Treatment of distal radius fracture with extensive bone loss with masquelet technique using autograft from the proximal tibia is safe and effective.
Dr. Victor E. Greco, 14 Regina Street, Pittsburgh, Pennsylvania 15203, United States. E-mail: Greco81890@yahoo.com
IntroductionDistal radius fractures are one of the most common fractures in the United States. Treatment usually involves internal fixation using a volar Henry approach with placement of a volar locking plate. Optimal treatment becomes less apparent when significant bone loss occurs. No case of an open distal radius fracture treated using a staged Masquelet technique involving proximal tibial autograft is available in the literature. Herein, we describe and discuss a case report of a novel technique to treat a large (5 cm) bone defect for an open distal radius fracture.
Case ReportA 59-year-old man suffered an open, comminuted, and intra-articular distal radius fracture with 5 cm of bone loss. He was treated using a staged Masquelet technique with incorporation of ipsilateral proximal tibial autograft with a bone harvester to obtain cancellous autograft and bone marrow graft. The patient initially underwent emergent I and D, acute carpal tunnel release, and internal and external fixation. A 5 cm bone void was filled with antibiotic cement. Four weeks later, the antibiotic cement was removed, cancellous bone graft and marrow were harvested from the proximal tibia, and the graft was placed within the prior bone void. Fracture site healing was confirmed radiographically and with computer-tomography imaging 3 months later. The patient has demonstrated excellent results 1 year post-operative with 60° of wrist flexion, 40° of wrist extension with mild pain, and full finger range of motion with radiographic union.
ConclusionInternal fixation with placement of a volar locking plate remains the mainstay of treatment for distal radial fractures. However, in more comminuted fractures with bone loss, treatment becomes more challenging. We have presented a unique case utilizing a staged Masquelet technique with incorporation of a proximal tibial autograft to educate readers on an alternative option and technique for autograft donor sites in these more complicated fractures.
KeywordsDistal radius, autograft, tibia.
Injuries to the hand and wrist encompass 28.6% of all musculoskeletal injuries sustained to the musculoskeletal system [1]; moreover, distal radius fractures account for the most common form of upper extremity fractures [2]. The mechanism most commonly involves a fall onto an outstretched arm. Fixation involves internal fixation utilizing a volar Henry approach with placement of a volar locking plate. In more comminuted and complex fractures, a dorsal bridge plate and dorsal/radial locking plates may be used, or even an external fixator to maintain the length if significantly comminuted. Bone loss presents a challenging problem for reconstruction with numerous treatment options and techniques. A polymethylmethacrylate spacer can also be utilized in traumatic cases with extensive bone loss to induce a vascularized membrane (Masequelet technique). In our case report, we discuss a 59-year-old man who sustained a high energy, open, and comminuted distal radius fracture with 5 cm of bone loss that underwent a staged Masequelet technique utilizing antibiotic cement, as well as ipsilateral proximal tibial autograft and bone marrow harvest using a bone harvester to achieve bony union.
