Recurrent Giant Cell Tumors predispose to metastasis, and hence warrant evaluation for pulmonary metastasis.
Dr. Satvik N Pai, Department of Orthopaedic Surgery, Sri Ramachandra Institute of Higher Education and Research, No.1, Ramachandra Nagar, Porur, Chennai, Tamil Nadu, India. E-mail: satvik.pai@gmail.com
Introduction:Giant cell tumor (GCT) is a rare, locally aggressive tumor of bone characterised by the presence of abundant giant cells. GCT has a tendency for recurrence, occurring in approximately a quarter of cases. GCT very rarely metastasize, with metastasis to lungs being reported in approximately 1% of GCTs.
Case Presentation:A 48 year -year-old gentleman noticed a swelling around his left wrist. Radiograph showed a lytic lesion in the distal radius having typical soap bubble appearance. He underwent left distal radius curettage and bone cement placement. The histopathological examination of excised tissue confirmed the diagnosis of GCT. Patient then had recurrence of the tumor 6 months after the surgery. He underwent left distal radius resection, fibular grafting, and wrist arthrodesis. Resected tissue on histopathological examination showed features consistent with GCT. One year later, patient noticed multiple swellings in the region of his left wrist. On examination, there were multiple bony hard, non-tender swellings over the distal forearm. Radiographs revealed a lytic lesion in the fibular strut graft with breach of the cortex. Patient was diagnosed to have recurrence for GCT for the second time. Chest radiograph and Computed Tomography (CT) scan of the thorax revealed multiple canon ball lesions in bilateral lungs, suggesting a metastasis of GCT. The patient, however, did not have any respiratory complaints. We then performed an excision of the tumor, removal of plate and k-wire, and applied a wrist spanning external fixator. Histopathological examination confirmed a recurrence of GCT. The patient was not willing for metastasectomy. The patient was followed up for a period of 18 months. We found no clinical, radiological evidence of recurrence. The metastatic lesions in the lungs were not found to have increased in number or size, while the patient remained asymptomatic.
Conclusion:Giant cell tumours are benign, however, they have a propensity for recurrence. Recurrent GCT are more likely to lead to pulmonary metastasis, and thus warrant pulmonary evaluation. Pulmonary metastasis has a favourable outcome with only half the cases having progression.
Keywords:giant cell tumor, recurrent, pulmonary, metastasis, distal radius.
Giant cell tumor (GCT) of bone is a rare, locally aggressive tumor of bone characterized by the presence of abundant giant cells [1]. It accounts for 5% of primary bone tumors and 20% of benign bone tumors [2]. It occurs most commonly in individuals aged 2040 years and has preponderance for females [3]. The most common sites include the distal femur, proximal tibia, and distal radius [1]. Radiographs show a typical eccentric lytic lesion, mostly located in the meta-epiphyseal area of long bones [2]. Histologically, these tumours are comprised of mononuclear cells, macrophages and uniformly distributed multinuclear giant cells [4]. Standard treatment consists of consists of extensive curettage and filling of the cavity with bone graft or cement, with some preferring to supplement with local adjuvant therapy [5]. GCT is known to have a tendency for recurrence, with recurrence occurring after treatment in approximately a quarter of cases [6]. GCTs very rarely turn malignant, with metastasis occurring in just 1% of GCTs [7]. The lungs are the most common site of metastasis of GCT, with it accounting for 25% of the cases of metastasis [7]. We report a case of recurrent giant cell tumor of the distal radius, with metastasis to lungs.
