JFCs should be considered in the differential diagnosis of calcified extradural lesions.
Dr. Katsunori Fukutake, Department of Orthopedic Surgery, Toho University Omori Medical Center, Ota-Ku, Tokyo, Japan. E-mail: katsunori.fukutake@med.toho-u.ac.jp
IntroductionJuxta-facet cysts (JFCs) are extradural lesions. Calcification of cyst walls is often reported, although completely calcified facet cysts are extremely rare.
Case PresentationA 65-year-old man presented with a 1-year history of the right lower extremity weakness and pain, and chronic low back pain. Imaging showed hypointensity on T1- and T2-weighted magnetic resonance images which can be very well appreciated on a completely calcified computed tomography mass arising from the right L3/4 facet joint. The patient underwent a total cyst removal with a facetectomy of the right L3/4 facet, and L3 to L4 posterior fusion.
ConclusionWe presented a case of a completely calcified JFC in a patient with back pain and radiculopathy who underwent cystectomy and spinal fusion. JFCs should be considered in the differential diagnosis of calcified extradural lesions.
KeywordsJuxta-facet cysts, calcified, case report.
Juxta-facet cysts (JFCs) are extradural lesions from the facet joints or that have grown into the ligament flavum, which was initially used by Kao to describe both synovial and ganglion cysts [1]. The pathogenesis remains unclear, but most authors suggest that it may develop due to excessive joint mobility with degenerative spondylosis and/or spondylolisthesis [2, 3, 4]. This excessive joint mobility results in weakening of the joint capsule and synovial fluid herniation [5]. These patients can be asymptomatic or may present with back pain or radiculopathy. Characteristic magnetic resonance imaging (MRI) of facet cysts shows hypointensity on T1-weighted images and hyperintensity on T2-weighted images. However, in this case, hypointensity was observed on T1- and T2-weighted images, which can be very well appreciated on