Although CT-guided RFA is the gold standard in treating intra-articular osteoid osteomas, open excision is a safe and effective method to treat, especially in developing countries like India, with a lack of advanced machinery and infrastructure in every tertiary care hospital.
Dr. Rohan Ratra, Department of Orthopaedic Surgery, Himalayan Institute of Medical Sciences, Swami Ram Nagar, Dehradun - 248140, Uttarakhand, India. E-mail: rohanratra@gmail.com
Introduction:An osteoid osteoma is a benign bone tumor. It is quite common and has become a known entity to most orthopedists and radiologists since it was first reported by Jaffe in 1935. Considering its incidence, it is at third position in the list of most common benign tumors, with prevalence up to 11% among the benign tumors and 3% among primary bone tumors.
Case Report:Case 1 - A 15-year-old male presented with symptoms of left hip pain for 1 year. Radiographs were repeated by us at 1 year which revealed cortical thickening and sclerosis surrounding the central lucent nidus in the posterolateral aspect of femoral neck. The patient underwent en bloc resection of the lesion. Case 2 - A 13-year-old male presented with symptoms of left hip pain for 1⅟2 years. Radiographs revealed an irregular lucent area surrounded by sclerosis in inferior aspect of femoral neck. By gradual removal of overlying reactive bone, the underlying nidus was exposed. Excision with curettage and burr was applied to the nidus, with bone chips used to fill the cortical defect.
Results:Both the patients were followed for a period of 1 year from surgery as chances of recurrence of osteoid osteoma is within that period. In both the cases, Harris hip score improved from poor status pre-operatively to a score between 80 and 89 (good result) at 1 month, and >90 (excellent result) on further follow-ups. By 1 year, the lesion had healed and femoral neck size, neck shaft angle, and joint widening were also reduced to normal.
Discussion and Conclusion:Intra-articular osteoid osteomas behave differently than extra-articular tumors. The radiological and clinical features are different from extra-articular lesions. Computed tomography (CT)-guided radiofrequency (RF) ablation is a safe, effective, simple method to treat osteoid osteoma. Open excision can be performed in the absence of CT-guided RF ablation.
Keywords:Intra-articular, osteoid osteoma, open excision.
An osteoid osteoma is a benign bone tumor. It is quite common and has become a known entity to most orthopedists and radiologists since it was first reported by Jaffe in 1935 [1]. Considering its incidence, it is at third position in the list of most common benign tumors, with prevalence up to 11% among the benign tumors and 3% among primary bone tumors [2]. The natural history of the disease was comprehensively explained by Golding in 1954 [3]. According to Golding [3] and others who have reported on osteoid osteoma, the lesion is mostly recorded in 2nd and 3rd decade of life and males are more commonly affected [4, 5]. The tumor can involve almost any bone of the body but there is a predilection noted towards lower extremity bones; femur and tibia [6]. Most commonly, it involves the proximal femur while in spine posterior vertebral elements are exclusively involved [2]. Intra-articular osteoid osteomas (IAOO) are rare and have a non-specific presentation. Difficulty in diagnosing the tumor can lead to various complications such as secondary osteoarthritis, leg length discrepancies, muscle atrophy, and structural deformities [7, 8, 9]. The lesion typically consists of a small radiolucent nidus surrounded by sclerosis (1.5–2 cm). Histologically, it is similar to osteoblastoma with the exception that osteoblastoma is larger [2, 6].
Character of pain is typical, severe pain which gets aggravated at night and patients report pain relief with the use of non-steroidal anti-inflammatory drugs (NSAIDS). A drastic uprise in prostaglandin concentrations in nidus has been reported in the literature which explains the cause of severe pain [10, 11]. IAOO presents with pain, joint effusion, and decrease range of motion. A primary articular disorder usually presents with similar symptoms leading to a delay in diagnosis [2]. We report 2 children with IAOO in the femoral neck.
