Tuberculosis of the shoulder has variable presentation, early diagnosis and treatment with anti-tubercular therapy is instrumental in prevention of severe joint damage.
Dr. Shrihari L Kulkarni, Department of Orthopaedics, SDM College of Medical Sciences and Hospital, Shri Dharmasthala Manjunatheshwara University, Dharwad - 580 009, Karnataka, India. E-mail: shrihari1711@gmail.com
Introduction:Tuberculosis (TB) involving the shoulder joint is rare. Early diagnosis is difficult but essential to prevent severe joint damage. In this report, we present variable presentation and management of TB of shoulder joint in three patients.
Case Report:This report includes three patients. First patient was a 58-year-old male with severe muscle wasting around the shoulder with restriction of all movements had dry form of TB. Second patient was 55-year-old female with pain and swelling in the shoulder had wet form of TB with submuscular bursitis with rice bodies. A 50-year-old female presented with pain in the right shoulder with restricted active movements only was diagnosed with mobile form of TB was our third patient. Shoulder TB was diagnosed on the basis of histopathological examination in all three patients and was treated with 12 months of anti-tubercular therapy (ATT). All patients had good recovery and were back to their routine activities.
Conclusion:TB of the shoulder has variable presentation; histopathological examination is the gold standard for diagnosis. Early diagnosis and treatment with ATT help in prevention of the severe joint damage.
Keywords:Skeletal tuberculosis, shoulder joint, histopathology, anti-tubercular therapy.
Tuberculous bacilli have been infecting the humans since the days beyond recall. Extra-pulmonary tuberculosis (TB) accounts for about 15–18% of newly detected TB cases, spine being the most common site for musculoskeletal TB which is involved in more than half of the cases involving musculoskeletal system. Shoulder involvement is very uncommon, and its incidence is estimated to be about 1–2% [1]. Shoulder TB is hardly considered as a differential diagnosis as the clinical presentation is indolent and non-specific. Even the radiographic features are not remarkable; hence, the diagnosis is often delayed. Early diagnosis and initiation of the treatment are pivotal in prevention of severe joint damage [2]. In this report, we present three patients with shoulder TB with emphasis on the difference in the clinical and radiological presentation.
Case 1 (Caries Sicca)
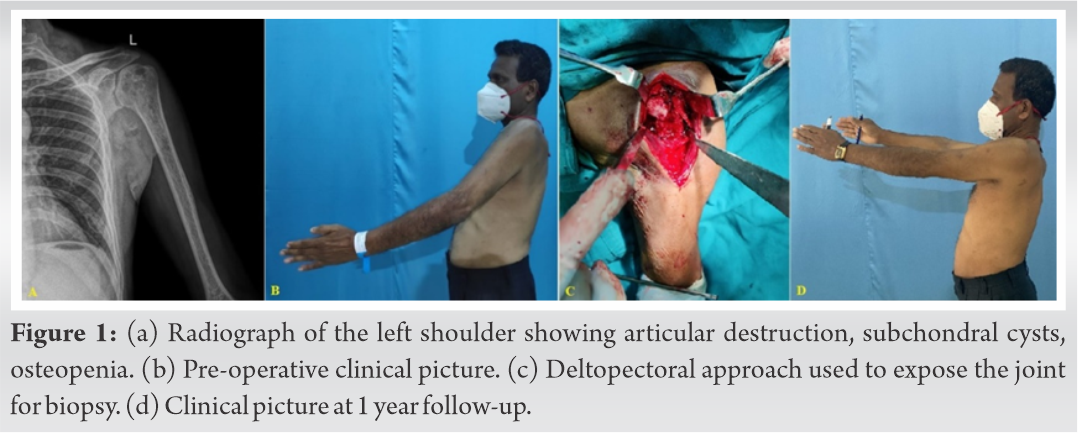
A gentleman aged 58 years presented with pain and stiffness in left shoulder for 12 months and increased for 3 months. Shoulder was tender on palpation, severe wasting of muscles around the shoulder girdle was noted with painful global restriction of movements. Axillary and deep pectoral lymph nodes were enlarged (three in number, largest measuring about 1.5 cm, firm, mobile, and non-tender). There were no signs of acute inflammation in the shoulder. Total white blood cells count was 12770 cells/mm3 and erythrocyte sedimentation rate was 50 mm/h. Radiographs of the left shoulder revealed focal lytic lesions in head of the humerus with reduced joint space, subchondral cysts, and articular irregularity. After procuring informed consent, arthrotomy of the left shoulder was performed using deltopectoral approach. Intraoperatively capsule was thickened, minimal purulent thick discharge was present in the joint and patchy destruction of cartilage over the head of the humerus was noted. Histopathological analysis of the capsule and synovial tissue revealed features suggestive of tubercular infection of the shoulder joint. Anti-tubercular therapy (ATT) was started and patient was followed up regularly. After 1 year of ATT, patient was pain-free and had regained good range of movements in his left shoulder (Fig. 1).