computed tomography (CT). Calcification of cyst walls is often reported, although completely calcified facet cysts are extremely rare. To the best of our knowledge, only two cases of completely calcified JFCs have been reported previously in the English-language literature [6, 7]. Here, we present a case of a completely calcified JFC in a patient with back pain and radiculopathy who underwent cystectomy and spinal fusion.
History
The patient was a 65-year-old man who presented with a 1-year history of the right lower extremity weakness and pain, and chronic low back pain. Three months before admission to our hospital, the right lower extremity weakness worsened. He had a gait disorder at the time of presentation due to pain in the right lateral thigh and right lower extremity weakness. The patient had no significant medical history and did not take medications.
Physical examination
The femoral nerve stretching test was positive on his right leg. Both lower extremity tendon reflexes were intact; however, weakness in the right lower extremities (iliopsoas muscle MMT4 and quadriceps femoris MMT4) was observed. Hyposensation (fine touch 7/10) was observed in the right lateral thigh. The Japanese Orthopedic Association score was 13 points (3–4–6–0).
Imaging studies
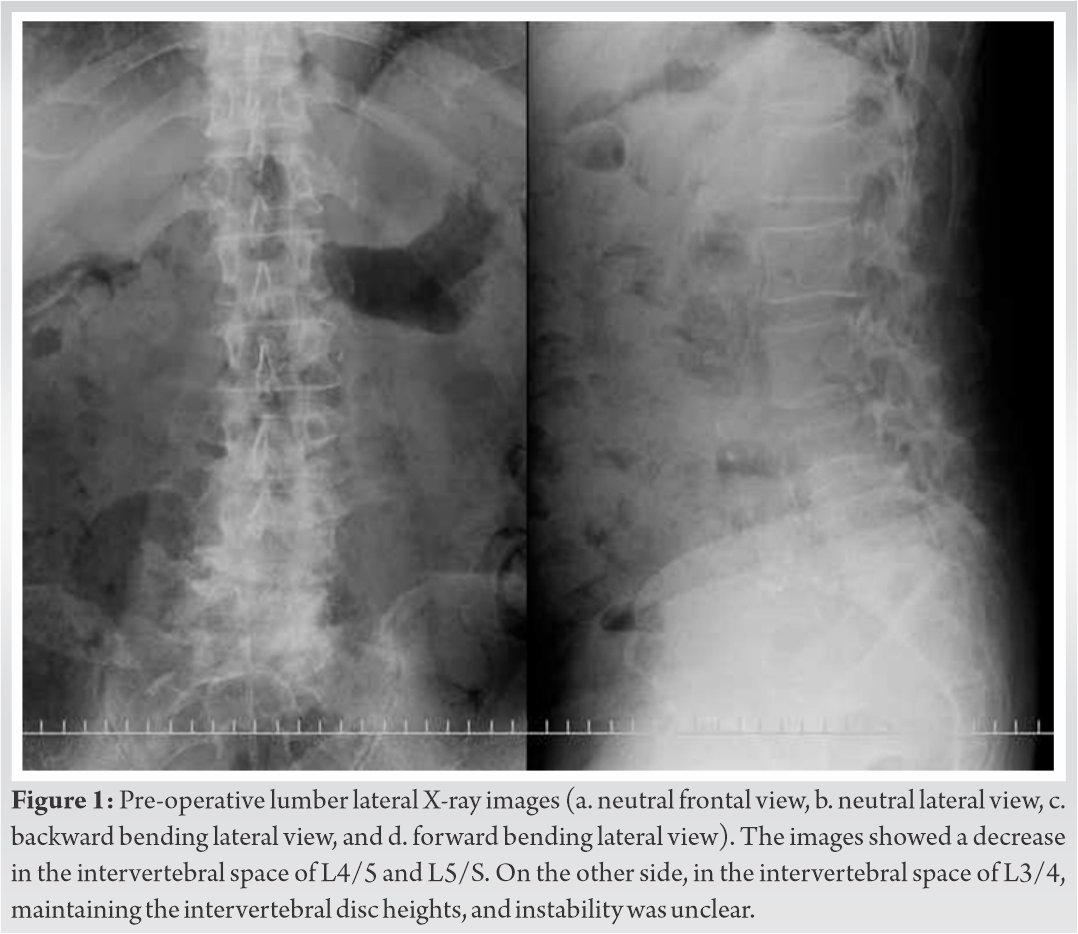
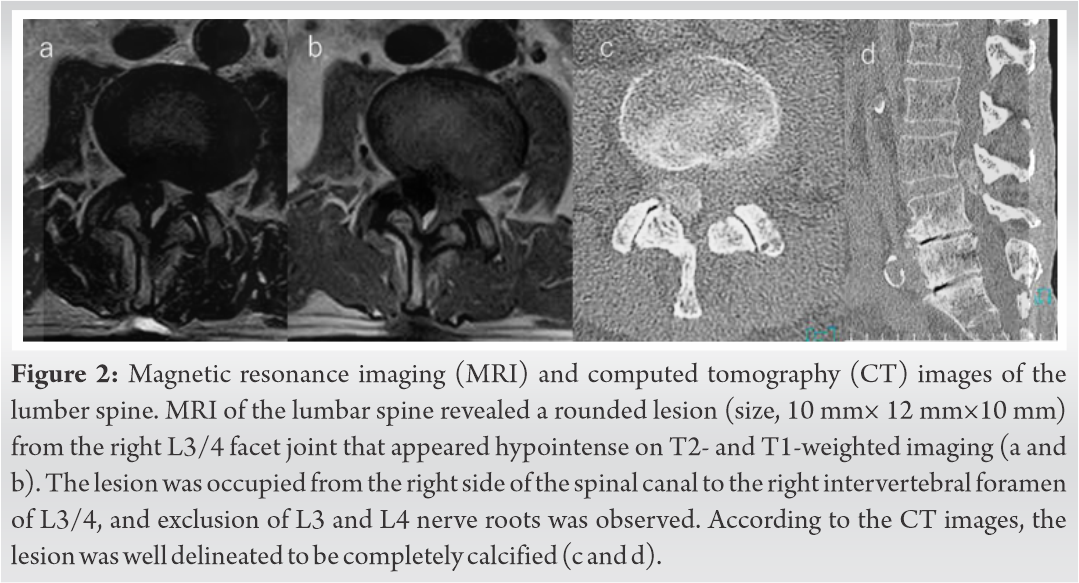
X-ray images showed a decrease in the intervertebral space of L4/5 and L5/S. On the other side, in the intervertebral space of L3/4, maintaining the intervertebral disc heights, and instability was unclear (Fig. 1). MRI of the lumbar spine revealed a rounded lesion (size, 10 mm × 12 mm × 10 mm) from the right L3/4 facet joint that appeared hypointense on T1- and T2-weighted MRI (Fig. 2a and b). The lesion occupied the right side of the spinal canal to the right intervertebral foramen of L3/4, and exclusion of L3 and L4 nerve roots was observed. By CT imaging, the lesion was well delineated to be completely calcified (Fig. 2c and d).
