Haglund deformity and chronic tendoachilles tear can be managed well using double row suture anchor repair augmented with FHL graft and curettage of lipoma with filling the cavity using hydroxyapatite bone substitute is good choice for intraosseous lipoma.
Dr. Pranay Kondewar, Department of Orthopaedics, Grant Government Medical College, Mumbai, Maharashtra, India. E-mail: pranaypk1@gmail.com
Introduction: Achilles’ tendon is the largest tendon in the body, Tendon is an anatomical structure with inherent less blood supply and so more prone to injury and notorious healing outcomes. The management options for tendoachilles injury depend on the location of the tear, degree of retraction of the torn ends, and patient-related factors. Intraosseous lipoma is very rare benign tumor of bone accounting for 0.1% of all bone tumors. Most common site being proximal femur involvement of calcaneum is very rare presentation. Symptomatic patients with significant heel pain need operative intervention in the form of curettage alone or in combination with filling cavity with bone graft or bone graft substitutes. Many people use PMMA bone cement to fill the void.
Case Report: A 65-year-old male presented with chronic heal pain and difficulty in walking. On clinical examination and radiological investigation, calcaneal intraosseous lipoma was confirmed along with insertional tendinopathy of tendoachilles and haglund syndrome causing tear at insertion into calcaneal tuberosity. We managed this patient in single-stage surgery using tendoachilles split approach for removing haglund deformity and double row anchor suturing for tendon reattachment. Repair was augmented with flexor hallucis longus (FHL) graft fixed using interference screw in the calcaneum. Lipoma was approached with separate medial approach. Cortical window created, lipoma curettage was done, and cavity filled with hydroxyapatite bone graft substitute.
Conclusion: Tendoachilles split approach with double row suture anchor repair along with FHL graft gives good clinical outcome in insertional tendinopathy of tendoachilles with haglund syndrome. Curettage of intraosseous lipoma with filling the void using bone graft substitute such as hydroxyapatite gives good results and pain relief.
Keywords: Tendoachilles tear, calcaneal intraosseous lipoma, double row repair, hydroxyapatite flexor hallucis longus graft, haglund deformity.
Achilles’ tendon is the largest tendon in the body, formed from soleus and gastrocnemius. Tendon is an anatomical structure with inherent less blood supply and so more prone to injury and notorious healing outcomes. Tendoachilles is having least blood supply at a point 2.6 cm proximal to its insertion. In elderly patient, chances of tear increase to systemic medical conditions and age-related degenerative changes in the tendon [1]. The management options for tendoachilles injury depend on the location of the tear, degree of retraction of the torn ends, and patient-related factors. Options include direct end to end repair alone with krackow/Kessler/bunnell suturing technique. Augmentation of the repair with flexor hallucis longus (FHL) graft and fixation in calcaneum with interference e screw. Gastrocnemius v-y plasty and other muscle lengthening surgeries. Haglund syndrome is characterized as a painful posterosuperior deformity of the heel with possible causes as tight Achilles tendon, high-arched foot, and tendency to walk on the outside of the heel. Surgical treatment may be recommended in cases where of insufficient response to non-operative treatment. In this case, we have used the tendon split approach with double row suture anchor repair for combined tendoachilles tear and haglund deformity. This repair was augmented with FHL graft fixation in calcaneum using interference screw. This above combined technique helps to provide adequate structural strength to repair and improves the biology around the repair for early healing and rehabilitation [2]. Intraosseous lipoma is very rare benign tumor of bone accounting for 0.1% of all bone tumors. Most common site being proximal femur [3]. Lipomas are common benign soft-tissue tumors composed of mature adipose tissue with no evidence of cellular atypia. Benign lipomas can affect bone, joint and the tendon sheaths, and other soft tissues. Intraosseous lipoma is the rarest bone tumor [4]. Usually, its asymptomatic may cause pain in some patients. Asymptomatic cases can be managed conservatively. Symptomatic patients with significant heel pain needs operative intervention in the form of curettage alone or in combination with filling cavity with bone graft or bone graft substitutes. Many people use PMMA bone cement to fill the void, which enables early weight bearing in post-operative period. Sometimes lipoma can grow in size and can cause fracture of calcaneum, which needs additional surgical fixation using plate.
