Open VTB2W PPF around an Exeter stem can be internally fixed if the bone cement interface is intact and the fracture can be anatomically reducible, double plating provides more stability for early weight bearing mobilization.
Dr. Veenesh Selvaratnam, Department of Trauma and Orthopaedic Surgery, Exeter Hip Unit, Princess Elizabeth Orthopaedic Centre, Royal Devon and Exeter Hospital, Exeter, United Kingdom. E-mail: veenesh_selvaratnam@yahoo.co.uk
Introduction: The incidence of periprosthetic fracture (PPF) around a total hip arthroplasty (THA) continues to increase with the rise of number of THA performed. We present a rare case of a 73-year-old man who sustained an open periprosthetic femur fracture around a THA.
Case Report: This gentleman sustained an open PPF around a fully cemented THA after he lost control and fell off his bicycle. After thorough surgical debridement, internal fixation with double plating was performed and the fracture went on to unite with an excellent patient reported outcome score. To the best of our knowledge, this is the only reported open 3A VTB2W PPF THA in the literature.
Conclusion:Open PPF around a THA is a rare and uncommon occurrence. Principles of open fracture management should be continued and we recommend urgent surgery to reduce the risk of post-operative infection. Open VTB2W PPF should be fixed with double plating if the bone cement interface is intact and the fracture can be anatomically reduced. Double plating gives additional rotational stability and allows early weight bearing post-operatively.
Keywords:Periprosthetic hip fracture, open fracture, open periprosthetic hip fracture.
Since the first reported periprosthetic femur fracture around a total hip arthroplasty (THA) in 1954 [1], the prevalence of periprosthetic fracture (PPF) continues to rise with the increasing rate of THA worldwide [2]. These fractures can occur either around the acetabular component or significantly more frequently in the femoral component [3]. The incidence of PPF is reported between 0.07% and 18% after THA [4, 5, 6]. Historically, non-operative management such as traction has resulted in poor outcomes [7]. Operative management of PPF has been shown to result in early mobilization and reduced hospital stay. It also affords a reduction in systemic and local complications such as malunion and non-union [8].