Post-hospitalization course
The patient’s most remarkable symptom was pain in the right lateral thigh and weakness of the right lower extremity, and we diagnosed radiculopathy due to a calcified JFC. The patient underwent total cyst removal with facetectomy of the right L3/4 facet, and L3 to L4 posterior fusion (Fig. 3). Facetectomy was essential for reliable decompression of nerve roots. The cyst wall was fragile and adhered to the surrounding tissue and easily teared, making it difficult to remove as a mass. Finally, the cyst was resected completely, and the cyst contents and wall were submitted as pathological specimens. Intraoperatively, the lesion was compressing the thecal sac and noted to consist of a paste like material that was not ossification.
Post-operative course
On the 1st day after the operation, rehabilitation started with a hard lumbar corset. The post-operative hospital course was unremarkable. The right lateral thigh pain was improved, and weakness gradually recovered. Twelve days after surgery, the patient was discharged.
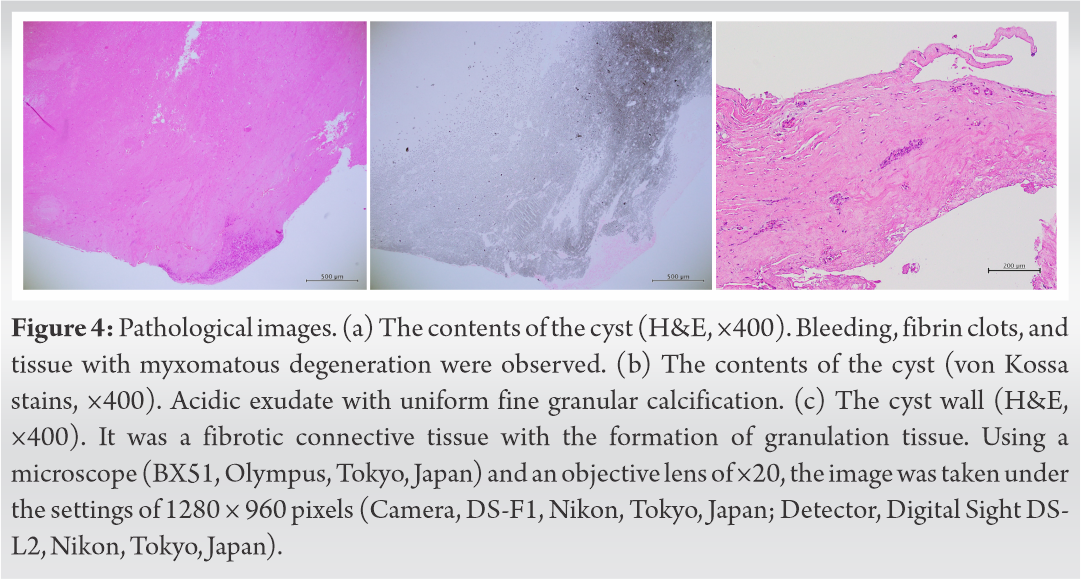
A pathological image (H&E, × 400) was provided and showed bleeding, fibrin clots, and tissue with myxomatous degeneration as the contents (Fig. 4a). In addition to von Kossa staining, it provided acidic exudate with uniform fine granular calcification (Fig. 4b). The cyst wall was fibrotic connective tissue with the formation of granulation tissue (Fig. 4c). Histologic analysis identified that the lesion was a simple pseudocyst, containing calcified material.
JFCs are extradural lesions from the facet joints or have grown into the ligament flavum, which was initially used by Kao [1] to describe both synovial and ganglion cysts. The pathogenesis remains unclear, but some reports have suggested that the pathogenesis of lumbar JFCs involves facet degeneration caused by various factors that lead to a weakening of the joint capsule [2, 3, 4]. This weakening allows herniation of the synovium, and synovial fluid fills the newly formed cavity and becomes a cyst, which communicates with the associated joint [8, 9]. In this case, the mobility of the lower lumbar spine was reduced because of degeneration of the intervertebral discs of L4/5 and L5/S1. Therefore, mechanical stress was applied to the facet joints of L3/4 as the adjacent segment.
. Calcification of cyst walls is often reported, although completely calcified facet cysts are extremely rare. Some differential diagnoses are considered calcified spinal extradural lesions, such as synovial osteochondromatosis [10], tumoral calcinosis [11], calcium pyrophosphate dehydrate crystal deposition disease [12], and lumbar presentation of ossification of the ligamentum flavum [13].
To the best of our knowledge, only two cases of completely calcified JFCs have been reported previously in the English-language literature [6, 7]. In both cases, facetectomy and posterior fusion were performed due to the size and mineralization of the lesion and showed good results.
