An extra-epiphyseal, over-the-top, bony-tunnel free ACL reconstruction with an Achilles tendon allograft is an effective solution for the treatment of ACL agenesis in an Ehlers Danlos pediatric patient with open physes.
Dr. Pietro Conte, Department of Biomedical Sciences, Humanitas University, Milan, Italy. E-mail: pietro.conte@humanitas.it
Introduction: The agenesis of the anterior cruciate ligament (ACL) is a rare condition infrequently diagnosed as an isolated malformation. Still, it is linked to systemic disorders such as Ehlers-Danlos syndrome (EDS), an inheritable connective tissue disorder characterized by joint hyperlaxity and increased risk of dislocations and subluxations. The literature on ACL reconstruction in EDS patients is minimal, and ours is the second case report describing the surgical management of an ACL agenesis in a patient with this pathology.
Case Presentation:The present case report describes the surgical management of an 11-year-old patient affected by EDS. The particularity of this case is that the young patient presented with complete agenesis of the ACL in the right knee resulting in severe joint instability needing surgical reconstruction. This case represented a challenge for the orthopedic surgeon due to the need to improve joint stability without compromising the bone growth of a young patient with open physes while also dealing with tissues that have reduced mechanical properties due to the patient’s disease. The patient was therefore treated with an Achilles tendon allograft through a modified version of the typical ACL reconstructive surgery that excluded the classical tunnel drilling in the tibia and femur.
Conclusion:At a 2-year follow-up, this technique proved to be an effective treatment for ACL agenesis in an EDS patient. It could provide a reference for surgeons facing similar cases. The proposed surgical technique, completely extra-epiphyseal, could also be applied to healthy young patients with open physes to avoid future growth disturbances.
Keywords:Anterior cruciate ligament, anterior cruciate ligament agenesis, Ehlers-Danlos, pediatric anterior cruciate ligament reconstruction, anterior cruciate ligament reconstruction, anterior cruciate ligament agenesis.
Ehlers-Danlos syndrome (EDS) is a hereditary disorder affecting connective tissue [1] with an estimated incidence of 1 in 5000 live births [2]. At a genetic level, EDS is caused by mutations with autosomal transmission affecting genes coding for collagen; these lead to a wide variety of dermatological, musculoskeletal, and cardiovascular manifestations [3]. Joint hypermobility and skin hyperextensibility are the most common clinical findings, predominantly involving the knee and shoulder joints [4]. Depending on the soft-tissue involvement severity, the clinical picture can range from little soft-tissue involvement to severe biomechanical impairment, such as soft-tissue agenesis, recurrent dislocations, and progressive cartilage damage. This was the case of the present EDS patient who came to our attention reporting right knee instability and was diagnosed with complete agenesis of the anterior cruciate ligament (ACL). Giorgi first described ACL agenesis as a rare condition with a prevalence of 0.017 per 1000 live births [5]. It can be an isolated finding, but it is frequently associated with various other intra-articular or systemic conditions, EDS being one of these. There is limited evidence in the existing literature regarding the outcomes of ACL reconstruction in EDS patients with open physes in concomitance with an ACL insufficiency, the latter either due to agenesis or traumatic tear. Here, we report the case of an 11-year-old patient, affected by EDS with consequent ACL agenesis that successfully underwent an all extra-epiphyseal, tunnel-free, and ACL reconstruction with an Achilles tendon allograft.
An 11-year-old boy with a known clinical diagnosis of EDS presented to our department in 2017 with a history of bilateral knee instability associated with recurrent episodes of multiple atraumatic subluxations of the knee, particularly the right one. Physical examination revealed an unswollen right knee with preserved range of motion and bilateral knee procurvatum that was more prominent on the right side. Lachman test and anterior drawer test on the right knee both confirmed the anterior instability reported by the patient, and the dislocation could be reduced manually. No insufficiency of the collateral ligaments was observed. The posterolateral and posteromedial corners appeared functionally valid bilaterally. A weight-bearing X-ray image of the right knee revealed a posterior subluxation of the femoral condyles with respect to the tibial plates, as well as a patellar deformation (Fig. 1).
