2nd Ray amputations may result in instability of the tarso- metatarsal with ensuing midfoot deformity, which must be monitored with serial clinical and radiographic examination of the foot.
Dr. Aditya Menon, Department of Orthopaedics, P D Hinduja Hospital and Medical Research Centre, Veer Savarkar Marg, Mahim (West), Mumbai - 400 016, Maharashtra, India. E mail: docmenon83@gmail.com
Introduction:Lower limb amputations secondary to diabetic foot infection/osteomyelitis (OM) are the most common cause for non-traumatic amputations of the lower extremity. Hind/midfoot amputations are commonly done for metatarsal (MT) OM. They are, however, associated with higher complication and revision rates and often lead to below knee amputation. In comparison, distal/forefoot toe disarticulation/ray amputation (R amp) have lesser revision rates/complications and give better functional outcome. Here, we report a case of 2nd R amp with an uncommon complication.
Case Report:A 42-year-old male with uncontrolled diabetes and bilateral diabetic neuropathy presented with discharging sinus over plantar aspect of the left foot since 1 week. There was no evidence of underlying OM on MRI. Wound healed with soft-tissue debridement and empirical antibiotics (culture negative) for 2 weeks. Re-debridement was done for a wound gape 6 weeks later. Infection resolved with targeted antibiotics (oral ciprofloxacin and doxycycline) for Enterobacter cloacae given for 1 month. Six months later, he developed pain and swelling in the left foot following prolonged barefoot walking and possible injury with a stone. There was local redness, swelling, and a plantar sinus. MRI revealed septic arthritis of the left 2nd metatarsophalangeal (MTP) joint, OM of the 2nd MT head, and an encapsulated soft-tissue abscess. Aggressive debridement with 2nd R amp and careful separation of encapsulated abscess was done leaving behind base of 2nd MT to maintain stability of the Lisfranc joint. Wound healed primarily. Targeted antibiotics for Methicillin Susceptible Staphylococcus aureus were given for 6 weeks. Good diabetic control and avoiding bare foot walking were advised and he is infection free, fully functional, and asymptomatic at 36 months. However, he was noted to have developed valgus deformity of the midfoot secondary to Charcot osteoarthropathy of the Lisfranc joints at 36 months follow-up, involving 1st, 3rd, and 4th TMT joints. The other foot did not show any evidence of Charcot arthropathy.
Conclusion:Recurrent wound infections with subsequent OM are a common feature of diabetic foot. R amps have better functional outcomes with preserved foot stability, shorter length of hospitalization, and associated costs as compared to hind/midfoot amputations. They may, however, develop Charcot osteoarthropathy due to the void between adjoining MTs resulting in altered forces across the Lisfranc joints. Surgeons must beware of this complication, especially following R amps and monitor these patients with serial clinical and radiographic examination.
Keywords:Diabetic foot infection, amputation, diabetic neuropathy, osteomyelitis, diabetic foot ulcer, surgery, antibiotics, conservative surgery, Charcot neuropathy.
Recurrent wound infections with subsequent osteomyelitis (OM) are a common feature of diabetic foot (DF) [1]. Lower limb amputations secondary to diabetic foot infections (DFI), especially DF Osteomyelitis, are the most common cause for non-traumatic amputations of the lower extremity [1]. Hind/midfoot amputations are commonly done, especially for infections of the forefoot [2]. They are, however, associated with wound breakage, complications and revision rates. Forefoot amputations such as ray amputation (R amp) or toe disarticulation have better functional outcomes, lesser revision rates, and in hospital stay [3, 4]. Here, we report a case of 2nd R amp with an uncommon complication.