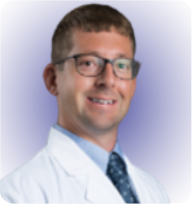
A 59-year-old man fell ~10 feet from a dump truck onto an outstretched arm. The patient was found to have a left open, severely comminuted distal radius and ulna fracture, and median nerve dysfunction (Fig. 1). The patient was emergently taken to the operating room for irrigation and debridement, acute carpal tunnel release, and open reduction with internal/external fixation. After thorough debridement under sterile conditions, a 5 cm bone void remained within the distal radial metaphysis (Fig. 2).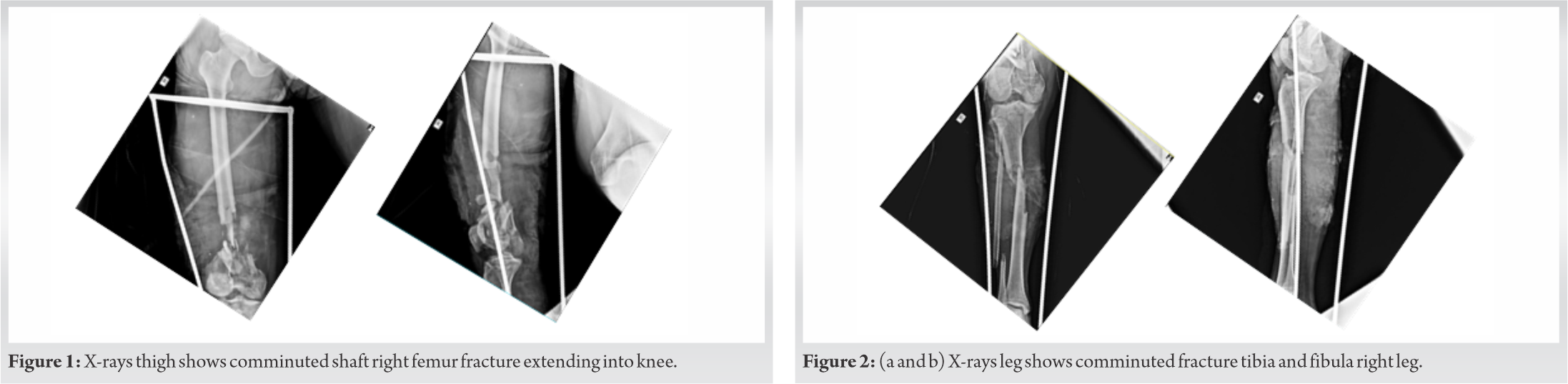 Utilizing the Masquelet technique, antibiotic cement was placed into the defect for the initial stage of the treatment. A volar plate was applied to the patient’s distal radius to span the fracture. The ulna was fixated with a 3.5 mm compression plate, being definitive fixation for this fracture. Finally, a wrist-spanning external fixator was applied to the patient’s left upper extremity for more rigid fixation (Fig. 3).
Utilizing the Masquelet technique, antibiotic cement was placed into the defect for the initial stage of the treatment. A volar plate was applied to the patient’s distal radius to span the fracture. The ulna was fixated with a 3.5 mm compression plate, being definitive fixation for this fracture. Finally, a wrist-spanning external fixator was applied to the patient’s left upper extremity for more rigid fixation (Fig. 3).
Four weeks later, the patient was taken back to the operating room; the external fixator was removed and a dorsal wrist-spanning bridge plate was placed using the prior incisions. A volar Henry approach was utilized to expose the volar aspect of the distal radius and remove the antibiotic spacer and plate. The proximal and distal aspects of the distal radius bone void were debrided until healthy and bleeding bone was visualized.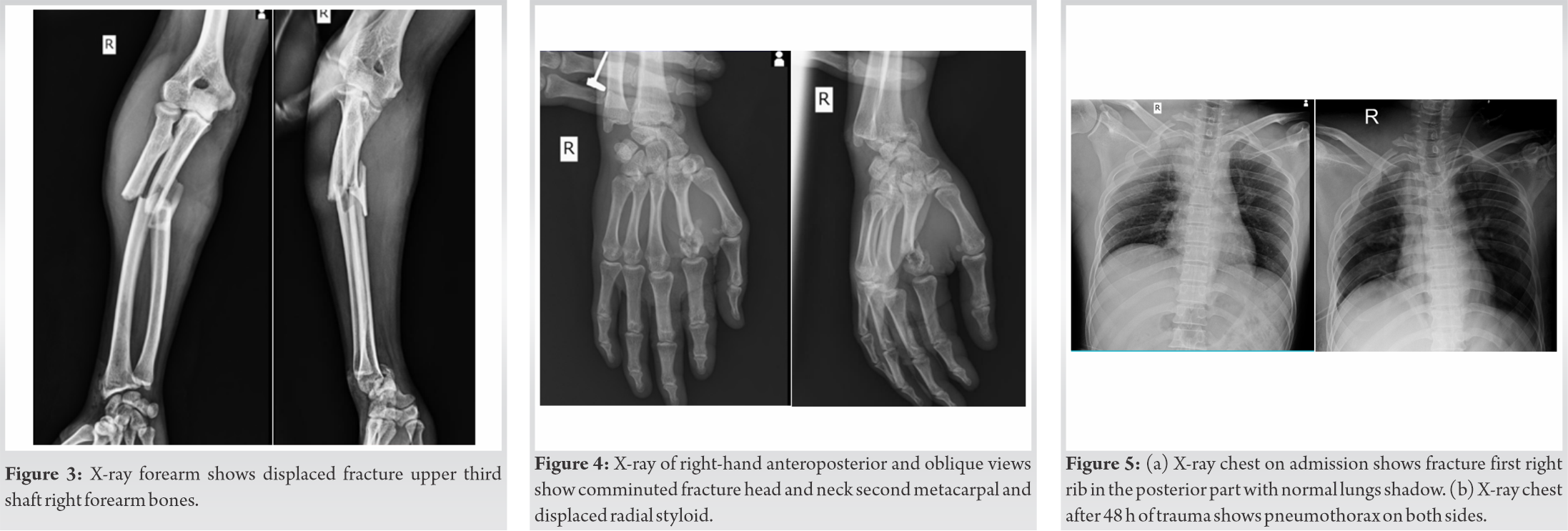
The ipsilateral tibia was chosen as the autograft bone harvest site to fill the void. After prepping and draping in a sterile fashion, Gerdy’s tubercle was identified by palpation and a 1.5 cm incision was made under fluoroscopy. During dissection, care was taken to divide the iliotibial band and periosteum in separate layers. Using the Avitus® Bone Harvester system (Shelton, computed tomography [CT]), a 1 cm corticotomy within the proximal tibia (PT) allowed entrance into cancellous tibial metaphysis. The bone harvester was then introduced through the cortical window as cancellous bone and marrow were harvested under fluoroscopy (Fig. 4). The Avitus® Bone Harvester is a sharp curette with a hollowed tube connected to suction allowing efficient harvesting of cancellous bone and marrow into its handle. Approximately 35 cc of cancellous bone and 25 cc of bone marrow were harvested (Fig. 5). The harvest site was then back-filled with synthetic calcium phosphate. Periosteum, fascia, and skin were primarily closed. The harvested bone graft and marrow were placed into the radial bone defect. Finally, a volar plate was placed to achieve adequate internal fixation.