Case 2 (Caries Exudata)
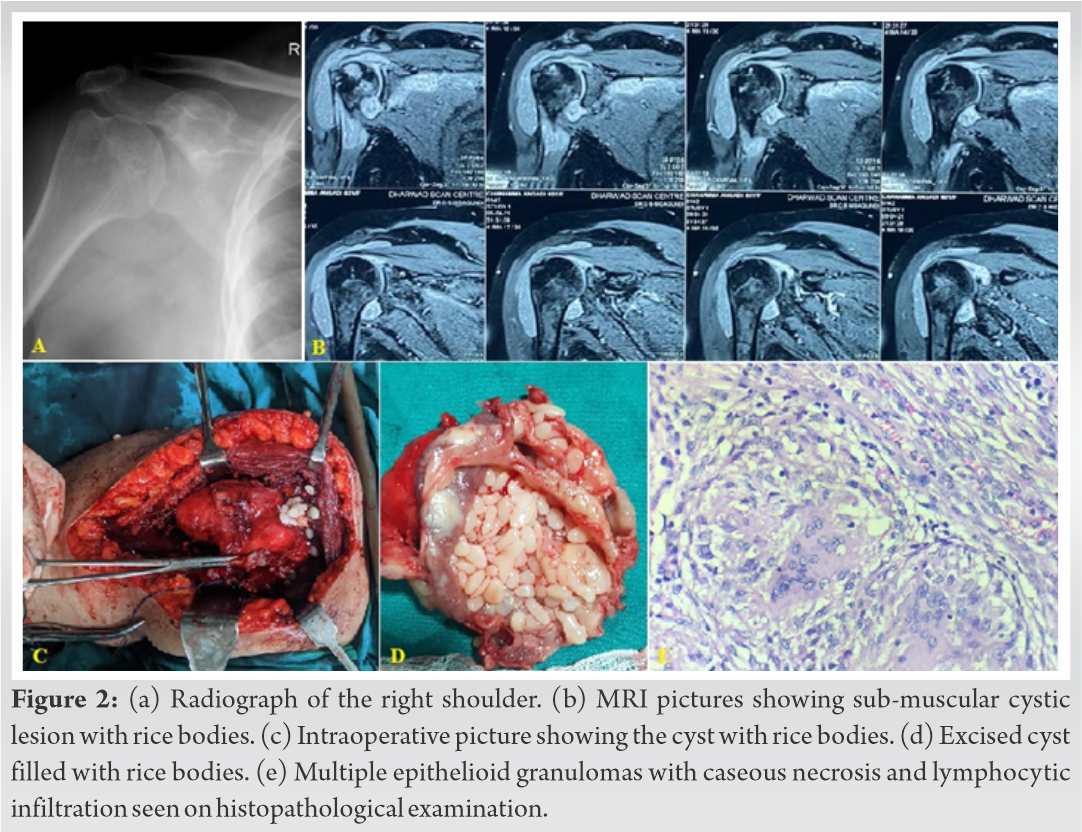
A 55-year-old lady, presented to us with complaints of pain in the right shoulder for 2 years which had aggravated in the past 7 months. Patient had history of on and off fever. Pain was associated with swelling in the anterior aspect of the shoulder, which was oval shape, about 5 × 6 cm and soft in consistency. Shoulder was tender and the movements were restricted and painful (rotations were maximum affected). The total white blood cells count was 12970 cells/mm3 and ESR was 80mm/hr. Radiographs showed no abnormality, MRI revealed heterogenous effusion with thickened synovium with internal heterogenous contents with erosions over the head of the humerus and glenoid cavity with collection extending along the submuscular plane of the subscapularis muscle. Patient was taken up for excision of the lesion after taking informed consent. With patient in supine position shoulder was exposed by the deltopectoral approach. Intraoperatively a soft globular swelling (bursal cyst) measuring 7 × 6.5 × 2 cm covered by fibrous adhesions on its surface with lumen filled of rice bodies was noted. Histopathological examination showed bursal cyst lined by thick layer of fibrin overlying multiple epithelioid granulomas with caseous necrosis and lymphocytic infiltration. Rice bodies were composed of homogenous pink fibrinous material. All features were suggestive of tubercular bursitis of the right shoulder. Patient was started on ATT and was followed up regularly. ATT was given for 1 year without any complications. At 1 year follow-up patient was comfortable with full range of movements at the right shoulder (Fig. 2).
