Although leiomyomas are commonly seen in females, they are an important differ-ential of soft tissue/bony lesions in the spine and occasionally occur even in immunocompetent males.
Dr. Rohan B. Gala, Department of Orthopaedics, D.Y. Patil University- School of Medicine, Navi Mumbai, Maharashtra, India. E-mail: drrohangala17@gmail.com
Introduction:Leiomyomas are benign epithelial tumors with a female preponderance usually in the uterus, gastro-intestinal tract and skin. They are well-capsulated tumors with no mitotic activity and little pleomorphism. Primary leiomyoma in the upper cervical spine region is rare and the occurrence of these lesions in young immunocompetent males is extremely rare.
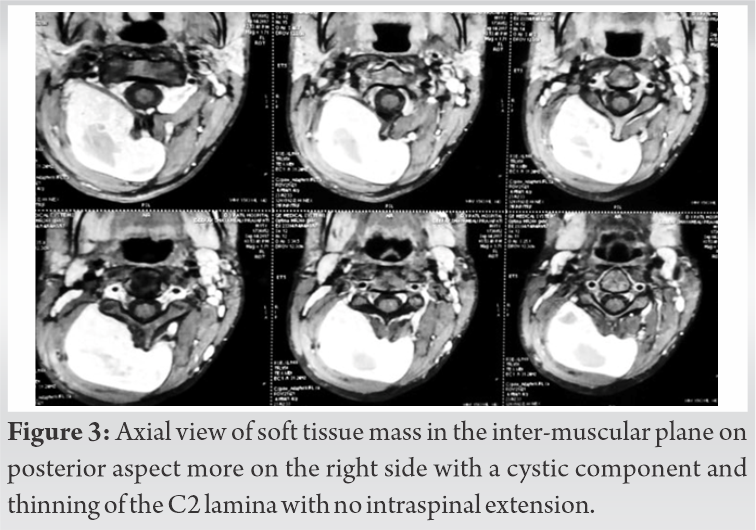
Case Report: A 15-year-old male had swelling over the nape of the neck for 4 years with slight difficulty in neck movements for a few months. Asymptomatic 4 years back be developed a painless swelling at the nape of the neck on the right side initially the size of a pea which gradually increased size. A 10x8cm firm, on-tender and non-pulsatile swelling at the nape of the neck on the right extending from the occipital nuchal line and crossing the midline up to the posterior border of the sternomastoid. The skin over the swelling wasn’t adherent and the swelling did not reduce on neck movements. Neck movements were terminally restricted with restriction on rotation towards the right. Routine X-ray’s and magnetic resonance imaging were suggestive of a soft tissue mass in the inter-muscular plane on the posterior aspect more on the right side with a cystic component and causing thinning of the C2 lamina with no intraspinal extension. Biopsy was done. Findings were suggestive of a spindle cell benign tumor. Posterior en bloc excision was planned and the lesion blog with the entire capsule was excised and sent for histopathology which revealed the lesion was a leiomyoma. The patient has shown no clinical or radiological evidence of recurrence at 4 year fol-low-up.
Conclusion:Leiomyomas in the upper cervical spine is extremely rare in adolescent immunocom-petent male.
Keywords:Leiomyoma, spine, cervical.
Leiomyomas are benign tumors of smooth muscle. The distribution of such tumor’s mirrors the dis-tribution of smooth muscle tissue in the body. Therefore, these are more common in the genitouri-nary and gastrointestinal tracts. They are less frequent in the skin and rare in the deep soft tissues. Several types of leiomyomas have been described for classification purposes.
These include- cutaneous leiomyoma (leiomyoma cutis), angiomyomas (vascular leiomyoma), leiomyomas of deep soft tissue origin, leiomyomatosis peritonealis disseminata (represents a diffuse metaplastic response of the peritoneal surfaces), and finally benign genital stromal tumor’s.
