When we perform revision anterior cruciate ligament reconstruction with BTB, we should consider that the patient may have collateral circulation in the lower leg.
Dr. Akira Maeyama, Department of Orthopaedic Surgery, Fukuoka University Faculty of Medicine, 7-45-1 Nanakuma, Jonan-ku, Fukuoka 810-0180, Japan. E-mail: akira.maeyama0713@joy.ocn.ne.jp
Introduction:Acute compartment syndrome (ACS) is one of the most serious orthopedic diseases causing complications and requiring emergency surgery. Most cases of ACS are associated with fractures and crush injuries. However, surgical procedures can also cause ACS.
Case presentation:We herein describe a 41-year-old man who underwent arthroscopic surgery for revision anterior cruciate ligament reconstruction with the semitendinosus tendon. Two days after the operation, the patient developed ACS of the left lower leg. This patient had undergone anterior cruciate ligament(ACL) reconstruction previously, and we assumed that the cause of the ACS was damage to the small blood vessels from the collateral circulation during hamstring tendon harvesting. Fasciotomy was performed under general anesthesia, and his postoperative course was uneventful.
Conclusion:ACS after revision anterior cruciate ligament reconstruction is rare. We should keep in mind that patients who have undergone previous surgery may develop ACS due to damage to the collateral circulation. To avoid ACS, harvesting tendon from the healthy side can avoid damage to the collateral circulation.
Keywords:Acute compartment syndrome, Anterior cruciate ligament reconstruction, Fasciotomy
One of the most devastating complications of orthopedic surgery is acute compartment syndrome (ACS), which is caused by bleeding or edema within a closed, nonelastic muscle compartment. ACS impairs tissue perfusion and jeopardizes the viability of the muscles, nerves, tendons, and vessels. Early diagnosis and fasciotomy are important to prevent permanent damage to the muscle and neurovascular structures [1]. The most common cause of ACS is trauma; however, some reports have also described ACS after orthopedic surgery, such as total hip and knee arthroplasty [2]. Arthroscopic anterior cruciate ligament (ACL) reconstruction for ACL rupture is a well-established operation with a high success rate. However, reported complications of ACL reconstruction include infection, complex regional pain syndrome, synovitis, and hematoma formation [3]. ACS after ACL reconstruction is a rare complication that has been reported very infrequently [4]. We present a case of ACS after revision ACL reconstruction.
This case involved a 41-year-old man for whom we performed left-side revision ACL reconstruction 3 weeks after injury using the semitendinosus tendon (tourniquet pressure, 280 mmHg; duration of tourniquet use, 55 minutes). Since we use tourniquet during the operation, no obvious arterial bleeding was observed in the surgical field. Approximately 20 years previously, the patient had undergone left ACL reconstruction with a patellar tendon graft. On the second postoperative day following revision, his lower leg became swollen and painful. Deep vein thrombosis was suspected, and the patient was transferred to a general hospital where he could be examined. Although computed tomography (CT) showed no thrombus in his lower leg, a hematoma was found in the gastrocnemius muscle. Postoperative ACS was suspected, and the patient was transferred to our critical care medical center. Upon arrival at our hospital, the patient’s lower leg was swollen, he exhibited poor toe movement, and the dorsal foot artery was not palpable. Although CT showed that blood circulation in the lower leg was maintained, a hematoma was found in the gastrocnemius muscle (Fig. 1). The anterior compartment pressure was elevated at 48 mmHg, and posterior compartment pressure was 50 mmHg. 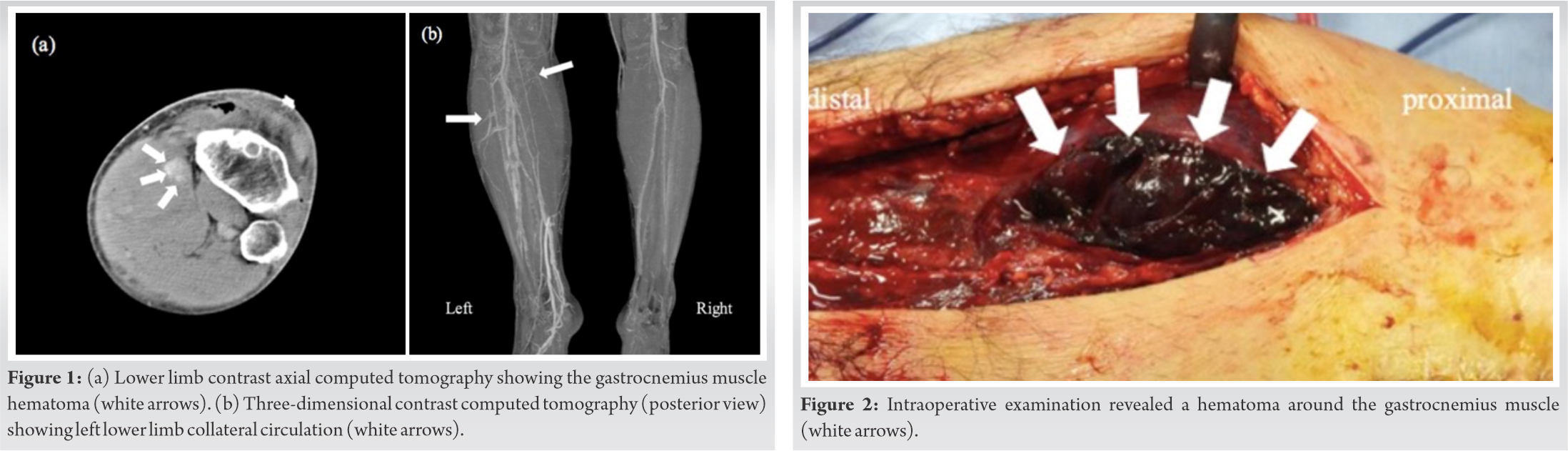