Case 1
A 15-year-old male presented with symptoms of left hip pain for 1 year. The pain was insidious in onset, activity associated, and got relieved with medications from local doctor. Pain gradually increased in intensity with severe pain at night. Pain typically got relieved with NSAIDS. There was no history fever, weight loss, loss of appetite, and evening rise of temperature. On examination, the pelvis was not tilted, and the left lower extremity was in external rotation. Hip tenderness was present and flexion, and rotation movements were painful and restricted. Routine hematology was normal. Acute phase reactants, i.e., erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were normal which helped to rule out the possibility of low-grade infection or tuberculosis. The radiograph was taken at 6 months by General Physician which was normal. Radiographs were repeated by us at 1 year which revealed cortical thickening and sclerosis surrounding the central lucent nidus in the posterolateral aspect of femoral neck (Fig. 1a and b). The patient had got a computed tomography (CT) scan done earlier which clearly demonstrated the lucent nidus surrounded by sclerotic rim (Fig. 1c). The patient underwent en bloc resection of the lesion. Anterior (Smith-Peterson) approach was used to gain access to the hip joint. The incision was made along the anterior half of iliac crest to Anterior Superior Iliac Spine, extending it down vertically. Superficial inter-nervous plane was made between sartorius and TFL. Lateral cutaneous nerve of thigh was identified and preserved. Deep plane was developed between rectus femoris and gluteus medius. This exposed the anterior joint capsule. To expose the femoral neck and head a T-shaped capsulotomy was performed (Fig. 1d). The lesion was identified by the surrounding sclerosis and the soft, curretable nidus in the middle. The lesion was removed using bone curette after unroofing the overlying reactive bone using bone osteotome.
Case 2
A 13-year-old boy presented with a history of pain in his left hip for 1⅟2 year. The pain was initially mild in intensity, intermittent, and relieved with NSAIDS. Pain gradually progressed in intensity and became constant. The patient denied any history of trauma at the onset of pain. There was no history fever, evening rise of temperature, weight loss, or loss of appetite. There was no complaint of swelling, weakness, or loss of function. Physical examination revealed decreased flexion and rotation movements at left hip. Limb lengths and gait were normal. Routine hematology was normal. Acute phase reactants, i.e., ESR and CRP were normal. Radiographs revealed an irregular lucent area surrounded