Postoperatively, the patient’s left arm was placed into a sugartong splint for 2 weeks, allowing the skin to heal. He was also made non-weightbearing on his left lower extremity for a period of 6 weeks secondary to the large amount of bone graft harvested along with a body mass index of 44. By 2 weeks, the splint was removed and both the patient’s upper and lower extremity incisions had healed. He began weightbearing on his left lower extremity at 6 weeks without difficulty or pain. By 3 months, distal radius bony union was confirmed by both X-ray (XR) and CT (Fig. 6a, b). A 3-month post-harvest XR was also taken of the left PT which demonstrated no complication (Fig. 7).
After bony union had occurred, the patient was then taken back to the OR for a 3rd time for removal of dorsal bridge plating. He was weaned from a wrist orthosis and began extensive occupational therapy for wrist range of motion and strengthening. At 1-year follow-up, the patient had achieved 60° of wrist flexion, 40° of wrist extension with mild pain, which remains similar to baseline wrist pain before injury, and full finger range of motion (Fig. 8). The radiographs do demonstrate ulnar positive variance of roughly 2 mm in the setting of moderate-to-severe radiocarpal arthritis. However, the patient has mild arthritic symptoms and functional range of motion.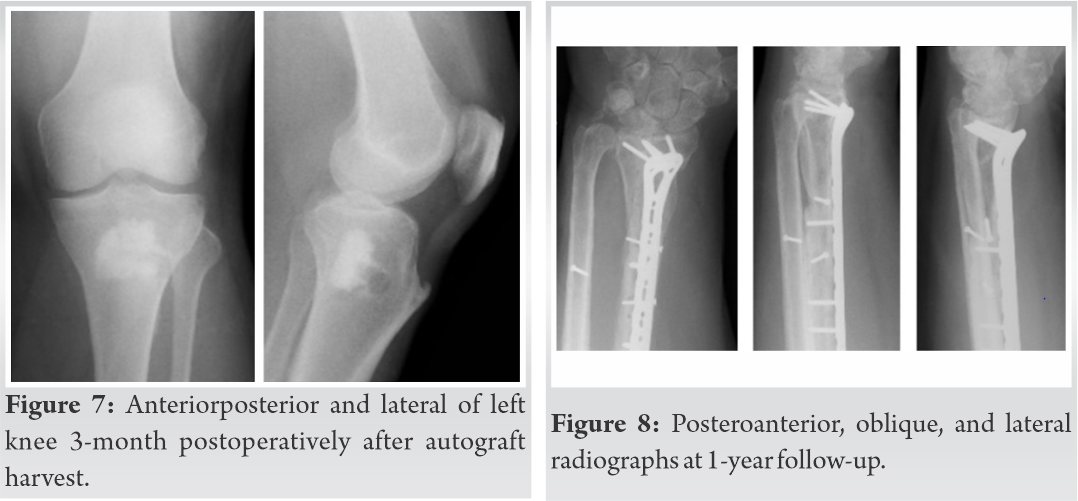
Distal radius fractures are one of the most common fracture in both the pediatric and adult population, accounting for approximately 25% and 18% of all fractures, respectively. Moreover, the incidence of distal radius fractures appears to be increasing in the US as well as worldwide [3]. These fractures are treated based on radiographic parameters and clinical examination. Surgical intervention of these fractures typically involves an open reduction and internal fixation depending on the angulation and nature of the fracture.
Distal radius fractures that result from high energy mechanisms or ballistics are often challenging to treat secondary to the amount of comminution and, frequently, bone loss. Surgeons may treat the bone voids with autograft bone, allograft bone, or commercially available biologic/synthetic bone substitutes. A recent Cochrane review of randomized control trials concluded that there was insufficient evidence for the use of allograft and bone substitutes in the treatment of distal radius fractures [4]. For bone defects greater than 6 cm, most authors recommend the use of autologous vascularized free fibula graft [5]. However, this comes with significant donor site morbidity and is typically reserved for younger patients without arthritic changes on radiographs.