An MRI of the right knee (Fig. 2) revealed agenesis of both the anterior and the posterior cruciate ligaments (PCLs). As per the classification proposed by Manner et al. [6], the malformation was diagnosed as a Type III deformity (combined ACL and PCL agenesis). Despite the absence of the PCL, posterior instability of the right knee was minimal.
After discussing with the patient and his parents and considering the clinical findings that revealed a prominent anterior instability, an isolated ACL reconstruction of the right knee was proposed to reduce the dislocation and restore the knee’s stability. As the X-rays demonstrated, the patient had open physes in both the tibia and femur. Therefore, it was necessary to perform a physeal-sparing technique to avoid any interference with skeletal growth and alignment. Furthermore, due to the patient’s known connective tissue disorder, we decided to reconstruct the ACL with an Achilles tendon allograft to avoid using an autologous tendon and preserve the patient’s hamstring and patellar tendons.
Several physis-sparing techniques have been described in the existing literature, and in this case, an over-the-top approach was selected based on the experience of the primary surgeon [7]. Conventionally, this technique already avoids the drilling of a femoral tunnel. The graft is brought in the over-the-top position through a small hole in the posterior capsule of the knee, through which it is then passed to reach its final extra-articular position for fixation, achieved with the use of two titanium staples. In contrast to the traditional technique, in our case, the drilling of the tibial tunnel was also avoided (Fig. 3). Instead, a central sulcus 6 mm in length was created that passed under the intermeniscal ligament and reached the anterior tibial spine where it was then distally fixed with two metal staples. It was then passed through this sulcus into an ACL position through the posterior capsule through an incision and proximally fixed on the lateral femoral condyle in an over-the-top position with two metal staples as previously mentioned for the standard technique.