by sclerosis in inferior aspect of femoral neck. Increases in neck shaft angle, enlarged femoral neck, and a widened joint space were identified (Fig. 2a). He subsequently had a magnetic resonance imaging scan of left hip which confirmed the presence of a small radiolucent nidus (<1 cm) surrounded by sclerosis in inferior aspect of femoral neck (Fig. 2b). By gradual removal of overlying reactive bone, the underlying nidus was exposed. Excision with curettage and burr was applied to the nidus, with bone chips used to fill the cortical defect. Similar to the first case, the surgical approach used was Smith-Peterson anterior approach to the hip.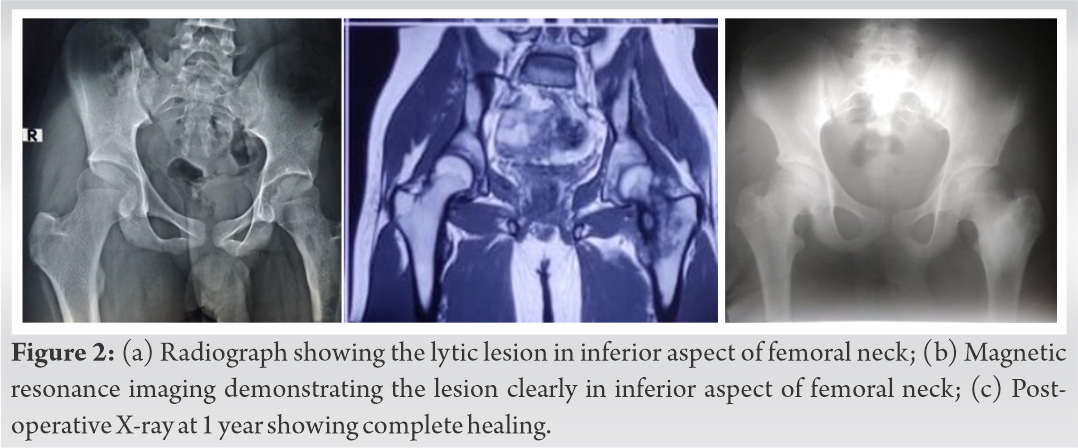
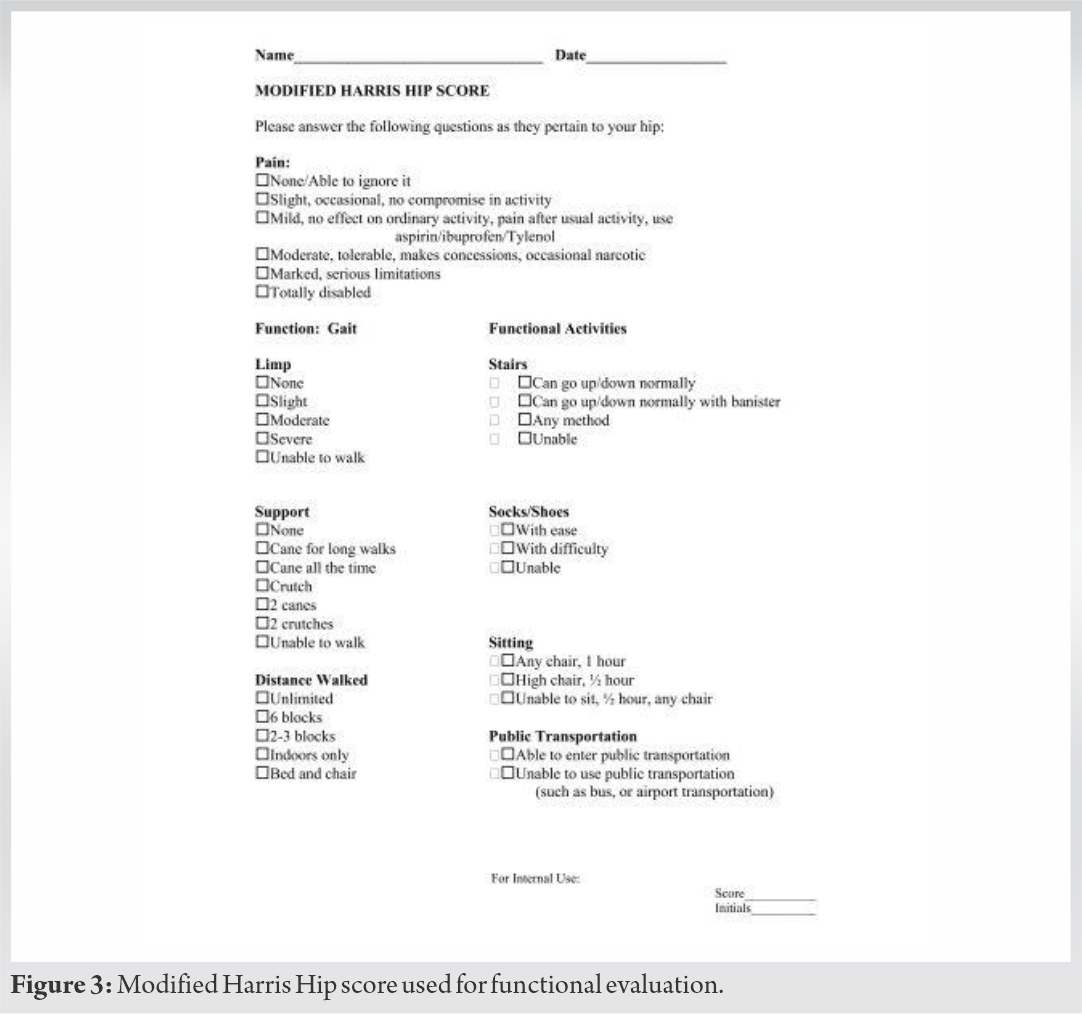
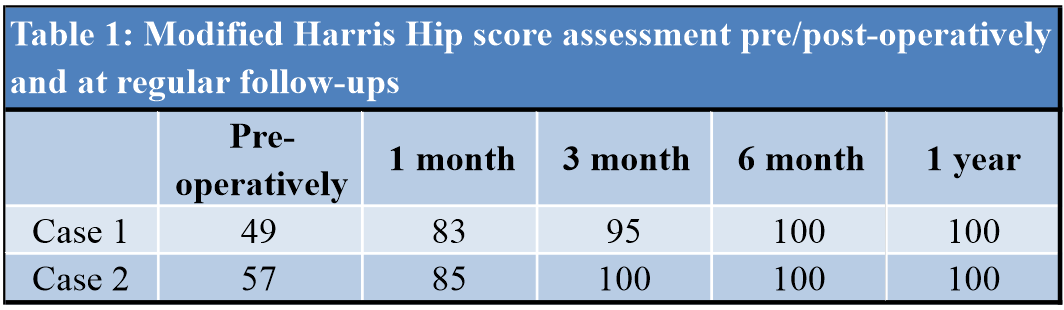
Both the patients were followed for a period of 1 year from surgery as the chances of recurrence of osteoid osteoma are within that period. No post-operative immobilization was given. An immediate relief from pain was seen during early post-operative period. Within 3 weeks from surgery, both the patients returned to their daily routine activities. No complication was seen postoperatively. At each follow-up at 1, 3, 6, and 12 months, functional outcome was assessed using the modified Harris hip score [12] (Fig. 3). The modified Harris hip score was scored from 0 (worst functional outcome and maximum pain) to 100 points (best functional outcome and least pain). The interpretation of the outcome was as follows: <70 (poor result), 70–79 (fair result), 80–89 (good result), and >90 (excellent result). In both the cases, Harris hip score improved from poor status pre-operatively to a score between 80 and 89 (good result) at 1 month and >90 (excellent result) on further follow-ups (Table 1). Radiographs were repeated at 1, 3, 6, and 12 months. They showed bone formation and healing of the lesion (Fig. 1e and f and 2c). By 1 year, lesion had healed and femoral neck size, neck shaft angle and joint widening also reduced to normal. Histological specimen from both the patients demonstrated pathological changes consistent with osteoid osteoma.
IAOO of hip can differ in clinical features from extra-articular osteoid osteoma. Patients usually have symptoms related to hip involvement rather than due to the lesion per se. Patient has variable articular pain, hip joint tenderness, effusion, and restricted range of motion. Patient complaints less of night pain and limited response to NSAIDS [13]. Radiographic features are also different from long bone osteoid osteoma. Periosteal reaction is less marked as periosteum is absent within the capsule. As a result of synovitis and effusion, joint space may be increased [14]. Although IAOO has the same histological features as long bone OO, non-specific clinical and radiographic features result in delayed or false diagnosis. A delay in diagnosis by 8–23 months has been reported in literature [9]. In our study, both the patients were diagnosed after a period of 1 year from the onset of symptoms. Both the children were diagnosed late but they did not develop any deformity. However, delayed diagnosis can lead to gait abnormalities and deformities in hip [9]. Routine radiographs may not demonstrate osteoid osteoma clearly. Secondary changes like increase in neck shaft angle, widened joint space, short and broad femoral neck, and osteoporosis may occur after several months. Pain may precede changes on radiographs by several months. Thus, further studies like CT-scan and bone scan are indicated to diagnose the disease at an early stage before development of secondary changes and deformities [15]. Bone scan reveals focally increased uptake corresponding to the lesion; however, in our study, bone scan was not performed. CT-scan was performed in our study which clearly demonstrated and determined size and location of lesion pre-operatively. After precise localization of the nidus, surgical excision has been the standard treatment for osteoid osteoma. We did open excision and curettage in both the cases due to unavailability of CT-guided RF services at our center and financial issues with the patients. In our study, both the patients were symptom free following surgery and there was no recurrence reported till last follow-up. The success rate following excision ranges from 88% to 100% [12]. Rosenthal et al. [16] in 1992 inculcated CT-guided method in the treatment protocol of osteoid osteoma. Since then, several studies have reported on percutaneous CT-guided radiofrequency (RF) ablation for the treatment of osteoid osteomas. CT-guided RF ablation utilizes a very small incision to allow insertion of the electrode. There is minimal soft tissue injury and minimal bone loss. However, according to a few reports CT-guided method may not be as effective as open excision in complete excision of the tumor. The possible complications of RF ablation include infection, bleeding, pathological fracture, injury to adjacent neural and vascular structures, abscess formation, and soft tissue injury (skin and muscle burns) [17]. This is a grey area, however, advantages of CT-guided method outweighs open excision of osteoid osteoma. Open surgery was performed in our cases with excellent results, with this in mind, in the era of percutaneous guided surgeries, open excision still plays an important role in developing countries of the world.