The Vancouver classification by Duncan and Masri is the most commonly used PPF classification and it facilitates treatment decision [9, 10]. The majority of PPFs are located around the stem and classified as Vancouver type B (VTB) with either a well-fixed (VTB1) or loose stem (VTB2) with poor bone stock (VTB3). The treatment choice for VTB1 is open reduction internal fixation (ORIF), while the recommended management plan for a VTB2 is revision arthroplasty with a long stem bypassing the fracture site [11, 12, 13].
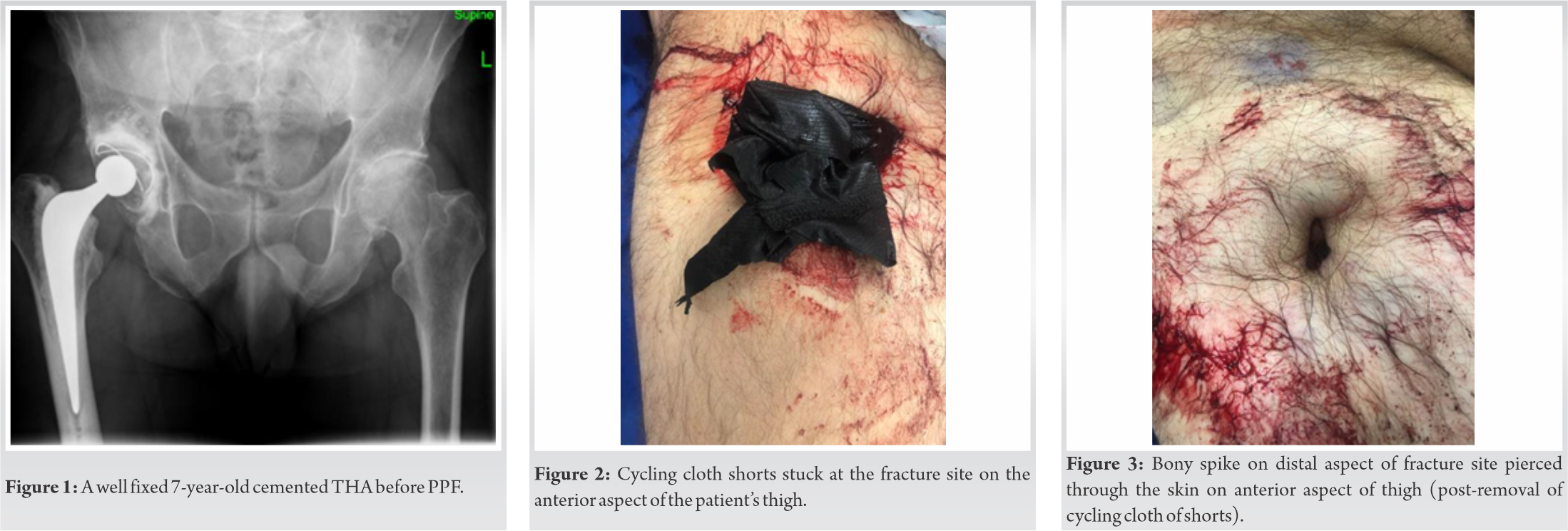
Although PPF is common, open PPF is extremely rare. We present a rare case of a 74-year-old gentleman who sustained a traumatic Gustillo-Anderson grade 3A VTB2W fracture which had an ORIF with a double plate with supplementary cable fixation. He had a fully cemented primary right THA in the Exeter Hip Unit, United Kingdom 7 years before his PPF for primary hip osteoarthritis (Fig. 1).
This was a 74-year-old gentleman who had a primary cemented Exeter V40 THA in 2013 for hip osteoarthritis. He was doing well until 7 years postoperatively when he lost control and fell off his bicycle at 18 miles/h.
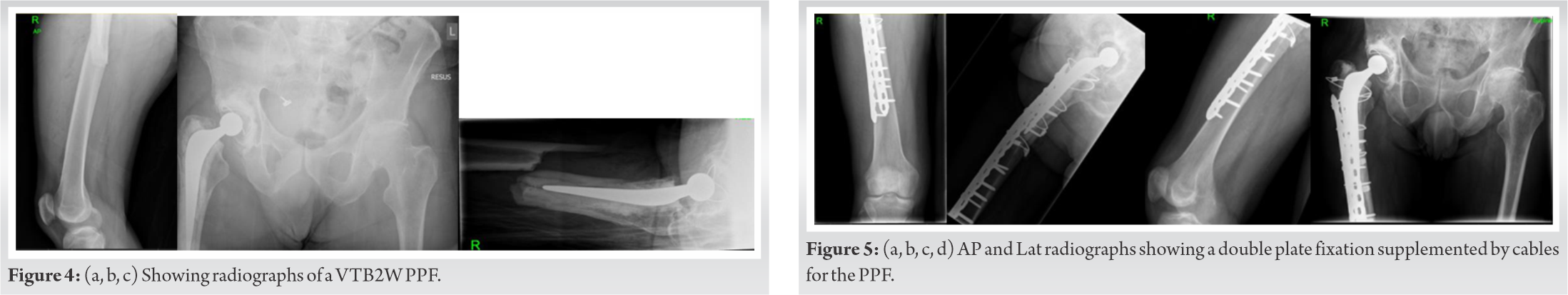
He sustained an open 3A comminuted right PPF with his clothing contaminating the fracture site (Fig. 2). The open wound was present on the anterior aspect of his thigh (Fig. 3). His PPF was classified as VTB2W with no evidence of loosening at the cement bone interface (Fig. 4).
He was assessed using ATLS principles on arrival to the Emergency Department. His open fracture was managed according to the BOA-BAPRAS guidelines [14]. He was taken to theatre expediently due to gross contamination of the wound and infection concerns with the in-dwelling metalwork of the THA. The surgery was performed in two stages with separate preparation, draping, and instrumentation for each stage. During the first stage, thorough debridement and washout of the wound, soft tissues, and fracture was undertaken in the supine position after extension of the open wound. The open fracture wound was primarily closed, after copious saline wash, with deep interrupted absorbable Vicryl sutures and interrupted non-absorbable nylon sutures to skin.