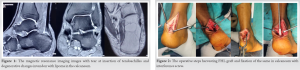
A 65-year-old male presented with complaints of pain in the left heel and difficulty in walking for 3 months. On examination, there was tenderness at insertion of tendoachilles. Thompson test was positive on further radiological examination X-ray suggested haglund deformity with calcification at tendoachilles insertion. There was a lytic radiolucent shadow in the calcaneum. For evaluating the lesion, magnetic resonance imaging was done which showed intraosseous lipoma of the calcaneum and tear of tendoachilles at insertion into the calcaneal tuberosity. There were retrocalcaneal bursitis and degenerative tear with calcification in the torn edges of tendon. Lipoma was located at junction of anterior process and body of calcaneum (Fig. 1).
Patient was operated in floppy lateral position with tourniquet. Adequate padding given to bony prominences. A posteromedial approach is used for the tendoachilles. A 6 cm incision taken slightly medial to the tendoachilles, paratenon incised retracted and preserved. The insertion of tendoachilles identified and torn end was separated from fibrotic tissue and debridement of the torn edges was done, tendoachilles incised from midline to get access to haglund deformity, it was removed step-by-step with osteotomes and smooth ended with burr. There was a spike present at most posterior part which was also excised. Round contour was achieved in posterior most part of calcaneum. Flexor hallucinations longus was identified behind the tendoachilles and was cut with keeping adequate length of its tendon. Later, a guide pin is passed in calcaneum and 5 mm tunnel was created then FHL graft was passed through tunnel and fixed with the interference screw (Fig. 2, 3).
Then 2 anterior row anchors were fixed in the calcaneum, one on medial and other on lateral side. Anchors with three fiber wires were used for this (two anchors with six fiber wires) and then three wires passed from the each torn edges of the tendon. Now, posteriorly two swivelock anchors were used for fixation, one medial and one lateral side. The wires from torn ends were pulled so that ends of the tendon comes closer and overlies on the bone (Fig. 4). Sutures were tied and cut. Paratenon was repaired, wound closed in layers. Patient was then turned in the supine position from floppy lateral and lesion was localized with fluoroscopy. A 3 cm incision was taken over the lesion on medial side, soft tissue, and tendons with neurovascular bundle retracted directly to visualize the bone over medial side of calcaneum. The location of the lesion is confirmed on fluoroscopy and a cortical window 1 × 1 cm was created and all the material within cavity taken out with multiple angled curettes and sent for histopathological analysis. The cavity cleaned with hydrogen peroxide wash and then it is packed with the hydroxyapatite bone substitute. Wound closed in layers. Slab given in 20° of equines from ventral surface. Suture removal is delayed till 21 days for better healing. Post-operative X-ray shows removed lesion with cavity completely filled by bone graft substitute (Fig. 5). At 3-week post-operative, below knee slab was given in neutral position of ankle and then in 15° dorsiflexion for next 3 weeks. Total immobilization for 9 weeks, after that partial weight bearing is initiated with boot walker and physiotherapy continued for 4 weeks.
At 1-year post-operative, there is no recurrence of the lesion and patient is able to walk pain free.
Intraosseous lipoma was first reported in 1910 by Wehrsig, who described this tumor in them proximal fibula of a 5-year-old girl [5]. Intraosseous lipoma has unknown ethology varying from traumatic onset and then fat degeneration/infection or osseous fat infarction with metaplasia/primary origin from marrow fat cells [6]. Symptoms depend on bone affected. Calcaneal lipoma presents as heel pain of chronic duration with incidental finding on X-ray imaging. Rarely, it presents with fracture. It can be managed conservatively with analgesic and anti-inflammatory medications/non-weight bearing frames. Surgery is advised when size is increasing on follow-up/increased symptoms/fracture on the bone. Based on histological findings, an intraosseous lipoma can be classified by Milgram classification system as follows: Stage I, a lesion composed of mature fat cells without calcification; Stage II, a predominantly fatty lesion with necrosis, focal calcification, or ossification; and Stage III, a fat-containing lesion with multiple necroses, extensive calcification, and cystic degeneration [7]. Although this staging does not correlate with pain. Intraosseous calcaneal lipoma is usually located at the junction of the anterior and middle third of the calcaneus, called as the neutral triangle. This area is devoid of the trabecular network crossing the calcaneum. Surgical management options for it include curettage of the lipoma through a cortical window in bone and then the cavity so created can be filled with various bone graft material or bone graft substitute such as hydroxyapatite, another method is filling the defect with PMMA cement which gives advantage of early weight bearing. When there is associated fracture of the bone, surgical fixation can be done. In a case series presented by the Kang et al. at a single institute, they had 21 pathologically confirmed cases of intraosseous lipoma, most common being femur and then others long bones least common being calcaneum. Surgical management was done as curettage and bone grafting which gave good clinical outcome [8]. As this case had combined pathology of calcaneal lipoma and haglund syndrome with tendoachilles tear; the management was complex and literature did not have any published case report on this clinical scenario.