The type which is relevant to this discussion is the leiomyomas of deep soft tissue origin which is the rarest form of leiomyoma [1]. Histologically, these tumor’s show fascicles of well-differentiated, uniform, elongated spindle-shaped cells with abundant eosinophilic cytoplasm which resemble smooth muscle cells. They show no necrosis, at most only mild atypia and <1 mitoses/50 high-power fields (HPF) [1, 2, 3]. As such, leiomyomas in the spine are extremely rare with only a limited number of studies describing them in English literature. Out of these nine were cases of Benign metastasizing leiomyoma (BML) [4, 5, 6, 7, 8, 9, 10, 11], and only 2 were Primary leiomyomas of the Spine [3, 12]. The tumor’s show strong reactivity to smooth muscle markers such as caldesmon, smooth muscle actin (SMA), and desmin with very low Ki-67 proliferative index (<2%) [2, 3, 5, 8].
A 15-year-old student had swelling over the nape of the neck for 4 years with slight difficulty in neck movements for 6 months (Fig. 1).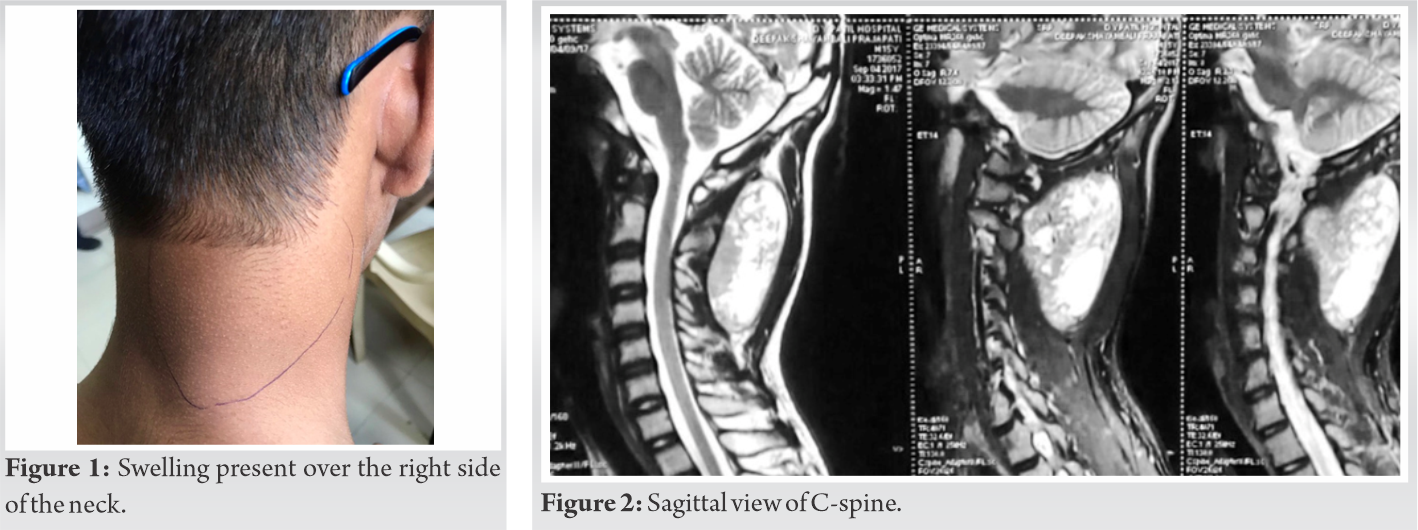

Primary leiomyomas of deep soft tissue origin is exceedingly rare as compared to their malignant counterpart. These are of two distinct types somatic and gynecologic, which differ in their presentation [1]. The less common somatic leiomyoma affects both sexes equally [1]. They measure several centimeters at presentation and about one-third also contain calcification. In contrast, the leiomyoma of gynecologic type occurs exclusively in women, usually in the peri-menopausal period. They closely resemble the standard uterine leiomyomas on gross and histo-pathological evaluation. This type typically displays both nuclear estrogen and progesterone receptor proteins [1].
Primary leiomyomas of the head and neck region are rare due to the paucity of smooth muscle in this region [2, 14, 15]. Leiomyomas have been described at locations like the oral cavity, nasal cavi-ty, nasopharynx, larynx, esophagus, and orbits [14, 15, 16]. Majority of the primary leiomyomas of the neck arise from the esophagus [2]. Leiomyomas of intra-spinal origin are extremely rare with two previous case reports describing leiomyomas arising from the thoracic spine [3, 12]; whereas, there is only one report of leiomyoma arising from the cervical spine. We believe that ours is an extremely rare case of a primary neck leiomyoma not arising from the esophagus with only two such cases described in literature [2, 14].