A 48-year-old man noticed a swelling around his left wrist two and a half years ago. The swelling gradually increased in size over 6 months. Radiograph of the wrist showed a lytic lesion in the distal radius having typical soap bubble appearance. He was diagnosed to have a giant cell tumor of the distal radius. His chest radiograph at the time was normal. He underwent left distal radius curettage and bone cement placement 2 years back. The Histopathological examination of excised tissue showed mononuclear stromal cells, macrophages, and multiple multinuclear giant cells, thereby confirming the diagnosis of GCT. The patient then had a recurrence of the swelling after 6 months of the surgery. Radiographs (Fig. 1) and Magnetic Resonance Imaging (MRI) (Fig. 2) suggested recurrence of tumor. His chest radiograph at this time also was normal.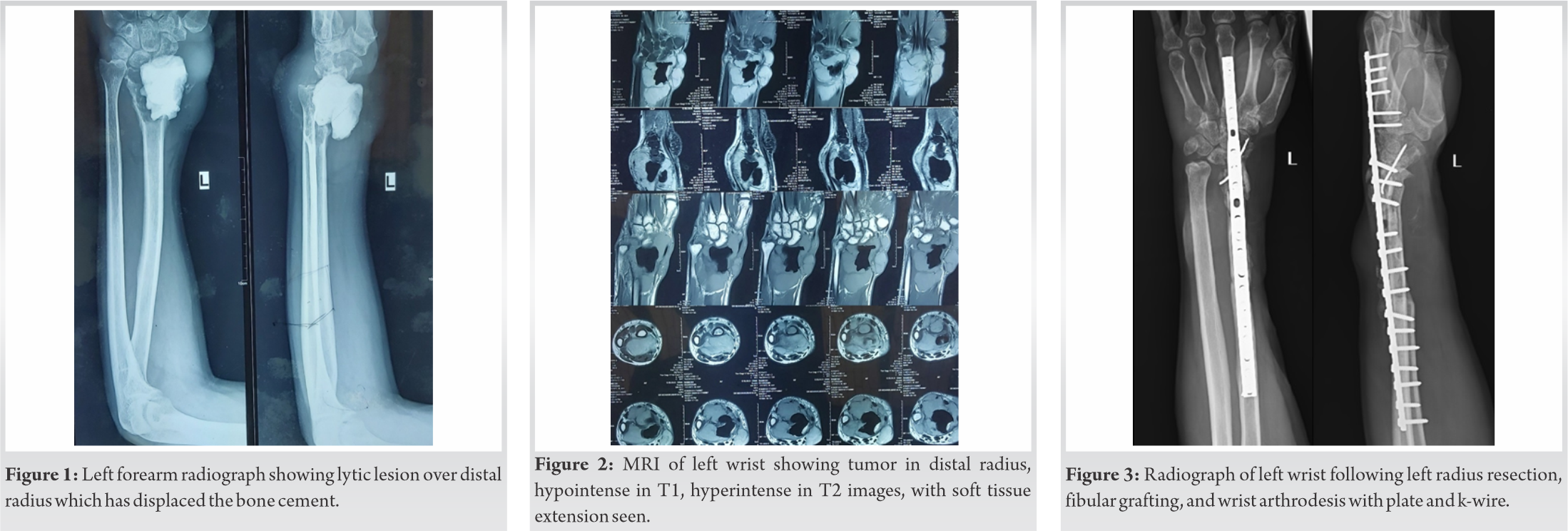
On examination, there were multiple bony swellings over the left distal forearm and wrist region, involving the volar and dorsal aspect, radial and ulnar sides, with the largest swelling being of the size 4 cm × 3.5 cm (Fig. 4). The swellings were hard in consistency and non-tender. The abdominal flap over the distal forearm and wrist was found to be healthy. Healed surgical scars from previous surgeries were also present over the dorsal aspect. The fingers were sensate and capillary refill in the fingers was satisfactory. However grip strength (Left – 12 kg, right – 34 kg) and pinch strength (left – 4.5 kg, Right – 7.5 kg) were decreased on the left side.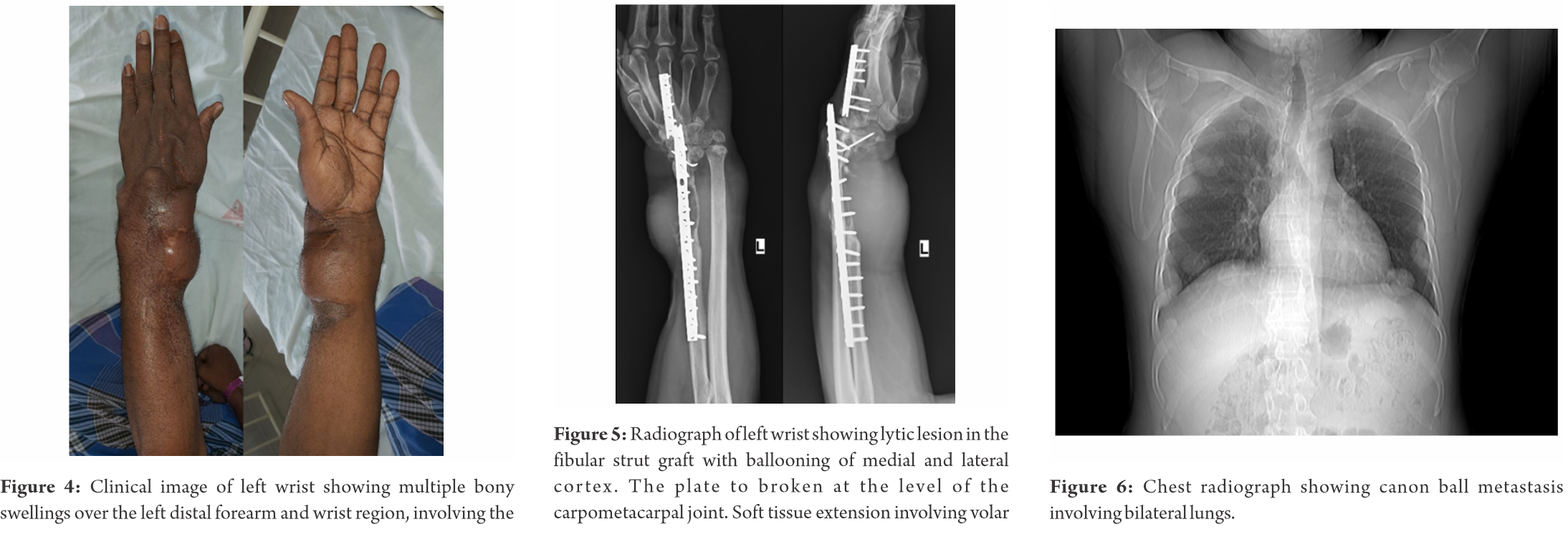
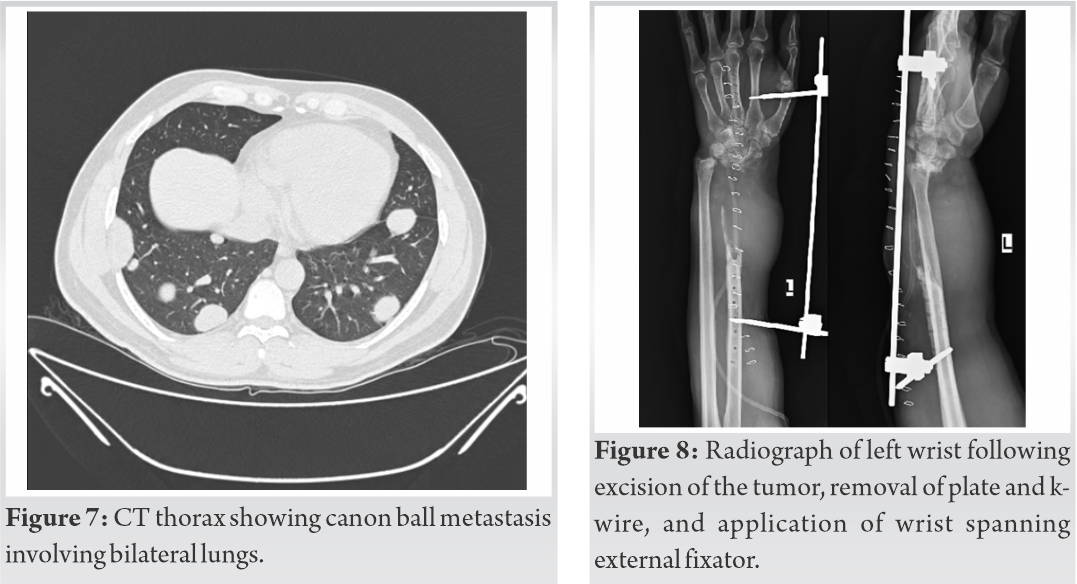
All routine blood investigations were found to be within normal limits. Radiographs (Fig. 5) revealed a lytic lesion in the fibular strut graft, causing ballooning of the medial cortex and breach of the lateral cortex. The lesion had destructed most of the fibular strut graft including the distal