For the second stage of the procedure, the patient was repositioned in the lateral decubitus position and the leg was re-prepped and draped for surgery. A lateral incision was made incorporating the distal extend of the previous THA wound and extending down to the femur using a subvastus approach. The fracture site was re-exposed, debrided, and washed again with evidence of bleeding bone post-debridement. A decision was taken to retain all hip arthroplasty components due to no evidence of loosening or subsidence of components on pre-operative radiographs. The hip joint was not opened as the fracture did not appear to communicate with the joint on radiographs or direct inspection and it was felt that opening up the joint to washout would provide and unnecessary increased risk of post-operative dislocation.
The fracture was reduced and reduction held with Kinamed Iso-elastic polymer cerclage Supercables (Camarillo, CA, USA). The fracture was then further stabilized using double plating technique with both plates at 90° to each other to provide a biomechanically stable construct. A broad curved Depuy Synthes (MA, USA) LCP 4.5 mm stainless steel plate was placed laterally and a narrow Depuy Synthes LCP 4.5 mm plate anteriorly underneath quadriceps through the same lateral incision. Non-locking screws were used to compress the plate to bone followed by locking screws to minimize the risk of plate failure. Dall Miles 2 mm Cables (Stryker Ltd, Kalamazoo, In) were then placed around both plates to supplement fixation (Fig. 5). The wound was irrigated with 9 L pressurized, pulsed saline wash followed by low pressure 6 L 0.02% aqueous Chlorhexidine wash. Absorbable Vicryl sutures were used for deep layers followed by subcuticular monofilament absorbable skin closure.
Postoperatively, the patient was given a further 48 h of intravenous antibiotics and 2 weeks of oral antibiotics. Immediate rehabilitation was with 50% weight-bearing immediately post fixation for 6 weeks. Venous thromboembolism prophylaxis was undertaken with Aspirin 150 mg once daily for 6 weeks as per routine departmental protocols. After clinical and radiological review at 6 weeks, the patient was progressed to full weight-bearing. Clinical and radiological union were evident at the 6-month stage and with no post-operative complications.
At 1-year follow-up, this patient was independently mobile, back to regular long-distance cycling, and walking 10,000 steps a day. He reported excellent patient reported outcome at 1 year with an Oxford Hip Score of 48/48 and reported no issues with his THA.
To the best of our knowledge, this is the first published case report of an open 3A VTB2W PPF in a fully cemented THA which underwent internal fixation with double plating. Although the number of PPFs are on the rise with a reported incidence of approximately 1%, an open PPF of the femur is rare due to the large amount of soft-tissue surrounding the femur. A high-energy injury is required to create the fracture and significant soft-tissue injury causing an open injury. The 1-year mortality rate among those with PPF (11%) is lower than hip fracture (16.5%) but higher than primary THA (2.9%) group [15].
The recommended treatment option for VTB2 by the Vancouver classification is revision arthroplasty with a longer stem by passing the fracture site, internal fixation is increasingly undertaken around VTB2 fractures with polished tapered stems especially when the stem has not subsided significantly and is minimally displaced within the cement mantle [16]. Internal fixation is a less invasive procedure with lower risk of complication for patients and a lower risk of post-operative dislocation. This can be especially useful in the management of polymorbid elderly patients [16, 17]. It is important when internally fixed then anatomic reduction of the cement mantle and fracture is performed for good results to be achieved [18].
Some authors propose that reducible fracture patterns with adequate bone stock might benefit from ORIF alone (well-fixed cement mantle, no loss of fragments) or ORIF with cement-in- cement revision (deficient mantle, fragment loss) [19, 20].