The pathogenesis of such tumors is uncertain. According to a theory put forward by Steel et al. such tumors arise from the smooth muscle component of blood vessels [12]. More modern studies postu-late the possible role of aberrant undifferentiated mesenchyme within the blood vessels [2, 14, 15]. In addition, association of concomitant viral infections such as Epstein-Barr virus [3, 17, 18, 19] and human immunodeficiency virus with smooth muscle tumors is well known [12, 20, 21, 22, 23]. Our case was again unique in this respect with the patient being immuno-competent.
The clinical presentation is characterized by the location of the tumor which secondary to its mass effect may present as a progressive swelling with secondary restriction in neck movements, difficul-ty feeding or breathing with associated malnourishment [2]. Intraspinal tumors may result in radicu-lopathy, spasticity as well as motor and sensory neurodeficit [3, 12]. In our case, the features gradu-ally worsened over a period of 4 years which is in accordance with other studies [3, 6, 9, 11, 12].
On histopathological evaluation the tumor comprises multiple interlacing fascicles or bundles of well-differentiated spindle-shaped acidophilic/eosinophilic cells which have blunt-ended, elongated nuclei also called as cigar-shaped nuclei. [2, 3, 12]. Somatic leiomyomas show no necrosis, only mild atypia if at all and virtually no mitotic activity with <1 mitosis/50 HPF [1]. Typically, IHC is assertive in ruling out other differential diagnoses with the tumor cells showing strong reactivity to smooth muscle markers such as SMA, desmin, and caldesmon. The Ki-67 proliferative index is also <2%. [2, 3, 5, 8]. Soft tissue leiomyomas of gynecologic type, either primary or BML may exhibit positivity for estrogen and progesterone receptors, unlike the somatic variety. [1, 11] Gross total excision of the tumor with intact capsule usually gives excellent results [3, 24]. Careful protection of adjacent vital structures is necessary to prevent inadvertent injury. Usually, it is not difficult to carefully delineate the mass from the surrounding tissues [3, 14]. There is one report of tumor recurrence in a young female following subtotal resection which necessitated repeat surgery [2]. In general, the post-operative outcomes after total resection are good although hormonal therapy may play a role in preventing recurrences in leiomyomas of gynecologic type [3].
Leiomyomas in the upper cervical spine are extremely rare in adolescent immunocompetent male.
Soft tissue swelling in adolescent male around craniovertebral junction should be extensively inves-tigated before planning optimum management.
References
- 1.Goldum JR, Folpe AL, Weiss SW. Enzinger and Weiss’s Soft Tissue Tumours. 6th ed. Amsterdam, Netherlands: Elsevier Publications; 2014. [Google Scholar]
- 2.Al-Habib A, Elgamal EA, Aldhahri S, Alokaili R, AlShamrani R, Abobotain A, et al. Large primary leiomyoma causing progressive cervical deformity. J Surg Case Rep 2016;2016:rjw190. [Google Scholar]
- 3.Yang T, Wu L, Deng X, Yang C, Zhao L, Xu Y. Intraspinal leiomyoma: A case report and literature review. Oncol Lett 2014;8:1380-4. [Google Scholar]
- 4.Gatti JM, Morvan G, Henin D, Aboulker J, Nahum H, Glowinski J. Leiomyomatosis metastasizing to the spine. A case report. J Bone Joint Surg Am 1983;65:1163‐5. [Google Scholar]
- 5.Hekster RE, Lambooy N, van Hall EV, Kazzaz BA, van Rijssel EJ. Hormone-dependent spinal leiomyoma. Surg Neurol 1994;41:330‐3. [Google Scholar]
- 6.Alessi G, Lemmerling M, Vereecken L, De Waele L. Benign metastasizing leiomyoma to skull base and spine: A report of two cases. Clin Neurol Neurosurg 2003;105:170‐4. [Google Scholar]