portion which was fixed to the carpal bones by a k-wire. The instability at the wrist joint, had caused the plate to break. Swellings were also visible within the soft tissue of the distal forearm, involving volar and dorsal aspects of the forearm. Patient was diagnosed to have a recurrence for GCT for the second time. It was classified as Grade 3 (aggressive) as per Campanacci classification system and Enneking classification system owing to the cortical breach and soft tissue extension. Further work up was done, chest radiograph (Fig. 6) and Computed Tomography (CT) scan of the thorax (Fig. 7) revealed multiple canon ball lesion in bilateral lungs, suggesting a metastasis of GCT. The patient however did not have any respiratory complaints. We obtained the opinion of an oncologist, who advised metastasectomy. We then performed an excision of the tumor, removal of plate and k-wire, and applied a wrist spanning external fixator (Fig. 8). The resected tissue on Histopathological examination again revealed mononuclear stromal cells, macrophages and multiple multinuclear giant cells, thereby confirming a recurrence of the GCT. The patient was not willing for metastasectomy. The patient followed up with us for a period of 18 months following the surgery. We found no clinical, radiological evidence of recurrence. The metastatic lesions in the lungs were not found to have increased in number or size, while the patient remained asymptomatic.
GCT’s are can often by diagnosed on radiographs. However, it is recommended to always also perform an MRI to rule out soft tissue extension. The role of CT is limited in terms of diagnosis, with it being useful mainly to detect any pathological fractures. A histopathological confirmation of the tumor is always recommendable [2]. Despite GCT’s being a predominantly benign condition, they are known to recur after primary treatment. The rates of recurrence of GCT is a matter of