The classical tibial drilling could not be used on an 11-year-old patient as it would have caused a biomechanical impairment of growth of the epiphyseal plates.
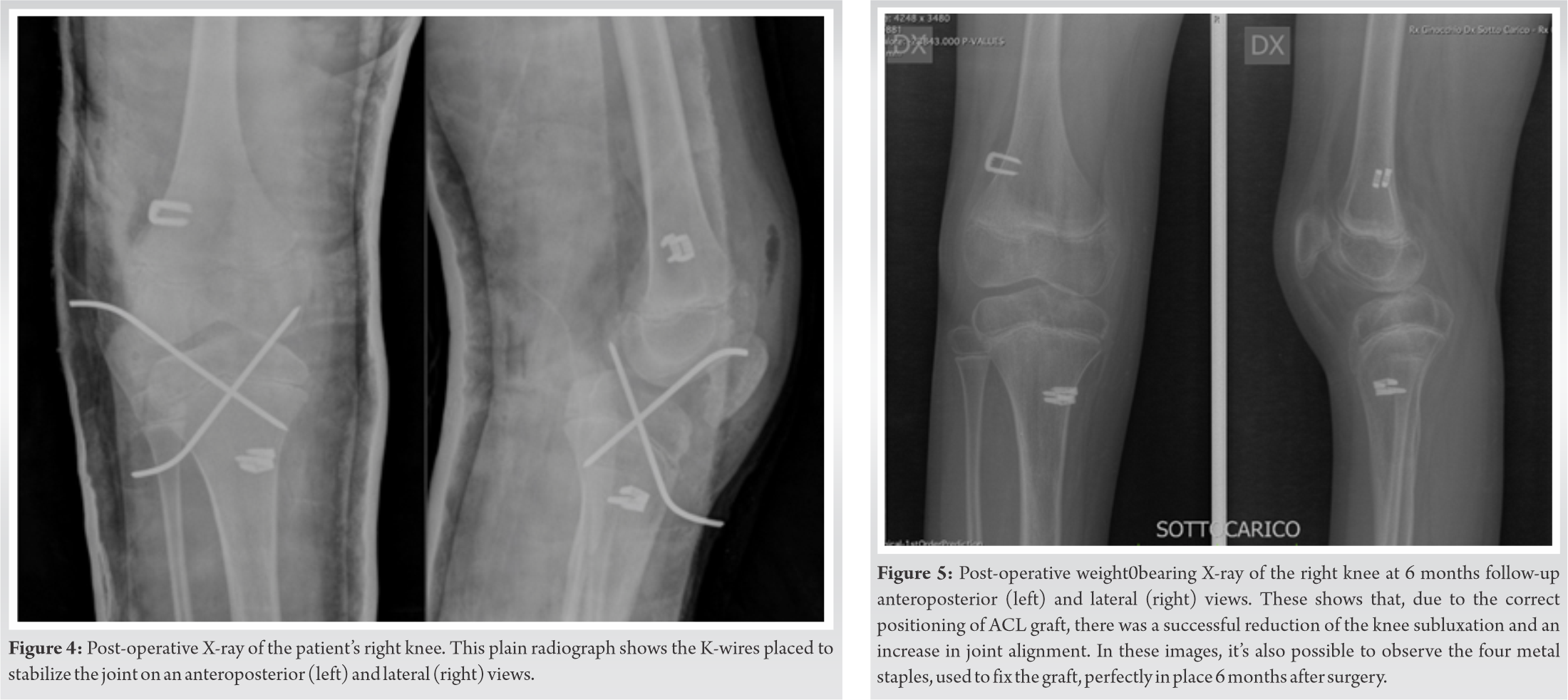
Due to the level of joint instability and the altered composition of the patient’s connective tissues, the surgeon also decided to strengthen the ACL reconstruction by positioning two crossed Kirschner wires through the joint (Fig. 4). This was done to help prevent further knee subluxations that could lead to graft failure in the 1st month after the surgery.
Outcome and follow-up
The patient was discharged from our hospital 3 days after surgery in good general condition. The operated knee was unswollen and maintained in a brace in full extension for the first 30 days. Weight-bearing was not permitted for the 1st month, and only isometric exercises were prescribed as tolerated. One month later, the transarticular K-wires were removed. The patient was allowed progressive weight-bearing with two crutches for the following month, together with range of motion and muscle strengthening exercises. Full weight-bearing without crutches was reached at 70 days post-operative.
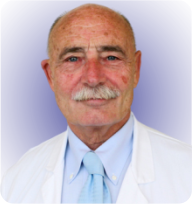
X-ray images (bilateral and weight-bearing) performed at 6 months after surgery demonstrated improved knee alignment and joint congruency (Fig. 5). These images also showed no signs of bone resorption or focal bone lesions were observed. Imaging repeated a year later showed, compared to the previous examination, increased development and calcification of the metaphyseal cartilages of the proximal tibia, proximal fibula, and distal femur. Further imaging performed 2 years later showed an intact bone structure and growth, without any complications regarding malalignment or limb lengths discrepancies. The clinical evaluation at 2 years demonstrated good right knee stability with a negative Lachman and anterior drawer test. The patient was satisfied with the clinical outcome of the surgery, and no further subluxation episodes were registered.