There is a paucity of literature on the best bone graft or substitute for distal radius fractures with substantial bone loss <6 cm. Most authors would agree that autograft bone is the gold standard for that it has osteogenic, osteconductive, and osteoinductive properties with incorporation of the Masquelet technique. This technique, originally described in 1986, is a two-stage procedure to induce a reaction by placement of a foreign body (i.e., cement) to produce a biologic cavity that will prevent graft resorption, secrete growth factors, and promote graft revascularization. The second stage of the procedure, performed 4–8 weeks later, involves removal of the cement and placement of bone graft in the newly developed vascularized pseudomembrane which prevents graft resorption [6]. The iliac crest is a common source of autologous bone graft but it is not without risk of substantial complications including continued donor site pain, hematoma/neuroma formation, stress fracture, and infection. The reported prevalence of these complications ranging from 9% to 49% in some series [7].
A second autograft harvesting technique for bone-graft harvest is the Synthes Reamer-Irrigator-Aspirator System (West Chester, PA). This system harvests medullary autograft bone from the canal of the femur, utilizing low intramedullary pressure. This technique has been described for both distal radius fractures as well as wrist arthrodesis with successful bony union demonstrated in both reports [8]. Although relatively safe and reliable, a recent review of the RIA system demonstrated complications such as erosion of the femoral cortex, dislocation of the drill, fat embolism, infection, and blood loss requiring transfusion in 11 of 306 patients [9].
The PT is an alternative site of autologous bone graft harvest. With the development of the Avitus Bone Harvester, multiple sources of autograft can be harvested without significant technical difficulty (PT, distal tibia, andcalcaneus). This system utilizes a hollowed-curette with suction and filters to provide the ability to harness both cancellous autograft as well as bone marrow graft separately. This system has been popularized in foot and ankle surgery as a source of autograft, but has not been described in the literature for distal radius fracture bone grafting with concurrent bony void. In a paper presented at the AOFAS Annual Meeting in 2018, the authors describe nine patients who underwent harvest using this system. The mean incision length was 2 cm. Average graft obtained included 25 cm3 of cancellous graft and 21 cm3 of bone marrow aspirate. The mean procedure time was 5 min with average blood loss of 1 mL. No major or minor complications arose including fracture, infection, hematoma formation, sensory changes, or wound healing issues.
