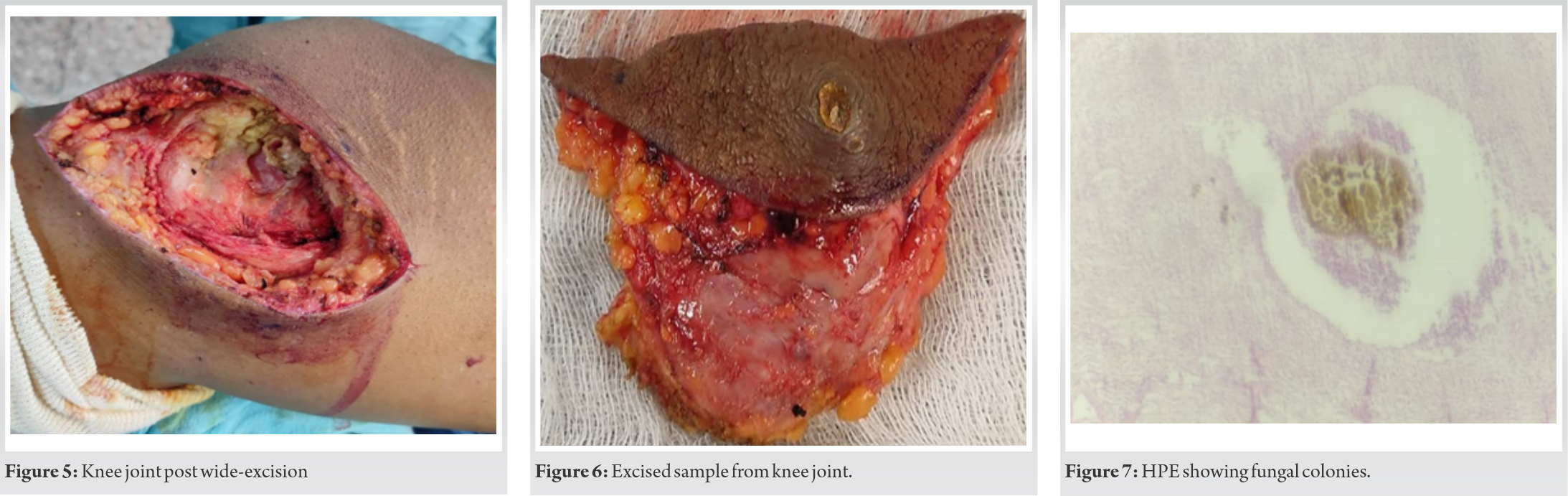
A 25year-old male presented to outdoor with painless swelling around medial aspect of the right knee joint with intermittent discharge of black granules from sinus since 6 months (Fig. 1). Proper history, clinical examination, digital radiographs (Fig. 2), and hematological investigations were performed. Above mentioned investigations were inconclusive so MRI knee joint (Fig. 3) was performed which showed involvement of skin and subcutaneous tissue around medial aspect of knee joint on coronal and sagittal sections.
The mycetoma around knee joint in this patient belonged to Stage-B as per “Staging-classification of mycetoma.”
Stage description
A.-Swelling and no sinuses
B.-Woody induration with sinuses/pustules
C.-Bone involvement on X-ray
D.-Spread to other sites/multiple lesions
Proper consent was taken before starting treatment. Preoperatively, there was no restriction in knee joint range of motion (ROM). Then, excisional biopsy was planned. The patient was laid supine in operation theatre, neuraxial anesthesia was given, painting and draping were done, and tourniquet was inflated to pressure of 320 mmHg. Then, fusiform skin incision was made around medial aspect of knee joint and subcutaneous dissection was performed followed by wide local excision (Fig. 4, 5). 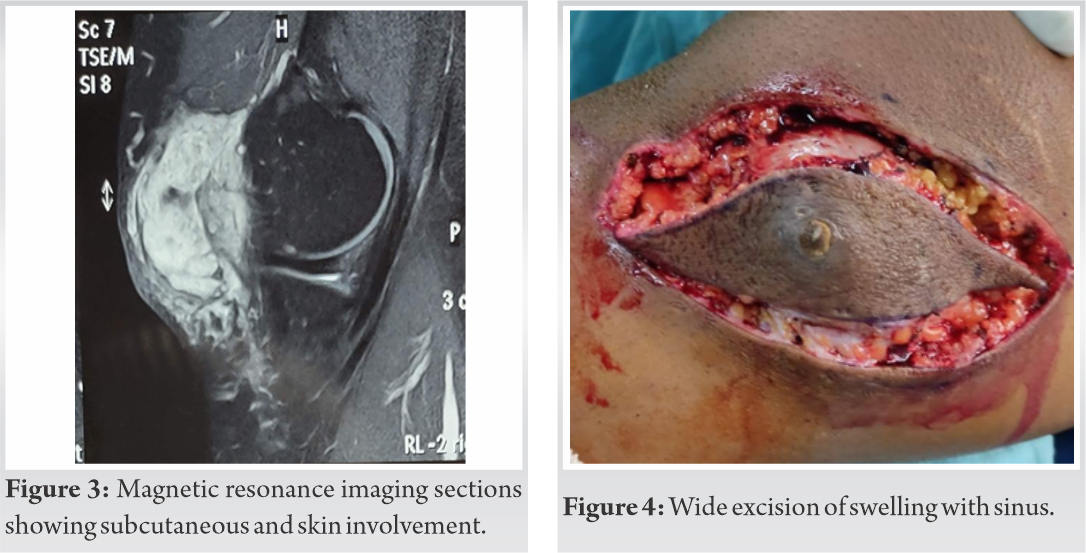
Size of excised tissue measures around 9 × 6 × 4 cm (Fig. 6) and sent for HPE, gram’s staining, and fungal culture.