A 42-year-old male with uncontrolled diabetes and bilateral diabetic neuropathy presented with discharging sinus over plantar aspect of the left foot since 1 week. Dorsalis pedis (DP) and posterior tibial (PT) artery pulsations were palpable. Diabetic control was poor (HbA1c – 10 %). Complete blood count (CBC – 11350 g/l) and erythrocyte sedimentation rate (ESR – 20 mm/hr) were raised. MRI showed abnormal soft-tissue enhancement on the plantar aspect of 2nd MT head and 2nd MTP joint with no underlying OM (Fig. 1). Wound was debrided and healed after secondary closure and 2 weeks of empirical antibiotics (negative deep tissue culture). Re-debridement was done for a wound gape 6 weeks later. Deep tissue cultures grew Enterobacter cloacae. Wound healed subsequently after 1 month of oral ciprofloxacin and doxycycline as prescribed by the infections disease specialist. Medical management of diabetes was supervised by the endocrinologist. However, 6 months later, he developed pain and swelling in the left foot following prolonged barefoot walking and possible injury with a stone (Fig. 2).
There was local redness, swelling, and a plantar sinus. Glycosylated hemoglobin showed poor diabetic control over the preceding months due to non-compliance with the prescribed medication (HbA1c – 11.7 %). CBC (12170 g/l) and ESR (81 mm/h) were raised. DP and PT artery pulsations were palpable. Radiographs showed destruction of the left 2nd MT head, neck and base of proximal phalanx of 2nd toe with a soft-tissue shadow (Fig. 3). MRI films showed septic arthritis of the left 2nd metatarsophalangeal (MTP) joint, OM of the 2nd metatarsal (MT) head, and a soft-tissue abscess (Fig. 4).
As the infection was restricted to 2nd ray and the abscess was well encapsulated, 2nd R amp was considered as the best way to excise infected tissues with a margin of normal tissues. Second R amp involving en bloc excision of infected tissues with a clean skin and soft-tissue margins was subsequently done leaving behind base of 2nd MT to maintain stability of the Lisfranc joint (Fig. 5, 6, 7).
Deep tissues cultures at this stage grew Methicillin Susceptible Staphylococcus aureus, treated with intravenous Flucloxacillin for 2 weeks followed by oral Cephalexin for 4 weeks. Following wound healing (Fig. 8), he could ambulate independently with modified footwear with arch support.
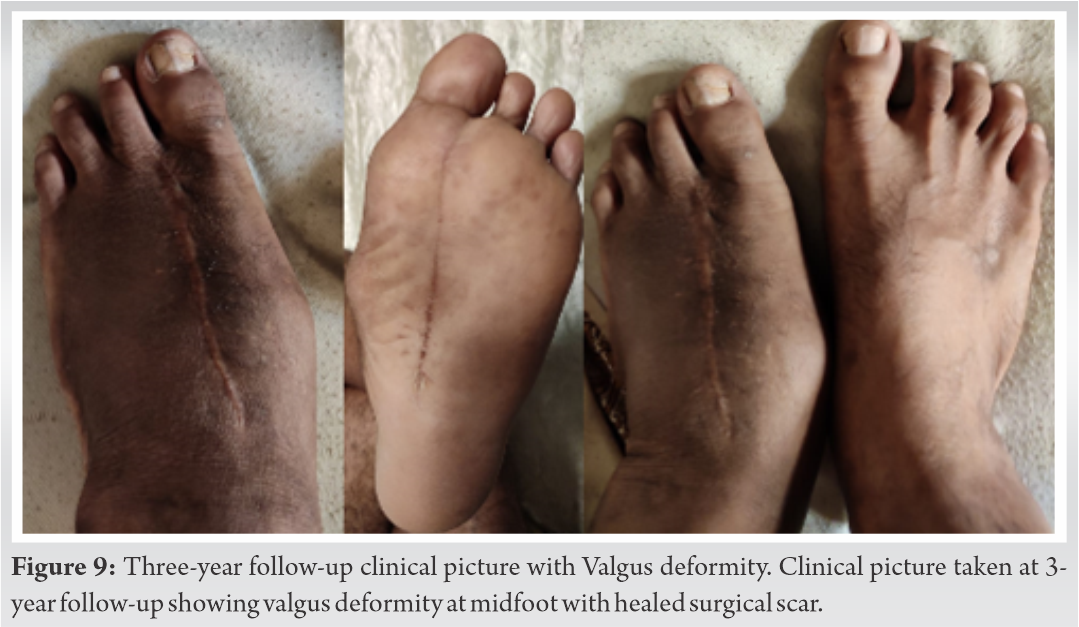
He had an infection free, asymptomatic 36 months follow-up and foot was functionally normal. At this stage, however, a valgus deformity of the midfoot was noted (Fig. 9).