speculation with a wide range of reports recurrence rates in literature. Xu et al. [8] in their study found the rate of recurrence to be 2.1% (6 out of 291 patients with GCT developed recurrence of GCT after surgical excision). The mean interval between initial surgery and recurrence is 11.3 ± 4.1 months (range 517 months). Soft tissue extension of the tumor has been identified as a risk factor for recurrence [6]. Age of the patient, sex, and presence of pathological fracture were not found to have a correlation with the chance of recurrence. The use of polymethylmethacrylate (PMMA) as an adjuvant significantly has been suggested to reduce the recurrence rate following intralesional treatment of benign GCTs [9], however recurrence-free survival for PMMA and phenol and for PMMA alone has been found to be similar [6]. Most studies suggest no correlation between the locations of GCT to the rate of recurrence, but Siddiqui et al. [10] found that GCTs in the proximal tibia were more likely to recur. The use of adjuvants such as liquid nitrogen, phenol, or argon beam coagulation, paired with intralesional curettage decrease the rate of recurrence [9]. For expandable bones such as the lower ulnar end, upper fibular end, excision an option to decrease risk of recurrence. Wide resection has also been shown to decrease the risk of recurrence for all GCTs, however, associated with higher rates of surgical complications and leads to functional impairment requiring reconstruction [3]. In our case, the primary treatment given was curettage with bone cement packing, still the tumor recurred 6 months after the primary surgery. Following the second surgery involving resection of the distal radius and replacing it with a fibular strut graft, patient developed another recurrence 18 months following the second surgery, which may have been due to insufficient excision of soft tissue component of the tumor in the 2nd surgery.