Case 3 (Caries Mobile)
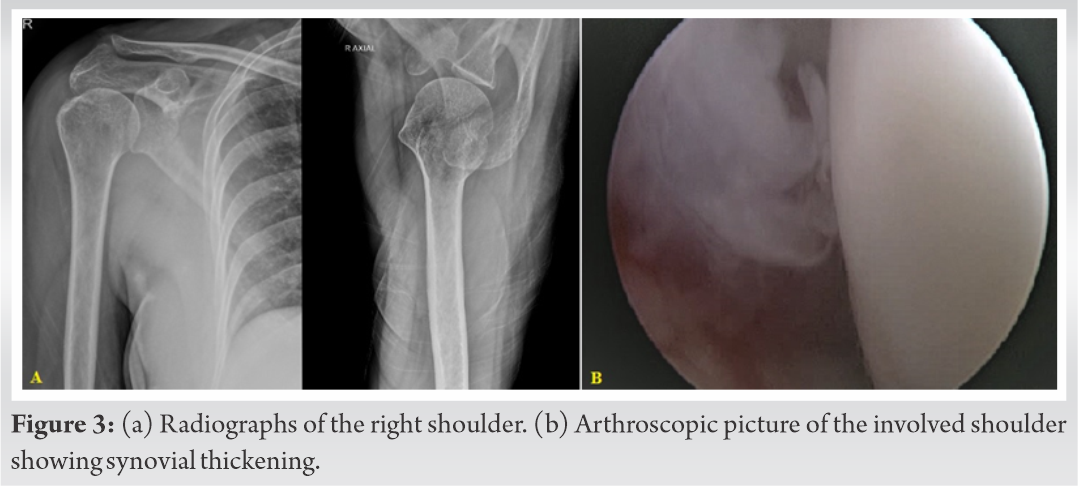
A 50-year-old female presented to us with dull aching pain in the right shoulder for more than a year and which had increased in the past 4 months. She had difficulty in carrying out her daily activities especially those requiring overhead abduction. Patient had suffered from pulmonary TB 12 years ago for which she had taken ATT for 6 months, along with well controlled diabetes mellitus, hypertension, and hypothyroid. Right shoulder was tender on palpation, the active movements (mainly abduction) were restricted and painful and passive movements were within full range. The total white blood cells count was 6900 cells/mm3 and ESR was 28 mm/h. Radiographs showed no abnormality and MRI showed moderate degree of synovial effusion in the glenohumeral joint. After obtaining informed consent, diagnostic arthroscopy, debridement, and biopsy were performed. Histopathology revealed multiple epithelioid granulomas with surrounding caseous necrosis. The patient was started on ATT and followed up regularly. At 1 year follow-up patient was able to perform her daily routine and had full range of active movements in the shoulder (Fig. 3).
Shoulder TB is a rare condition. Usually, the infection spreads via the hematogenous route or by the direct spread from the adjacent bone. TB of the shoulder is classified into three types depending on the clinical presentation: Caries Sicca, Caries Exudata, and Caries Mobile (Table 2). Caries Sicca or the classical dry form of shoulder TB is the most common presentation. Caries Exudata or the fulminating type and Caries Mobile are rare in adults [3]. Caries Exudata can present as subdeltoid bursitis with formation of rice bodies. Aggregation of the fibronectin/fibrin in the synovial fluid and microinfarction of the synovium leading to sloughing of the infarcted tissue are the proposed theories in the pathogenesis of the rice bodies [4]. Pain, stiffness (especially external rotation and over-head abduction), supraspinatus, and deltoid wasting are the most common presenting features in TB of the shoulder. Fever, weight loss, loss of appetite, and lymphadenopathy are uncommon systemic symptoms, as is swelling of the joint. Due to the overlap of these features with many other shoulder pathologies, it is very difficult to diagnose this condition in its early stages. Richter et al. established the average delay in diagnosis to be 15 months and Kapukaya et al. found an average delay of about 5.2 months in the onset of symptoms and diagnosis of TB of the shoulder [5, 6].