Despite extensive knowledge on the treatment of traumatic ACL injury in healthy patients, there are only a few studies on how to manage such injuries in patients with EDS, especially in children with open physes. We conducted a detailed literature review on the PubMed database searching for reports on the surgical management of ACL tears and agenesis in patients with Ehlers-Danlos syndrome. Titles including the words “ACL agenesis,” “ACL tear,” “Ehlers-Danlos syndrome,” and “pediatric ACL reconstruction” were reviewed and analyzed. Our research pointed out that this is just the second case report describing an ACL reconstruction for ACL agenesis in EDS patients. Our research found two similar case reports of ACL reconstruction in EDS patients following a traumatic ligament tear. Williams et al. [8] described the case of an 18-year-old boy with a known diagnosis of EDS presenting with a traumatic full-thickness tear of ACL that was successfully treated with arthroscopic ACL reconstruction using a technique consisting of a combination of ipsilateral hamstring autograft and Ligament Advanced Reinforcement System (LARS) synthetic ligament. Similarly, Choi et al. [9] described an ACL reconstruction in a 25-year-old EDS patient presenting severe traumatic knee instability. The patient was successfully treated with ACL reconstruction with an Achilles tendon allograft.
The patients mentioned above, differently from ours, were adults, and had closed growth plates. Therefore, they were treated with a standard ACL reconstruction technique involving the drilling of both the femoral and tibial tunnels and the use of classical fixation devices (Endobutton and screws). The only other report of an ACL reconstruction for ACL agenesis in an EDS patient is the one by Erdman and Warnick who described the initial failure of a non-anatomic physeal-sparing iliotibial (IT) band autograft, which was then followed by an all-epiphyseal revision ACL reconstruction with a posterior tibialis allograft [10]. This report, together with ours, is the only evidence of ACL reconstructions in a pediatric EDS patient with open growth plates. It is of note that the first ACL reconstruction revision they performed at 10 years of age, both the femoral and tibial tunnel were drilled after fluoroscopic images confirmed that the guide pin would not cross the physis. There is no consensus for the optimal treatment of ACL agenesis, neither in healthy nor in EDS patients. Some authors consider conservative treatment the best option since most patients remain asymptomatic or do not mention significant joint instability [11, 12]. However, a study by Gabos et al. [13] reported a better outcome in symptomatic patients treated with surgical ACL reconstruction compared to the non-operative group. Furthermore, a recent review by Dingel et al. [14] noted that pediatric ACL injuries treated non-operatively often lead to secondary meniscal and/or cartilage damage which may lead to even greater joint instability and knee degeneration. Early operative management is, therefore, frequently considered the best therapeutic option in most pediatric ACL injuries. In these cases, there are two main choices to be made: The surgical technique to adopt to prevent physeal damage and consequent growth deformities, and the graft to use to ensure sufficient strength and stability.
Regarding the surgical technique, general treatment recommendations are that prepubescent patients (boys ≤ 12 and girls ≤ 10) are treated with a physeal-sparing reconstruction, adolescent patients (boys: 13–14, girls: 11–12) with a transphyseal reconstruction, and older adolescents (boys ≥ 15 and girls ≥ 13) with a conventional ACL reconstruction [15]. The patient was 11 years old in our case, so an extra-epiphyseal bony tunnel-free technique was performed to prevent future growth disturbances. As for the graft type, surgical reconstructions of the ACL can be done using autografts, allografts, or synthetic materials. We chose to use an allograft due to the biomechanical compromise of the patient’s connective tissue due to EDS, as an autograft would probably lead to the reconstruction’s instability and failure. This choice was also supported by the satisfactory experiences on EDS patients reported by Choi et al. [9] who used an Achilles tendon allograft. Furthermore, Erdman and Warnick [10], who had a failure of the previously used IT band autograft, then successively performed a revision reconstruction using a posterior tibialis allograft. On the other hand, Williams et al. [8] used a hamstring autograft but reinforced it with a LARS synthetic ligament.
Due to the patient’s young age and clinical condition (ACL agenesis in EDS), we decided to use an extra-epiphyseal, over-the-top, and bony tunnel-free technique with an Achilles’ tendon allograft to restore proper knee stability without impairing the skeletal growth and alignment of the patient.