It is observed and accepted that if <50% of the tendon is detached then it can be repaired without suture anchors but if its more than 50% then it is necessary to attach maximum of tendon to the footprint. In elderly patients, there is age-related degeneration within the tendon fiber and it leads to delayed healing and osseous integration after surgery so it is very important to restore the adequate pull out strength and local biology. To achieve above, we did use FHL graft and double row suture repair technique which gives maximum strength. Advantages of these include larger surface area for contact between bone and tendon which improves both local biology and strength of fixation. The anatomical proof and rationale behind double row repair than single row repair are that the area of insertion on calcaneal tuberosity is that various parts of tendoachilles such as medial and lateral head of gastrocnemius (MG and LG) and soleus insert at different part on tuberosity so double row repair ensures better reattachment of all the three components to their footprint and elderly patients have poor bone quality which decrease the pull out strength of anchor [9, 10].
Tendoachilles split approach with double row suture anchor repair along with FHL graft gives good clinical outcome in insertional tendinopathy of tendoachilles with haglund syndrome. It helps to restore normal pull out strength and local biology at insertion. Curettage of intraosseous lipoma with filling the void using bone graft substitute such as hydroxyapatite gives good results and pain relief.
Double row repair with FHL Grafting gives very good strength to the repaired tendon and early rehabilitation is possible with it. Filling cavity with bone graft or substitute after thorough excision is good option for the treatment of intraosseous lipoma.
References
- 1.Mahajan NP, Kondewar P, Gs PK, Marfatia A. Surgical management of chronic tendoachilles tear in elderly patients-a case series. J Orthop Case Rep 2021;11:57-62. [Google Scholar]
- 2.Güler Y, Birinci M, Hakyemez OS, Buyukdogan K, Çaçan MA, Arslanoglu F, et al. Achilles tendon-splitting approach and double-row suture anchor repair for Haglund syndrome. Foot Ankle Surg 2021;27:421-6. [Google Scholar]
- 3.Mawardi M, Hussin P. Intraosseous lipoma of the calcaneum: A rare cause of heel pain. Malays Fam Physician 2018;13:38-9. [Google Scholar]
- 4.Martínez MR, Corral FJ, García JR, Beltrán MM, Mendoza AC. Cystic lesion of the calcaneus Intraosseous lipoma. Reumatol Clin 2007;3:139-42. [Google Scholar]
- 5.Wehrsig G. Lipom des Knochenmarks. Z Allg Pathol 1910;21:243-7. [Google Scholar]
- 6.Sani MH, Bajuri MY, Shukur MH. Intraosseous lipoma of the calcaneus: The non-stereotypic lesion of the bone. New Horiz Clin Case Rep 2017;2:1-3. [Google Scholar]
- 7.Milgram JW. Intraosseous lipomas: A clinicopathologic study of 66 cases. Clin Orthop Relat Res 1988;231:277-302. [Google Scholar]
- 8.Kang HS, Kim T, Oh S, Park S, Chung SH. Intraosseous lipoma: 18 Years of experience at a single institution. Clin Orthop Surg 2018;10:234-9. [Google Scholar]
- 9.Ballal MS, Walker CR, Molloy AP. The anatomical footprint of the Achilles tendon: A cadaveric study. Bone Joint J 2014;96:1344-8. [Google Scholar]
- 10.Zhuang Z, Yang Y, Chhantyal K, Chen J, Yuan G, Ni Y, et al. Central tendon-splitting approach and double row suturing for the treatment of insertional Achilles tendinopathy. BioMed Res Int 2019;2019:10. [Google Scholar]