Surgical treatment options for JFCs are simple laminotomy with cystectomy and spinal fusion if needed [14, 15]. Tubular surgery has also been described as minimally invasive spinal surgery [16]. However, calcified JFCs have a risk of calcified dural membranes and there is a possible difficulty in cystectomy due to adhesion. It is necessary to prepare for facetectomy and spinal fusion. In our case, it was believed that a facetectomy was necessary for reliable decompression of nerve roots; therefore, we performed a facetectomy of the right L3/4 facet, and L3 to L4 posterior fusion. The dural membrane and the cyst capsule were adhered and required careful peeling and facet joint resection was required for total cyst resection.
Here, we report a case of a completely calcified JFC in a patient who underwent cystectomy and spinal fusion. There was no recurrence of low back pain or leg pain in the post-operative course, and no recurrence of JFCs was observed on the images.
JFCs should be considered in the differential diagnosis of calcified extradural lesions.
References
- 1.1. Kao CC, Winkler SS, Turner JH: Synovial cyst of spinal facet. Case report. J Neurosurg 1974;41:372-6. [Google Scholar]
- 2.2. Yong-Hing K, Kirkaldy-Willis WH. The pathophysiology of degenerative disease of the lumbar spine. Orthop Clin North Am 1983;14:491-504. [Google Scholar]
- 3.3. Park WM, Kim K, Kim YH. Effects of degenerated intervertebral discs on intersegmental rotations, intradiscal pressures, and facet joint forces of the whole lumbar spine. Comput Biol Med 2013;43:1234-40. [Google Scholar]
- 4.4. Cho IY, Park SY, Park JH, Suh SW, Lee SH. MRI findings of lumbar spine instability in degenerative spondylolisthesis. J Orthop Surg (Hong Kong) 2017;25:2309499017718907. [Google Scholar]
- 5.5. Salmon B, Martin D, Lenelle J, Stevenaert A. Juxtafacet cyst of the lumbar spine. Clinical, radiological and therapeutic aspects in 28 cases. Acta Neurochir (Wien) 2001;143:129-34. [Google Scholar]
- 6.6. Huang KT, Owens TR, Wang TS, Moreno JR, Bagley JH, Bagley CA. Giant, completely calcified lumbar juxtafacet cyst: Report of an unusual case. Global Spine J 2014;4:175-8. [Google Scholar]
- 7.7. Kasliwal MK, Deutsch H. Completely calcified lumbar synovial cyst. Neurol India 2011;59:315-6. [Google Scholar]
- 8.8. Kao CC, Uihlein A, Bickel WH, Soule EH. Lumbar intraspinal extradural ganglion cyst. J Neurosurg 1968;29:168-72. [Google Scholar]
- 9.9. Jackson DE, Atlas SW, Mani JR, Norman D. Intraspinal synovial cysts: MR imaging. Radiology 1989;170:527-30. [Google Scholar]
- 10.10. Kim SW, Choi JH. Synovial chondromatosis presenting with lumbar radiculopathy. Spine (Phila Pa 1976) 2009;34:E414-7. [Google Scholar]
- 11.11. Carlson AP, Yonas HM, Turner PT. Disorders of tumoral calcification of the spine: Illustrative case study and review of the literature. J Spinal Disord Tech 2007;20:97-103. [Google Scholar]
- 12.12. Fujishiro T, Nabeshima Y, Yasui S, Fujita I, Yoshiya S, Fujii H. Pseudogout attack of the lumbar facet joint: A case report. Spine (Phila Pa 1976) 2002;27:E396-8. [Google Scholar]
- 13.13. Pantazis G, Tsitsopoulos P, Bibis A, Mihas C, Chatzistamou I, Kouzelis C. Symptomatic ossification of the ligamentum flavum at the lumbar spine: A retrospective study. Spine 2008;33:306-11. [Google Scholar]
- 14.14. Banning CS, Thorell WE, Leibrock LG. Patient outcome after resection of lumbar juxtafacet cysts. Spine (Phila Pa 1976) 2001;26:969-72. [Google Scholar]
- 15.15. Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: Clinical presentation, the role of spinal instability, and treatment. J Neurosurg 1996;85:560-5. [Google Scholar]
- 16.16. Sandhu FA, Santiago P, Fessler RG, Palmer S. Minimally invasive surgical treatment of lumbar synovial cysts. Neurosurgery 2004;54:107-11; discussion 111-2. [Google Scholar]