ACS is a disorder characterized by increased intracompartmental pressure that compromises the circulation and causes nerve and muscle damage, resulting in adverse effects on limb function [5]. ACS commonly occurs in the lower leg but can also occur in the upper limb or thigh [6]. Most cases of ACS are caused by bone fracture and crush-type injury [7]; however, long surgery time (> 4 hours), long duration of tourniquet use [8, 9, 10], high-pressure tourniquet use, specific operating positions, obesity, and the use of elastic stockings [11] have been reported as other causes of ACS. The clinical symptoms are well known as the 6 “Ps” (pain, pain on passive stretching of the involved muscles, paresthesia, pulselessness, and paralysis); however, the presence of these signs may indicate necrosis of the muscles and an irreversible clinical stage. Notably, arterial ischemia is more often associated with these signs than is ACS. Therefore, it is important to monitor the compartment pressure to ensure early diagnosis of ACS. Allen et al. [12] reported that fasciotomy should be performed when the pressure is > 50 mmHg or > 40 mmHg for > 6 hours. Masten et al. [13] reported that the indication for fasciotomy is a pressure of > 55 mmHg, and compartmental syndrome lasting > 12 hours is likely to result in chronic functional deficits. In the present case, the posterior compartment pressure was 50 mmHg, and the anterior pressure was 40 mmHg. Fasciotomy was performed approximately 12 hours after onset, and no complications occurred. Because distal leg venous thrombosis was suspected perioperatively, the patient was transferred to a general hospital, which might have caused delayed examination and delayed fasciotomy. However, because ACS results in irreversible symptoms, early fasciotomy and early diagnosis are very important. Some reports have indicated that nerve block after orthopedic surgery might mask signs of compartment syndrome; therefore, clinicians must be especially careful in such cases [14]. In our patient, a large hematoma was found around the gastrocnemius muscle, and arterial bleeding was observed from a bundle of blood vessels at the hamstring stump. Blood vessel injury is a rare complication of ACL reconstruction. Milankov et al. [15] reported a case of pseudoaneurysm of the medial inferior genicular artery following ACL reconstruction. The authors reported that one reason for a pseudoaneurysm of the inferior medial geniculate artery may be hamstring tendon harvesting. In the present case, contrast CT showed no obvious contrast media extravasation; however, bleeding was observed from a bundle of blood vessels at the hamstring stump during the second hematoma removal. The patient had undergone ACL reconstruction approximately 20 years previously, and lower leg contrast CT showed collateral circulation (Fig. 2). We hypothesized that the cause of the ACS in our patient was damage to small blood vessels from the collateral circulation during hamstring tendon harvesting. Because we haven’t deflated tourniquet before skin closure, we haven’t be able to confirm the presence of bleeding. If we have deflated tourniquet before skin closure over pes anserinus, we might be able to confirm the presence of bleeding. If a patient undergoing a lower limb operation has a history of an operation at the same site, the orthopedic surgeon should consider that the patient may have collateral circulation in the lower leg because the collateral circulation might be damaged. The first surgery in our patient was performed at another hospital using bone–tendon–bone (BTB) grafting. We usually perform ACL reconstruction using hamstring tendon harvesting and revision ACL reconstruction using BTB. If the first surgery is performed using BTB, there may be collaterals with adhesions around the knee. In such cases, we consider that preoperative CT or doppler are useful. Therefore, we should consider the graft choice in the initial surgery. If a patient has collateral circulation in the lower leg, we can lower the risk of blood vessel injury using a healthy side patellar tendon graft or hamstring tendon graft.