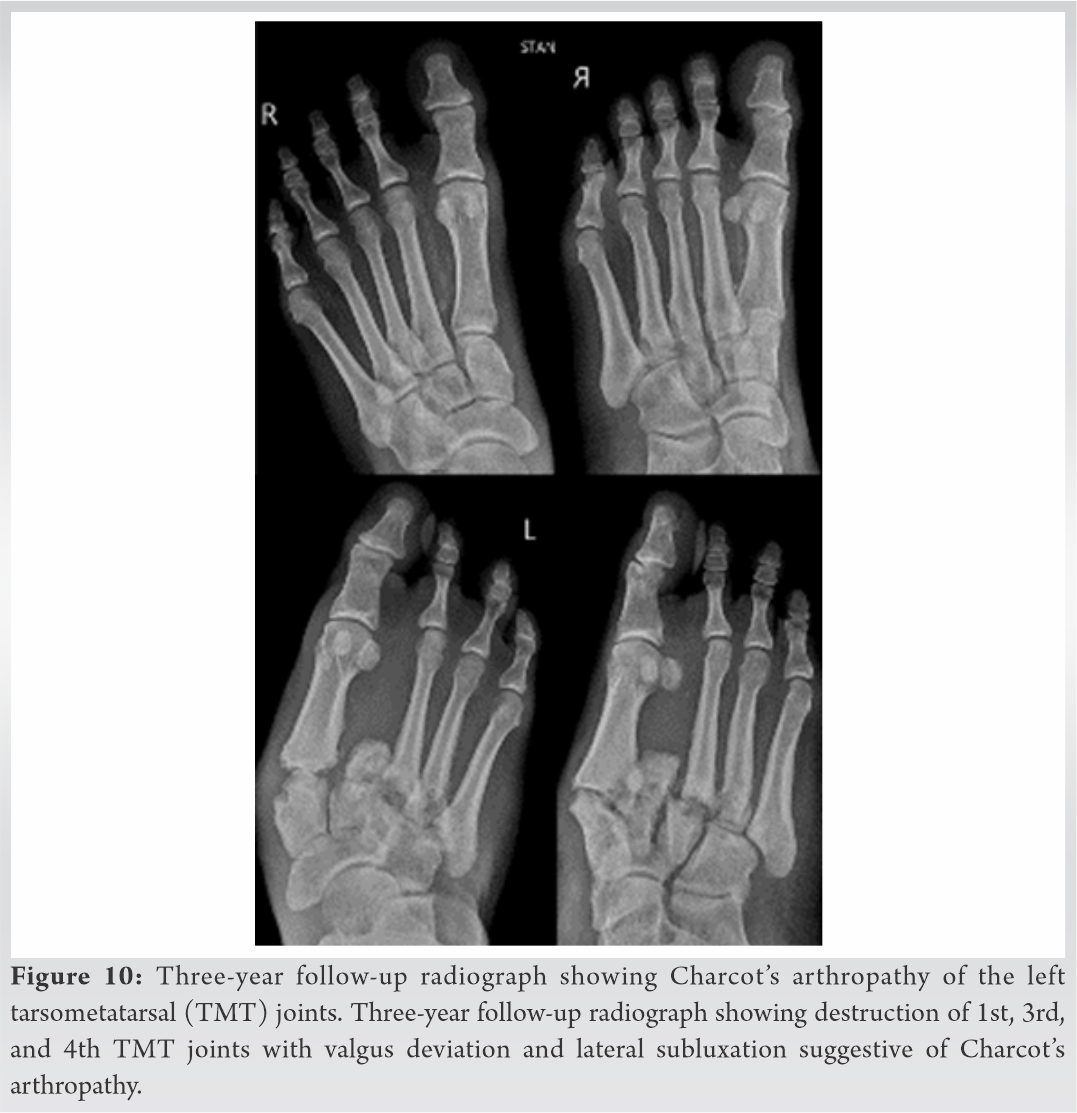
Radiographs showed valgus deformity of the midfoot with Charcot’s osteoarthropathy of the Lisfranc joints; involving 1st, 3rd, and 4th tarsometatarsal (TMT) joints (Fig. 10). As he was asymptomatic, he was advised supervised inaction and was ambulating independently with modified footwear.
