Emergent reduction of the elbow dislocation and anatomic reduction of the lateral condyle fracture is important to achieve satisfactory outcomes
Dr. Sanjeev Singh, Department of Orthopaedics, MGM Medical College and Hospital, Navi Mumbai - 410 209, Maharashtra, India. E-mail: sanjeevksingh1307@gmail.com
Introduction:Traumatic dislocations of the elbow are a rare injury in children. Concomitant elbow dislocations and lateral condyle fractures are even rarer. There is a wide variability in the outcomes of these injuries as there is no consensus regarding its management. We report one such rare case in a 7-year-old child.
Case Report:A 7-year-old child was brought to the emergency room with an alleged history of fall on outstretched hand sustaining injury to the left elbow. He was diagnosed with a posteromedial elbow dislocation, along with fracture of the lateral condyle. The patient underwent emergency reduction of the elbow under appropriate anesthesia following which there was persistence of varus and valgus instability, for which the lateral condyle was fixed with a standard pinning through a lateral approach with three Kirschner wires. The patient was immobilized for 6 weeks in a plaster, after which mobilization was done started. for the patient achieving 110 flexion post-surgery. At 3 months follow-up, the patient showed good functional outcome with full range of motion.
Conclusion:We report an exceedingly rare case of concomitant elbow dislocation and fracture of the lateral condyle in children. If emergent reduction of the dislocation and anatomic reduction of the fracture is achieved, satisfactory outcomes can be expected. Delayed recovery of the elbow motion is common, but full range of motion can be expected in the long run.
Keywords:Elbow, lateral condyle, dislocation, trauma.
Traumatic dislocation of the elbow is a rare injury in children constituting 3–6% of all elbow injuries [1, 2]. Ninety-five percent of elbow dislocations constitute posterior and of these 70% are posterolateral. Although both elbow dislocations [3] and lateral condyle fractures (LCFs) of the humerus [4] are common in the pediatric population, the concomitant presentation of both these injuries is rare.
More commonly, elbow dislocation in this population is associated with fracture of the medial epicondyle [3]. Reports of a concomitant pediatric LCF of the humerus and an elbow dislocation are scarce, with only some anecdotal cases reported [5, 6, 7, 8, 9, 10, 11, 12]. A direct adducting force exerted on a partially flexed elbow during a fall on an outstretched hand [5] is responsible for the avulsion of the lateral condyle of the humerus and posteromedial dislocation of the elbow [7, 8, 9, 10, 11]. There is wide variability in the reported outcomes of this injury, although some authors have reported good results with the early reduction of the dislocation with either closed or open reduction and internal fixation of the LCF [6, 8, 9]. Others have described suboptimal outcomes associated with malunion, nonunion, and limitations in range of motion [5, 7, 10, 11].
The purpose of this case report is to discuss the treatment and outcomes of these exceedingly rare condition injury and to review the literature.
A 7-year-old boy was brought to the emergency room with an alleged history of fall on an outstretched hand while cycling sustaining injury to his right elbow. Following injury, the patient developed swelling, deformity, and difficulty in using the extremity. There was no history of other related or remote trauma. The radiographs of the affected region were advised and showed a posteromedial elbow dislocation with a fracture of lateral condyle (Fig. 1).