A study by Mauffrey et al. prospectively compared the amount of harvested bone between the anterior iliac crest and PT. They found no significant difference (6.2 cm3 vs. 7.3 cm3) in amount of graft harvested. Furthermore, patients in the PT group were found to have decreased pain at the harvest site on post-operative day (POD) 1, 5, and 14. At POD 28 and 56, however, no difference in donor site pain was noted [10]. Due to the acute post-operative harvest-site pain, this grafting technique may aid in short-term pain control without decreased harvest quantity.
In cases of open fractures, possible contamination, and large bone voids, our technique of bone grafting from the PT in a staged procedure after Masquelet is safe, effective, and achieved bony union with good clinical results. We utilized external fixation as well as the Masquelet technique to produce a biologic cavity that will prevent graft resorption, secrete growth factors, and promote graft revascularization. We chose the PT as the source of autograft for its low donor site morbidity, volume of cancellous bone/bone marrow aspirate available, and the ease of access to the donor harvesting site. The Avitus Bone Harvester allows the procurement of graft through a small incision. One of the drawbacks of this technique, especially in our case, is that the patient was made non-weightbearing on the donor lower extremity. Overall, the patient tolerated the harvest procedure well, has no post-operative pain at the donor site, is full weight bearing in both upper and lower extremity sites, and achieved bony union at 3 months.
Cases of open comminuted distal radius fractures with significant bone loss present an issue as to what surgical and bone grafting techniques are best. The purpose of this article is to educate rather than compare autograft donor sites and techniques as well as to inform its readers on an alternative option for autograft bone harvest for these challenging patients.
We describe a novel treatment of a distal radius fracture with extensive bone loss. Using a staged Masquelet technique, we created a biologic cavity and subsequently filled in with autograft harvested from the PT. The patient tolerated the procedures well and has achieved bony union and full weightbearing of upper and lower extremity sites at 3 months.
References
- 1.Angermann P, Lohmann M. Injuries to the hand and wrist. A study of 50,272 injuries. J Hand Surg Br 1993;18:642-4. [Google Scholar]
- 2.Shinohara T, Hirata H. Distal radius nonunion after volar locking plate fixation of a distal radius fracture: A case report. Nagoya J Med Sci 2017;79:551-7. [Google Scholar]
- 3.Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin 2012;28:113-25. [Google Scholar]
- 4.Handoll HH, Watts AC. Bone grafts and bone substitutes for treating distal radial fractures in adults. Cochrane Database Syst Rev 2008;2008:CD006836. [Google Scholar]
- 5.Adani R, Delcroix L, Innocenti M, Marcoccio I, Tarallo L, Celli A, et al. Reconstruction of large posttraumatic skeletal defects of the forearm by vascularized free fibular graft. Microsurgery 2004;24:423-9. [Google Scholar]
- 6.Karger C, Kishi T, Schneider L, Fitoussi F, Masquelet AC, French society of orthopaedic surgery and traumatology (SoFCOT). Treatment of posttraumatic bone defects by the induced membrane technique. Orthop Traumatol Surg Res 2012;98:97-102. [Google Scholar]
- 7.Ozer K, Chung KC. The use of bone grafts and substitutes in the treatment of distal radius fractures. Hand Clin 2012;28:217-23. [Google Scholar]
- 8.O’Callaghan PK, Matthews JH, Kirn PT, Angermeier EW, Kokko KP. Bone grafting in total wrist arthrodesis with large bone defects using the reamer-irrigator-aspirator: A case study of 2 patients. J Hand Surg Am 2019;44:620.e1-7. [Google Scholar]
- 9.Haubruck P, Ober J, Heller R, Miska M, Schmidmaier G, Tanner MC. Complications and risk management in the use of the reaming-irrigator-aspirator (RIA) system: RIA is a safe and reliable method in harvesting autologous bone graft. PLoS One 2018;13:e0196051. [Google Scholar]
- 10.Huang YC, Chen CY, Lin KC, Renn JH, Tarng YW, Hsu CJ, et al. Comparing morbidities of bone graft harvesting from the anterior iliac crest and proximal tibia: A retrospective study. J Orthop Surg Res 2018;13:115. [Google Scholar]