Patients having recurrence of GCT, are more likely to develop pulmonary metastasis of the GCT [11]. Metastasis of GCT has been found more common in males than female counterparts. The median age of patient with metastasis from GCT was 26 years, with the metastasis occurring at an average of 2 years following initial diagnosis [7].While lungs are the most common site of distant metastasis from GCT, cases have been reported of metastasis to scalp, calf muscles and regional lymph nodes. Lung surveillance has been recommended for all patients with recurrent GCT, especially for 3 years from the time of local recurrence, with CT of the thorax being an effective diagnostic tool [12]. The overall prognosis of pulmonary metastasis is favorable, with disease progression after detection pulmonary metastasis occurring in only about half the patients [13]. Hemoptysis is a complication which can occur, however the pulmonary metastasis has rarely been found to be fatal [7]. Observation is an acceptable first-line method of managing patients with pulmonary metastases [13]. Metastasectomy has been recommended in feasible cases [7]. In our case, after discussion with the patient about the treatment options, we recommended metastasectomy, however patient preferred to avoid surgery for it.
Giant cell tumors are benign, however they have a propensity for recurrence. Recurrent GCT are more likely to lead to pulmonary metastasis, and thus warrant pulmonary evaluation. Pulmonary metastasis has a favourable outcome with only half the cases having progression.
Giant cell tumors are benign, but have a propensity for recurrence. Recurrent GCTs predispose to metastasis, and hence warrant pulmonary evaluation. Pulmonary metastasis from GCT has a favorable outcome and can be managed by observation and regular follow-up.
References
- 1.Verschoor AJ, Bovée JV, Mastboom MJ, Dijkstra PD, Van De Sande MA, Gelderblom H. Incidence and demographics of giant cell tumor of bone in The Netherlands: First nationwide pathology registry study. Acta Orthop. 2018;89:570-4. [Google Scholar]
- 2.Van der Heijden L, Dijkstra PD, van de Sande MA, Kroep JR, Nout RA, van Rijswijk CS, et al. The clinical approach toward giant cell tumor of bone. Oncologist 2014;19:550-61. [Google Scholar]
- 3.Karpik M. Giant Cell Tumor (tumor gigantocellularis, osteoclastoma) epidemiology, diagnosis, treatment. Ortop Traumatol Rehabil 2010;12:207-15. [Google Scholar]
- 4.Çomunoğlu N, Kepil N, Dervişoğlu S. Histopathology of giant cell tumors of the bone: With special emphasis on fibrohistiocytic and aneurysmal bone cyst like components. Acta Orthop Traumatol Turc 2019;53:35-9. [Google Scholar]
- 5.Turcotte RE. Giant cell tumor of bone. Orthop Clin North Am 2006;37:35-51. [Google Scholar]
- 6.Van der Heijden L, van de Sande MA, Dijkstra PD. Soft tissue extension increases the risk of local recurrence after curettage with adjuvants for giant-cell tumor of the long bones. Acta Orthop 2012;83:401-5. [Google Scholar]
- 7.Viswanathan S, Jambhekar NA. Metastatic giant cell tumor of bone: Are there associated factors and best treatment modalities? Clin Orthop Relat Res 2010;468:827-33. [Google Scholar]
- 8.Xu L, Jin J, Hu A, Xiong J, Wang D, Sun Q, et al. Soft tissue recurrence of giant cell tumor of the bone: Prevalence and radiographic features. J Bone Oncol 2017;9:10-4. [Google Scholar]
- 9.Arbeitsgemeinschaft Knochentumoren, Becker WT, Dohle J, Bernd L, Braun A, Cserhati M, et al. Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy. J Bone Joint Surg Am 2008;90:1060-7. [Google Scholar]
- 10.Siddiqui MA, Seng C, Tan MH. Risk factors for recurrence of giant cell tumours of bone. J Orthop Surg (Hong Kong) 2014;22:108-10. [Google Scholar]
- 11.Muheremu A, Niu X. Pulmonary metastasis of giant cell tumor of bones. World J Surg Oncol 2014;12:261. [Google Scholar]
- 12.Rosario M, Kim HS, Yun JY, Han I. Surveillance for lung metastasis from giant cell tumor of bone. J Surg Oncol 2017;116:907-13. [Google Scholar]
- 13.Tsukamoto S, Ciani G, Mavrogenis AF, Ferrari C, Akahane M, Tanaka Y, et al. Outcome of lung metastases due to bone giant cell tumor initially managed with observation. J Orthop Surg Res 2020;15:510. [Google Scholar]