IAOO behaves differently than extra-articular tumors. The radiological and clinical features are different from extra-articular lesions. CT-guided RF ablation is a safe, effective, simple method to treat osteoid osteoma. Open excision can be performed in the absence of CT-guided RF ablation. Chances of complete excision and low recurrence rate also increase with open excision method.
References
- 1.1. Jaffe HL. Osteoid-osteoma: A benign osteoblastic tumour composed of osteoid and atypical bone. Arch Surg 1935;31:709-28. [Google Scholar]
- 2.2. Lee EH, Shafi M, Hui JH. Osteoid osteoma: A current review. J Pediatr Orthop 2006;26:695-700. [Google Scholar]
- 3.3. Golding JS. The natural history of osteoid osteoma; with a report of twenty cases. J Bone Joint Surg Br 1954;36:218-29. [Google Scholar]
- 4.4. Enneking: Musculoskeletal Tumors. New York: Churchill Livingstone; 1983. p. 1031-42. [Google Scholar]
- 5.5. Phalen GS, Patch DW Pain in the hip caused by osteoid osteoma. Clin Orthop 1954;4:154-9. [Google Scholar]
- 6.6. Heck KR Jr. Benign bone tumors and neoplastic conditions simulatingbone tumors. In: Canale ST, Beaty JH, editors. Campbell’s Operative Orthopaedics. 11th ed. Philadelphia, PA: Mobsy, Elsevier; 2011. p. 896-91. [Google Scholar]
- 7.7. Cassar-Pullicino VN, McCall IW, Wan S. Intra-articular osteoid osteoma. Clin Radiol 1992;45:153-60. [Google Scholar]
- 8.8. Greco F, Tamburrelli F, Ciabattoni G. Intra-articular osteoid osteoma. Ital J Orthop Traumatol 1992;18:63-9. [Google Scholar]
- 9.9. Xiao J, Lam SK, Shi Z, Zhou H, Luo X. Osteoid osteoma of the femoral neck causes deformity in children: A case report. HIP Int 2011;???:???. [Google Scholar]
- 10.10. Ciabattoni G, Tamburrelli F, Greco F. Increased prostacyclin biosynthesisin patients with osteoid osteoma. Eicosanoids 1991;4:165-7. [Google Scholar]
- 11.11. Makley JT, Dunn MJ. Prostaglandin synthesis by osteoid osteoma. Lancet 1982;2:42. [Google Scholar]
- 12.12. Vishwanathan K, Akbari K, Patel AJ. Is the modified Harris hip score valid and responsive instrument for outcome assessment in the Indian population with pertrochanteric fractures? J Orthop 2018;15:40-6. [Google Scholar]
- 13.13. Papagelopoulos PJ, Mavrogenis AF, Kyriakopoulos CK, Benetos IS, Kelekis NL, Andreou J, et al. Radiofrequency ablation of intra-articular osteoidosteoma of the hip. J Int Med Res 2006;35:537-44. [Google Scholar]
- 14.14. Helms CA, Hattner RS, Vogler JB. Osteoid osteoma: Radionuclide diagnosis. Radiology 1984;151:779-84. [Google Scholar]
- 15.15. Ahlfield SK, Makley JT, Derosa GP, Fisher DA, Mitchell JQ. Osteoid osteoma of the femoral neck in the young athlete. Am J Sports Med 1990;18:271-6. [Google Scholar]
- 16.16. Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteomacompared with operative treatment. J Bone Joint Surg Am 1998;80:815-21. [Google Scholar]
- 17.17. Campanacci M, Ruggieri P, Gasbarrini A, Ferraro A, Campanacci L. Direct visual identificationand intralesional excision of the nidus with minimal removal of bone. J Bone Joint Surg Br 1999;81:814-20. [Google Scholar]