Diagnosis was confirmed with reports of HPE (Fig. 7) and fungal culture on the basis of which medical treatment was started in the form of tablet itraconazole 200 mg twice a day for a period of 3 months. Knee joint ROM at final follow-up was normal.
The patient was followed for 1.5 years postoperatively and period was uneventful.
Maduramycosis is a form of chronic inflammatory disease causing severe tissue destruction and after treatment, chances of recurrence are very high [10]. Clinical features seen in patients presenting with maduramycosis are mostly similar and sometimes may present with atypical clinical features [1]. Thus, clinical history followed by proper physical examination plays a key role in making the diagnosis. Till date, very few cases for mycetoma around knee joint have been reported. The gold standard treatment for eumycetoma is medical and surgical which was performed for the present case in which we performed wide surgical excision and oral itraconazole 200 mg twice a day were given for 3 months. As ketoconazole has chances of causing liver toxicity, itraconazole was given to the patient instead of it.
Complications such as disability, deformity, and secondary infections would occur if proper treatment is not given [11].
This case demonstrates that Madurella mycetomatis is a common organism causing eumycetoma. A single staged treatment was performed consisting of wide excision supplemented with anti-fungal treatment which resulted in good clinical outcome in terms of pain and function at 1.5 years of follow-up.
Although foot involvement is common in patients with mycetoma, we present a rare case of knee joint mycetoma, where if proper diagnosis and treatment were not done, it could have led to multiple surgeries and ultimately amputation of the extremity.
References
- 1.Suneet S, Anurag K. Surgical Diseases in Tropical Countries. New Delhi, India: Jaypee Brothers; 1996. [Google Scholar]
- 2.Baki R, Mathur DR. Incidence and changing pattern of mycetoma in western Rajasthan. Indian J Pathol Microbiol 2008;51:154-5. [Google Scholar]
- 3.Welsh O, Vera-Cabrera L, Salinas-Carmona MC. Mycetoma. Clin Dermatol 2007; 25:195-202. [Google Scholar]
- 4.Mahgoob ES. Mycetoma. In: Guerrant RL, Walker DH, Weller PF, editors. Tropical Infectious Diseases: Principles, Pathogens and Practice. 1st ed. New York: Churchill Livingstone; 2000. p. 616-20. [Google Scholar]
- 5.Van de Sande WW. Global burden of human mycetoma: A systematic review and meta-analysis. PLoS Negl Trop Dis 2013;7:e2550. [Google Scholar]
- 6.Fahal AH. Mycetoma: A thorn in the flesh. Trans R Soc Trop Med Hyg 2004;98:3-11. [Google Scholar]
- 7.Fahal AH. Mycetoma. In: Williams NS, Bulstrode CJ, O’Connell PR. Bailey and Love’s Short Practice of Surgery. 26th ed. Oxford: Oxford University Press; 2013. p. 64-8. [Google Scholar]
- 8.Fahal AH. Management of mycetoma. Expert Rev Dermatol 2010;5:87-93. [Google Scholar]
- 9.Gumaa SA, Mahgoub ES, El Sid MA. Mycetoma of the head and neck. Am J Trop Med Hyg 1986;35:594-600. [Google Scholar]
- 10.Rajkumar SA, Angamuthu N. Multiple foot sinues due to schizomycetes. Indian J Orthop 2005;39:125-6. [Google Scholar]
- 11.Lichon V, Khachemoune A. Mycetoma: a review. Am J Clin Dermatol 2006;7:315-21. [Google Scholar]