ACS after revision ACL reconstruction is rare. Two days after the operation, our patient developed ACS of the left lower leg, and contrast CT showed collateral circulation in the lower leg. The cause of the ACS was damage to small blood vessels from the collateral circulation during hamstring tendon harvesting. Fasciotomy was performed, and the postoperative course was uneventful. If a patient undergoing a lower limb operation has a history of an operation at the same site, the orthopedic surgeon should consider that the patient may have collateral circulation in the lower leg.
When we perform revision anterior cruciate ligament reconstruction with BTB, we should consider that the patient may have collateral circulation in the lower leg. Using healthy patellar tendon or hamstring tendon can avoid damage to small blood vessels from the collateral circulation during hamstring tendon harvesting.
References
- 1.Gamer MR, Taylor SA, Gausden E, Lyden JP. Compartment syndrome diagnosis, management, and unique concerns in the twenty-first century. HSS J 2014;10:143-52. [Google Scholar]
- 2.Hogerzeil DP, Muradin I, Zwitser EW, Jansen JA. Acute compartment syndrome of the thigh following hip replacement by anterior approach in a patient using oral anticoagulants. World J Orthop 2017;8:964-7. [Google Scholar]
- 3.Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg 2015;3:220-40. [Google Scholar]
- 4.Filho JS, Ramos LA, Sayum J, de Carvalho RT, Ejnisman B, Matsuda MM, Nicolini A, Cohen M. leg’s compartment syndrome after reconstruction of the anterior cruciate ligament: case report. Rev Bras Ortop 2015;46:730-2. [Google Scholar]
- 5.Pechar J, Lyons MM. Acute compartment syndrome of the lower leg: a review. J Nurse Pract 2016;12:265-70. [Google Scholar]
- 6.Schmidt AH. Acute compartment syndrome. Injury 2017;48(Suppl 1):S22-5. [Google Scholar]
- 7.McQueen MM, Gaston P, Court-Brown CM. Acute compartment syndrome. Who is at risk? J Bone Joint Surg Br 2000;82:200-3. [Google Scholar]
- 8.Klenerman L, Biswas M, Hulands GH, Rhodes AM. Systemic and local effects of the application of tourniquet. J Bone Joint Surg [Br] 1980;62:385-8. [Google Scholar]
- 9.Kort NP, van Raay JJ, van Hom JR. Compartment syndrome and popliteal vascular injury complicating unicompartmental knee arthroplasty. J Arthroplasty 2007;22:472-6. [Google Scholar]
- 10.Hirvensalo E, Tuominen H, Lapinsuo M, Helio H. Compartment syndrome of the lower limb caused by a tourniquet. A report of two cases. J Orthop Trauma 1992;6:469-72. [Google Scholar]
- 11.Raza A, Byrne D, Townell N. Lower limb compartment syndrome after urological pelvic surgery. J Urol 2004;171:5-11. [Google Scholar]
- 12.Allen MJ, Stirling AJ, Crawshaw CV, Barnes MR. Intracompartmental pressure monitoring of leg injuries. An aid to management. J Bone Joint Surg [Br] 1985;67:53-7. [Google Scholar]
- 13.Masten FA 3rd. Compartmental syndrome. An unified concept. Clin Orthop Relat Res 1975;113:8-14. [Google Scholar]
- 14.Park CH, Lee SH, Kang DG, Cho KY, Lee SH, Kim KI. Compartment syndrome following total knee arthroplasty: clinical results of late fasciotomy. Knee Surg Relat Res 2014;26:177-81. [Google Scholar]
- 15.Milankov M, Miljkovic N, Stankovic M. Pseudoaneurysm of the medial inferior genicular artery following anterior cruciate ligament reconstruction with hamstring tendon autograft. Knee 2006;13:170-1. [Google Scholar]