Elevated ESR is observed in most of the patients with skeletal TB but this finding is neither specific nor reliable. The radiological findings are classified into four stages by Martini et al. but there is no feature which is pathognomonic for skeletal TB (Table 3). Severe periarticular osteoporosis, bony erosions, and joint space narrowing (Phemister’s triad) are important findings on radiographs. MRI is helpful in early diagnosis as it demonstrates lesion before they appear on radiographs; additionally, it is also helpful in evaluation of the extent of the lesion. Effusion, peri-articular osteoporosis, lytic bone lesions, sclerosis, and thickening of the synovium are some of the features of TB seen on MRI. Most important disadvantage of MRI is, it fails to differentiate between tubercular osteomyelitis and chronic pyogenic osteomyelitis. Skeletal TB is usually paucibacillary; hence, it is difficult to demonstrate bacilli on microscopy. Histopathological examination of the pathological tissue is confirmatory for skeletal TB. Multiple granulomas with caesious necrosis are pathognomonic of the tubercular infection. In endemic regions skeletal TB can be diagnosed on the basis of clinical presentation, classical radiological features and raised ESR [6, 7, 8, 9]. Shoulder arthroscopy plays important role in diagnosis as it allows adequate joint visualization and also permits excision of the synovial tissue, rice bodies and pannus for biopsy. Arthroscopic biopsy is useful only in early stages of the disease. However, in advanced disease, an open debridement and biopsy is indicated. Minimum 12 months of ATT is necessary for the management of shoulder TB; in some cases, it can be can be extended to 18 months (2HRZE/10-16HRE) along with rest in arm pouch or brace and mobilization as tolerated. Surgical management is rarely required. Large abscess, persistent sinus, loose bodies in the joint and pannus over cartilage are some of the indications for surgery [10, 11]. In this study, we have described three patients with each type of clinical presentation. Two patients (Cases 1 and 2) with advanced disease underwent open biopsy and debridement. Arthroscopic debridement was performed for the third patient. Diagnosis was confirmed by histopathology in all patients. All patients took ATT for 1 year as per guidelines for the management of extra-pulmonary TB for Indian population and had good clinical and functional recovery.
TB of the shoulder is a rare condition and is infrequently diagnosed in its early stages due to non-specific clinical and radiological features. One has to be aware of its variable presentation. Early diagnosis and management of the condition is pivotal for prevention of the severe joint damage. Histopathological diagnosis is the gold standard, patients recover well with the ATT for 12 months and very rarely patients require surgical management.
Non-specific and variable presentation makes it difficult to diagnose the TB of shoulder in its early stages. High index of suspicion and knowledge of variable presentation is important in early diagnosis and treatment of this condition to prevent permanent joint damage.
References
- 1.Tuli SM. Tuberculosis of the Skeletal System. 4th ed. New Delhi: Jaypee Brothers Medical Publisher (P) Ltd.; 2010. p. 140-8. [Google Scholar]
- 2.Longo UG, Marinozzi A, Cazzato L, Rabitti C, Maffulli N, Denaro V. Tuberculosis of the shoulder. J Shoulder Elbow Surg 2011;20:e19-21. [Google Scholar]
- 3.Patel PR, Patel DA, Thakker T, Shah K, Shah VB. Tuberculosis of shoulder joint. Indian J Orthop 2003;37:7. [Google Scholar]
- 4.Pimprikar MV, Kekatpure AL. Subdeltoid bursa tuberculosis with rice bodies formation: Case report and review of literature. J Orthop Case Rep 2014;4:57-9. [Google Scholar]
- 5.Richter R, Hahn H, Nübling W, Köhler G. Die schultergürtel und schultergelenktuberkulose [Shoulder girdle and shoulder joint tuberculosis]. Z Rheumatol 1985;44:87-92. [Google Scholar]
- 6.Kapukaya A, Subasi M, Bukte Y, Gur A, Tuzuner T, Kilnc N. Tuberculosis of the shoulder joint. Joint Bone Spine 2006;73:177-81. [Google Scholar]
- 7.Kumar K, Panchal S, Sabarinathan N, Prabhakar A. Rare presentation of caries exudata with dumbbell shaped abscess in an adult a case report. J Orthop Case Rep 2021;11:23-7. [Google Scholar]
- 8.Watts HG, Lifeso RM. Tuberculosis of bones and joints: Current concepts review. J Bone Joint Surg 1996;78:288-98. [Google Scholar]
- 9.Martini M, Benkeddache Y, Medjani Y, Gottesman H. Tuberculosis of the upper limb joints. Int Orthop 1986;10:17-23. [Google Scholar]
- 10.Sharma SK, Ryan H, Khaparde S, Sachdeva KS, Singh AD, Mohan A, et al. Index-TB guidelines: Guidelines on extrapulmonary tuberculosis for India. Indian J Med Res 2017;145:448-63. [Google Scholar]
- 11.World Health Organization. Index TB Guidelines. Guidelines on Extra-pulmonary Tuberculosis for India. Geneva: World Health Organization; 2016. Available from: https://tbcindia.gov.in/ WriteReadData/ l892s/ 5585665076Index-TB%20Guidelines.pdf [Last accessed on 2021 Oct 04]. [Google Scholar]