Management of DFI has changed significantly over the last decade with every attempt to achieve infection remission along with a functionally viable foot [5]. MT OM is managed surgically with a wide array of surgeries from local debridement and curettage to R amps to mid/hind foot amputations [2, 6].
Tarsometatasrsal amputations (TMAs) are commonly done for MT OM. They are, however, associated with high rates of repeated surgeries, wound healing complications, muscular imbalances, and require modified footwear [3, 4]. Twenty-seven percent (8/27) patients with midfoot amputation following diabetic gangrene had wound healing complications necessitating BKA in a series published by Elsharawy [7]. These cases subsequently revised to BKA. Anthony et al. and Pollard et al. reported much higher (82% and 54%, respectively) complication rates following TMA [2]. In contrast, R amp has much lesser complications/revision rates and has better long-term functional outcome [1, 2, 3, 4]. Wong et al. and Borkosky and Roukis have shown success rates of up to 70–80% in their series [8, 9]. R amp is classically indicated in OM of MT with septic arthritis of the MTP joint [10]. Our case had OM of 2nd MT with soft issue abscess and septic arthritis of 2nd MTP joint. Although TMT amputation could have been done, R amp scores over it functionally as well as aesthetically. It is hence more acceptable to Indian population. He could ambulate independently with modified footwear with an arch support. At 3-year follow-up, the patient developed a valgus deformity of the midfoot was noticed. Radiographs revealed Charcot’s osteoarthropathy involving the 1st, 3rd, and 4th TMT joints (Lisfranc joints) with resultant valgus deviation. Opposite foot radiographs did not show any such changes. Fontalis et al. were the first to report on Charcot’s osteoarthropathy following R amp of the 1st or 5th MTs [13]. They postulated that the same could be due to increased pressures across the midfoot caused by destabilization following R amp. They recommend that this could indicate the need for enhanced foot protection following R amp. In contrast, our patient had a 2nd R amp and yet developed the deformity. This could possibly be due to the void left following MT excision between the adjoining 1st and 3rd MTs. Even modified footwear may not be able to prevent this deformity since the 1st ray would tend to drift towards the void left by 2nd R amp. Pressure changes across the TMT joint as described by Fontalis et al. could also have contributed to the same. The authors could not find any literature on Charcot’s osteoarthropathy following 2nd R amp.
R amps have better functional outcomes with preserved foot stability, shorter length of hospitalization, and associated costs. They have significantly lesser revisions/wound breakdowns as compared to TMA. Similar to 1st and 5th Ramp, a 2nd R amp could also destabilize the midfoot resulting in subsequent Charcot’s osteoarthropathy and midfoot deformity. Surgeons must be aware of this complication and monitor the foot with serial clinical and radiographic examination.
References
- 1.Second R amps may result in instability of the TMT joint due to the void between the adjoining MTs with ensuing Charcot osteoarthropathy and midfoot deformity. Surgeons must be aware of this complication, more commonly seen following 1st and 5th R amps. The patient must be advised to follow-up regularly for serial clinical and radiographic examination of the foot. [Google Scholar]