- 7.Choi S, Levy ML, Krieger MD, McComb JG. Spinal extradural leiomyoma in a pediatric patient with acquired immunodeficiency syndrome: Case report. Neurosurgery 1997;40:1080‐2. [Google Scholar]
- 8.Jayakody S, Young K, Young B, Ferch R. Serial spread of benign metastasizing leiomy-oma to the thoracic spine. J Clin Neurosci 2011;18:1135‐7. [Google Scholar]
- 9.Joseph V, Chacko G, Raghuram L, Rajshekhar V. Benign metastasizing leiomyoma causing spinal cord compression. Surg Neurol 2003;60:575‐8. [Google Scholar]
- 10.Vicente LF, Maia AP, Carvalho MJ, Sá e Melo P, Magalhães C, Torrezão I, et al. A benign leiomyoma causing paraparesis: A case report and histopathogenesis. Acta Obstet Gynecol Scand 2005;84:704‐6. [Google Scholar]
- 11.Iwakura R, Tachibana T, Maruo K, Arizumi F, Kusuyama K, Kishima K, et al. Benign metastasizing leiomyoma mimicking dumbbell tumor of the spine: A report of two cases. Interdiscip Neurosurg 2016;7:71-2. [Google Scholar]
- 12.Steel TR, Pell MF, Turner JJ, Lim GH. Spinal epidural leiomyoma occurring in an HIV-infected man. Case report. J Neurosurg 1993;79:442‐5. [Google Scholar]
- 13.Billings SD, Folpe AL, Weiss SW. Do leiomyomas of deep soft tissue exist? An analysis of highly differentiated smooth muscle tumors of deep soft tissue supporting two dis-tinct subtypes. Am J Surg Pathol 2001;25:1134-42. [Google Scholar]
- 14.Yamanishi T, Sakamoto K, Watanabe H, Yonaga T, Oishi N, Katoh R, et al. Primary cervical leiomyoma with remarkable calcification and ossification. Case Rep Otolaryngol 2014;2014:896275. [Google Scholar]
- 15.Veeresh M, Sudhakara M, Girish G, Naik C. Leiomyoma: A rare tumor in the head and neck and oral cavity: Report of 3 cases with review. J Oral Maxillofac Pathol 2013;17:281-7. [Google Scholar]
- 16.Purohit GN, Agarwal N, Agarwal R. Leiomyoma arising from septum of nose. Indian J Otolaryngol Head Neck Surg 2011;63:64-7. [Google Scholar]
- 17.Lee ES, Locker J, Nalesnik M, Reyes J, Jaffe R, Alashari M, et al. The association of Epstein-Barr virus with smooth muscle tumors occurring after organ transplantation. N Engl J Med 1995;332:19-25. [Google Scholar]
- 18.McClain KL, Leach CT, Jenson HB, Joshi VV, Pollock BH, Parmley RT, et al. Associa-tion of Epstein-Barr virus with leiomyosarcomas in young people with AIDS. N Engl J Med 1995;332:12-8. [Google Scholar]
- 19.Zevgaridis D, Tsonidis C, Kapranos N, Venizelos I, Tsitsopoulos P, Tsitsopoulos P. Ep-stein-Barr virus associated primary intracranial leiomyoma in organ transplant recipient: Case report and review of the literature. Acta Neurochir (Wien) 2009;151:1705-9. [Google Scholar]
- 20.Chadwick EG, Connor EJ, Hanson CG, Joshi VV, Abu-Farsakh H, Yogev R, et al. Tu-mors of smooth-muscle origin in HIV-infected children. JAMA 1990;263:3182-4. [Google Scholar]
- 21.McLoughlin LC. Nord KS, Joshi VV, DiCarlo FJ, Kane MJ. Disseminated leiomyosar-coma in a child with acquired immune deficiency syndrome. Cancer 1991;67:2618-21. [Google Scholar]
- 22.RossJS, Del Rosario A, Bui HX, Sonbati H, Solis O. Primary hepatic leiomyosarcoma in a child with the acquired immunodeficiency syndrome. Ham Pathol 1992;23:69-72. [Google Scholar]
- 23.Starasoler L, Vuitch F, Albores-Saavedra J. Intranodal leiomyoma: Another distinctive primary spindle cell neo-plasm of lymph node. Am J Clin Pathol 1991;95:858-62. [Google Scholar]
- 24.Hua W, Xu F, Mao Y, Zhang J, Wang Y, Mao R, et al. Primary intracranial leiomyomas: Report of two cases and review of the literature. Clin Neurol Neurosurg 2009;11:907-12. [Google Scholar]