An emergent reduction of the dislocation was planned with simultaneous fixation after informed consent of the parents and under appropriate anesthesia. Elbow was reduced with gentle traction and flexion with pressure from the medial aspect of the elbow to guide it into reduction. Clinical assessment of reduction was done with the regain of the normal contour of the elbow and smooth motion arc. The adequacy and concentricity of the reduction were confirmed by the image intensifier (Fig. 2). Post-reduction the joint was unstable to varus and valgus stresses. Through a standard lateral approach, the lateral humeral condyle was anatomically reduced and three (1.25 mm) Kirschner’s wires were used to fix it. Reduction checked under image intensifier and intra-operative arthrogram (Fig. 3).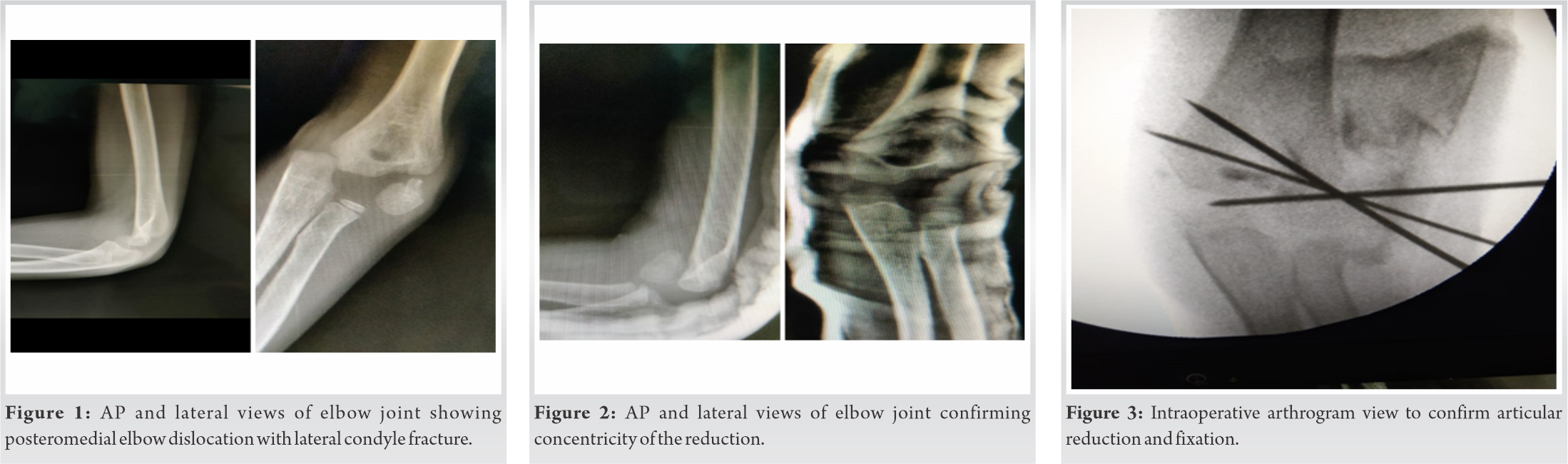
Postoperatively, a back slab was applied for 2 weeks. Stitches were removed and the slab was converted to a long-arm cast. At 6 weeks, the cast and wires were removed, radiograph (Fig. 4) was found to be satisfactory, and rehabilitation started with an active-assisted range of motion. Final follow-up at 3 months revealed good functional and radiologic results (Fig. 5, 6). The range of motion was 0–110° (as compared to 0–120° in opposite elbow) and there was no varus/valgus instability.
In the pediatric population, the association of elbow dislocation and a LCF is rare. Available reports on this issue are scarce and mostly limited to single cases, with wide variability in the reported outcomes. As the elbow joint is a hinge requiring mobilization to avoid notorious stiffness, prompt diagnosis and emergent reduction of the dislocation followed by stable fixation of lateral condyle fragment are necessary for achieving the objective.
According to Milch Classification, Milch type 2 injuries which include the fracture line traversing the trochlear groove are more common than Milch type 1 injuries which are thought to be more stable due to the presence of trochlear rim [10].
The present study reports the outcome of a 7-year-old boy who presented to our institution with concomitant elbow dislocation and a LCF Song type V. The initial radiographs demonstrated a posteromedial dislocation. The elbow dislocation was successfully reduced by closed manipulation followed by an anatomic reduction of the LCF by open reduction. No complications were seen in the perioperative period, and full range of motion was observed within 6 weeks after removal of the wires with union ensured clinico-radiologically.
Kirkos et al. [7], in a study, observed excellent range of motion in three patients and 15 degrees extension lag in one patient due to a small intra-articular gap due to inappropriate reduction. Cheng et al. [5] reported three cases with elbow dislocation associated with LCF and observed suboptimal range of motion in two cases, the authors observed that poor functional range of motion is inevitable in case of unsatisfactory anatomical reduction by either open or closed reduction and if the joint is incongruent. Tomori et al. [13] emphasized to increase awareness of these injuries for achieving satisfactory outcomes. Silva et al. [14] reported that satisfactory outcomes can be expected if prompt reduction and anatomical reduction is achieved in his case series of 12 cases with a mean follow-up of 51 weeks.