As uncommon as EDS might be, it must be considered when dealing with patients presenting with recurrent joint instability and alterations in soft-tissue integrity. ACL agenesis is a rare condition that must be surgically addressed when it leads to joint instability and functional impairment. A consensus on the best treatment option has not yet been achieved. In the case of orthopedic surgery of pediatric patients with open physes, it is essential to adopt a technique that spares the epiphyseal plates to preserve the growth potential of the bone. Consequently, for our case, we modified our approach to prevent drilling through tibial and femoral epiphyses applying an all-extra-epiphyseal technique. When treating ACL injuries in patients with connective tissue disorders, such as EDS, an Achilles tendon allograft can provide good clinical results given the better strength and stability when compared to the use of an autograft in a patient with compromised connective tissue to the disorder.
References
- 1.Shirley ED, Demaio M, Bodurtha J. Ehlers-danlos syndrome in orthopaedics: Etiology, diagnosis, and treatment implications. Sports Health 2012;4:394-403. [Google Scholar]
- 2.Genetic Home Reference. Ehlers-Danlos Syndrome. Bethesda, MD: National Institutes of Health; 2016. [Google Scholar]
- 3.Byers PH. Ehlers-Danlos syndrome: Recent advances and current understanding of the clinical and genetic heterogeneity. J Invest Dermatol 1994;103 Suppl 5:47S-52. [Google Scholar]
- 4.Stanitski DF, Nadjarian R, Stanitski CL, Bawle E, Tsipouras P. Orthopaedic manifestations of Ehlers-Danlos syndrome. Clin Orthop Relat Res 2000;376:213-21. [Google Scholar]
- 5.Giorgi B. Morphologic variations of the intercondylar eminence of the knee. Clin Orthop 1956;8:209-17. [Google Scholar]
- 6.Manner HM, Radler C, Ganger R, Grill F. Dysplasia of the cruciate ligaments: Radiographic assessment and classification. J Bone Joint Surg 2006;88A:130-7. [Google Scholar]
- 7.Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A. Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 1998;6:68-75. [Google Scholar]
- 8.Williams J, Hutt J, Rickman M. Anterior cruciate ligament reconstruction in ehlers-danlos syndrome. Case Rep Orthop 2015;2015:160381. [Google Scholar]
- 9.Choi J, Naito K, Curry EJ, Li X. Anterior cruciate ligament reconstruction with achilles tendon allograft in a patient with Ehlers-Danlos syndrome. Orthop J Sports Med 2018;6:2325967118785170. [Google Scholar]
- 10.Erdman MK, Warnick DE. Revision pediatric anterior cruciate ligament reconstruction after failure of iliotibial band technique treated with all-epiphyseal technique in a prepubescent with Ehlers-Danlos syndrome: A case report. J Pediatr Orthop B 2017;26:470-6. [Google Scholar]
- 11.Bossche SV, Vanzieleghem B, Declercq H, Verstraete KV. Absent anterior cruciate ligament. J Belg Soc Radiol 2015;99:31-3. [Google Scholar]
- 12.Balke M, Mueller-Huebenthal J, Shafizadeh S, Liem D, Hoeher J. Unilateral aplasia of both cruciate ligaments. J Orthop Surg Res 2010;5:11. [Google Scholar]
- 13.Gabos PG, El Rassi G, Pahys J. Knee reconstruction in syndromes with congenital absence of the anterior cruciate ligament. J Pediatr Orthop 2005;25:210-4. [Google Scholar]
- 14.Dingel A, Aoyama J, Ganley T, Shea K. Pediatric ACL Tears: Natural History. J Pediatr Orthop. 2019 Jul;39(Issue 6, Supplement 1 Suppl 1):S47-S49 [Google Scholar]
- 15.Perkins CA, Willimon SC. Pediatric Anterior Cruciate Ligament Reconstruction. Orthop Clin North Am. 2020 Jan;51(1):55-63. doi: 10.1016/j.ocl.2019.08.009. Epub 2019 Oct 21. PMID: 31739879. [Google Scholar]