Maggs et al. [20] proposed a modification of the Vancouver classification to include a subclassification of B2 fractures around cemented femoral prostheses to include B2W (where cement is well fixed to bone) and B2L (where cement is loose). Although this patient had a loose stem, his bone cement interface was intact; therefore, he was classified as B2W. Studies have shown that when the bone cement interface is intact and the fracture can be anatomically reduced, all Vancouver B fractures around Exeter Stems can be managed successfully with fixation rather than revision arthroplasty surgery. It has also been shown that fixation was associated with reduced need for blood transfusion, lower risk of revision surgery, shorter anesthetic, and surgical time compared with revision arthroplasty [21, 22].
Double plating for PPF has been shown to provide superior outcomes in terms of union, functional outcomes, and lower complication rates [22]. It allows immediate post-operative full weight-bearing after ORIF post-PPF [23]. In a biomechanical study, double plating was shown to increase stiffness, stability, and the number of cycles to failure was significantly higher than a single plate [24]. In the Exeter Hip Unit, we commonly double plate femoral PPF that is elected to be treated with internal fixation to increase the rotational stability of the construct and allows patients to full weight bear.
To the best of our knowledge, there is only one published case report of an open PPF femur around a THA [15]. It was a Vancouver C 3A in a fully cemented THA in a patient who sustained a polytrauma. The PPF femur fracture was fixed with a single lateral proximal femoral locking plate. The author did not give details of the outcome post fixation in terms of union, complications, or outcome scores.
This is the first reported 3A VTB2W PPF post-THA which underwent internal fixation using a technique of double femoral plating. Our patient had an excellent post-operative recovery, the patient reported outcomes along with bony union at 1-year follow-up with no evidence of infection at latest follow-up. We suggest ORIF with double plating in an open PPF VTB2W cemented stem that can be performed in similar cases if the fracture can be anatomically reduced and the bone cement interface is intact.
Open PPFs around a THA are rare. Double plating provides better rotational stability and allows earlier weight-bearing. We should have a low threshold for double plating these fractures when the bone cement interface is intact and the fracture can be anatomically reduced.
References
- 1.Horwitz IB, Lenobel MI. Artificial hip prosthesis in acute and nonunion fractures of the femoral neck: Follow-up study of seventy cases. J Am Med Assoc 1954;155:564-7. [Google Scholar]
- 2.Marsland D, Mears SC. A review of periprosthetic femoral fractures associated with total hip arthroplasty. Geriatr Orthop Surg Rehabil 2012;3:107-20. [Google Scholar]
- 3.Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. In: Clinical Orthopaedics and Related Research. United States: Lippincott Williams and Wilkins; 2004. p. 80-95. Available from: https://www.pubmed.ncbi.nlm.nih.gov/15057082 [Last accessed on 2020 Oct 20]. [Google Scholar]
- 4.Haasper C, Enayatollahi MA, Gehrke T. Treatment of Vancouver Type B2 Periprosthetic Femoral Fractures. Vol. 39. Berlin, Germany: International Orthopaedics, Springer Verlag; 2015. p. 1989-93. [Google Scholar]
- 5.Sidler-Maier CC, Waddell JP. Incidence and Predisposing Factors of Periprosthetic Proximal Femoral Fractures: A Literature Review. Vol. 39. Berlin, Germany: International Orthopaedics, Springer Verlag; 2015. p. 1673-82. [Google Scholar]
- 6.Lindahl H, Malchau H, Odén A, Garellick G. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Series B 2006;88:26-30. [Google Scholar]
- 7.Adolphson P, Jonsson U, Kalén R. Fractures of the ipsilateral femur after total hip arthroplasty. Arch Orthop Traumatic Surg 1987;106:353-7. [Google Scholar]