Available literature data have suggested that the combination of an elbow dislocation and a LCF in the pediatric population is rare and often suboptimal articular reduction can culminate in nonunion/malunion/stiffness, thereby resulting in poor outcomes. Author recommends use of intraoperative arthrogram for anatomical reduction. Also, Author recommends a proposed management algorithm (Table 1).
We report an exceedingly rare case of concomitant posteromedial elbow dislocation with LCF in the pediatric age group. Emergent reduction and anatomical reduction is the key to satisfactory outcomes. Delayed recovery of elbow motion is common, but full recovery of the ROM can be expected in the long term.
Emergent reduction and anatomical reduction is the key to achieving good outcomes in concomitant elbow dislocation with LCF.
References
- 1.Canale ST. Elbow Dislocations. In: Canale ST, Beaty JH, editors. Operative Pediatric Orthopaedics. St Louis, Baltimore: Mosby Yearbook; 1991. p. 978-9. [Google Scholar]
- 2.Wilkins KE. Dislocations of joints of the elbow. In: Rockwood CA, Wilkins KE, King RE, editors. Fractures in Children. Vol. 3. Philadelphia, PA: JB Lippincott Company; 1991. p. 532-54. [Google Scholar]
- 3.Wilkins KE, Beaty JH, Chambers HG, Wilkins KE. Fractures and dislocations about the elbow region. In: Rockwood CA Jr., Wilkins KE, Beaty JH, editors. Fractures in Children. Philadelphia, PA: Lippincott Raven; 1996. p. 680. [Google Scholar]
- 4.Beaty JH, Kasser JR. The elbow: Physeal fractures, apophyseal injuries of the distal humerus, osteonecrosis of the trochlea, and T condylar fractures. In: Beaty JH, Kasser JR, editors. Rockwood and Wilkins’ Fractures in Children. Philadelphia, PA: Lippincott Williams and Wilkins; 2006. p. 591-660. [Google Scholar]
- 5.Cheng PG, Chang WN, Wang MN. Posteromedial dislocation of the elbow with lateral condyle fracture in children. J Chin Med Assoc 2009;72:103-7. [Google Scholar]
- 6.Eksioglu F, Uslu MM, Gudemez E, Cetik O. Medial elbow dislocation associated with a fracture of the lateral humeral condyle in a child. Orthopedics 2008;31:93. [Google Scholar]
- 7.Kirkos JM, Beslikas TA, Papavasiliou VA. Posteromedial dislocation of the elbow with lateral condyle fracture in children. Clin Orthop Relat Res 2003;408:232-6. [Google Scholar]
- 8.Marcheix PS, Vacquerie V, Longis B, Peyrou P, Fourcade L, Moulies D. Distal humerus lateral condyle fracture in children: When is the conservative treatment a valid option? Orthop Traumatol Surg Res 2011;97:304-7. [Google Scholar]
- 9.Pouliart N, De BH. Posteromedial dislocation of the elbow with associated intraarticular entrapment of the lateral epicondyle. J Orthop Trauma 2002;16:53-6. [Google Scholar]
- 10.Rovinsky D, Ferguson C, Younis A, Otsuka NY. Pediatric elbow dislocation associated with a milch Type I lateral condyle fracture of the humerus. J Orthop Trauma 1999;13:458-60. [Google Scholar]
- 11.Sharma H, Sibinski M, Sherlock DA. Outcome of lateral humeral condylar mass fractures in children associated with elbow dislocation or olecranon fracture. Int Orthop 2009;33:509-14. [Google Scholar]
- 12.van Haaren ER, van Vugt AB, Bode PJ. Posterolateral dislocation of the elbow with concomitant fracture of the lateral humeral condyle: Case report. J Trauma 1994;36:288-90. [Google Scholar]
- 13.Tomori Y, Nanno M, Takai S. Posteromedial elbow dislocation with lateral humeral condylar fracture in children. Medicine 2018;97:e12182. [Google Scholar]
- 14.Silva M, Cooper SD, Cha A. Elbow dislocation with an associated lateral condyle fracture of the humerus: A rare occurrence in the pediatric population. J Pediatr Orthop 2015;35:329-33. [Google Scholar]