- 8.Rayan F, Konan S, Haddad FS. Uncemented revision hip arthroplasty in B2 and B3 periprosthetic femoral fractures-a prospective analysis. HIP Int 2010;20:38-42. [Google Scholar]
- 9.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect 1995;44:293-304. [Google Scholar]
- 10.Brady OH, Garbuz DS, Masri BA, Duncan CP. Classification of the hip. Orthop Clin North Am 1999;30:215-20. [Google Scholar]
- 11.Dargan D, Jenkinson MJ, Acton JD. A retrospective review of the Dall-Miles plate for periprosthetic femoral fractures: Twenty-seven cases and a review of the literature. Injury 2014;45:1958-63. [Google Scholar]
- 12.Lochab J, Carrothers A, Wong E, McLachlin S, Aldebeyan W, Jenkinson R, et al. Do transcortical screws in a locking plate construct improve the stiffness in the fixation of Vancouver B1 periprosthetic femur fractures? A biomechanical analysis of 2 different plating constructs. J Orthop Trauma 2017;31:15-20. [Google Scholar]
- 13.Lenz M, Stoffel K, Kielstein H, Mayo K, Hofmann GO, Gueorguiev B. Plate fixation in periprosthetic femur fractures Vancouver type B1-trochanteric hook plate or subtrochanterical bicortical locking? Injury 2016;47:2800-4. [Google Scholar]
- 14.Nanchahal: Standards for the Management of Open Fractures. Available from: https://www.scholar.google.com/scholar_lookup?title=Standards+for+the+Management+o f+Open+Fractures+of+the+Lower+Limb&author=J+Nanchahal&author=S+Nayagam&a uthor=U+Khan&publication_year=2009& [Last accessed on 2021 Jul 08]. [Google Scholar]
- 15.Aleem IS, Bhandari M, Elizalde SR. Early definitive fixation of an open periprosthetic femur fracture in the polytraumatized patient: A case report and review of the literature. J Orthop Case Rep 2016;6:33-6. [Google Scholar]
- 16.Solomon LB, Hussenbocus SM, Carbone TA, Callary SA, Howie DW. Is internal fixation alone advantageous in selected B2 periprosthetic fractures? ANZ J Surg 2015;85:169-73. [Google Scholar]
- 17.Joestl J, Hofbauer M, Lang N, Tiefenboeck T, Hajdu S. Locking compression plate versus revision-prosthesis for Vancouver type B2 periprosthetic femoral fractures after total hip arthroplasty. Injury 2016;47:939-43. [Google Scholar]
- 18.Baum C, Leimbacher M, Kriechling P, Platz A, Cadosch D. Treatment of periprosthetic femoral fractures Vancouver type B2: Revision arthroplasty versus open reduction and internal fixation with locking compression plate. Geriatr Orthop Surg Rehabil 2019;10:???. [Google Scholar]
- 19.Quah C, Porteous M, Stephen A. Principles of managing Vancouver type B periprosthetic fractures around cemented polished tapered femoral stems. Eur J Orthop Surg Traumatol 2017;27:477-82. [Google Scholar]
- 20.Maggs JL, Swanton E, Whitehouse SL, Howell JR, Timperley AJ, Hubble MJ, et al. B2 or not B2? That is the question: A review of periprosthetic fractures around cemented taper-slip femoral components. Bone Joint J 2021;103:71-8. [Google Scholar]
- 21.Powell-Bowns MF, Oag E, Ng N, Pandit H, Moran M, Patton JT, et al. Vancouver B periprosthetic fractures involving the Exeter cemented stem. Bone Joint J 2021;103:309-20. [Google Scholar]
- 22.Lodde MF, Raschke MJ, Stolberg-Stolberg J, Everding J, Rosslenbroich S, Katthagen JC. Union rates and functional outcome of double plating of the femur: Systematic review of the literature. Arch Orthop Trauma Surg 2021;???:???. [Google Scholar]
- 23.Takahashi D, Noyama Y, Asano T, Shimizu T, Irie T, Terkawi MA, et al. Finite element analysis of double‐plate fixation using reversed locking compression‐distal femoral plates for Vancouver B1 periprosthetic femoral fractures. BMC Musculoskeletal Disord 2021;22:276. [Google Scholar]
- 24.Wähnert D, Grüneweller N, Gehweiler D, Brunn B, Raschke MJ, Stange R. Double plating in Vancouver type B1 periprosthetic proximal femur fractures: A biomechanical study. J Orthop Res 2017;35:234-9. [Google Scholar]