It is difficult to pre-operatively differentiate between cystic lesions in the distal phalanx but there are several features which, if present, should alert you to the possibility of an intraosseous epidermoid inclusion cyst.
Dr. Claudette Hewitt, Department of Trauma and Orthopaedic Surgery, London North West University Healthcare NHS Trust, Harrow, England. E-mail: claudette.hewitt@nhs.net
Introduction: Lesions in the distal phalanx can be attributed to a broad range of pathologies. Benign lesions such as enchondromas are common; however, there are a range of conditions that can mimic tumors on both clinical presentation and imaging.
Case Report: Here, we report a case of a 42-year-old man who presented with pain and swelling in the distal phalanx of his right ring finger following trauma. Plain radiographs showed a fracture through a probable enchondroma in the distal phalanx, and this report was corroborated by an MRI. However intraoperatively, the lesion was found to be a caseous lesion encased in a capsule and histological examination revealed the lesion to be an intraosseous epidermoid inclusion cyst.
Conclusion: In this report, we discuss how enchondromas can be differentiated from intraosseous epidermoid inclusion cysts on clinical and imaging appearances. Intraosseous epidermoid inclusion cysts are more common in young males, with the previous trauma at the site of the lesion. Radiographically intraosseous epidermoid cysts can be differentiated by enchondromas by the absence of calcification within the lesion, and the location of the lesion in the subungal part of the distal phalanx. Ultimately, however, the definitive diagnosis of both lesions is histological and therefore it is important to maintain a broad differential when approaching the diagnosis of distal phalanx lesions.
Keywords: Enchondroma, epidermal cyst, interosseous epidermoid inclusion cyst, epidermoid cyst.
Intraosseous epidermoid inclusion cysts in bone are extremely rare. They are not true neoplasms but are a well-defined cystic cavity with keratin and a peripheral zone of squamous epithelium [1]. They most often involve the skull and the distal phalanx of the fingers or toes [2]. In the phalanx, intraosseous epidermoid inclusion cysts present on imaging as destructive osteolytic lesions, which can be difficult to distinguish preoperatively from an enchondroma or other malignant lesions. We present a case of an intraosseous epidermoid inclusion cyst in the distal phalanx which falsely presented as an enchondroma on both X-ray and MRI imaging. The correct diagnosis was only reached following histological examination of the excised lesion. Here, we discuss the case and then review how the available literature can aid the pre-operative differentiation between enchondromas and intraosseous epidermoid inclusion cysts.
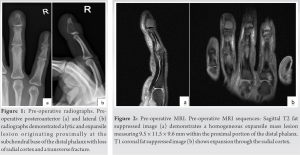
A 42-year-old male presented to our hospital following an injury to his right ring finger. He fell going up the stairs and stubbed his finger on a wall. He presented with right ring finger pain. He was generally fit and well with no medical history. He works as a hairdresser, reports no alcohol consumption, and is a social smoker. On examination, he had minimal tenderness to the radial aspect of distal phalanx of the right ring finger. There was swelling, clubbing, and redness to the finger but the skin was intact. He had a full range of movement of the finger with no neurovascular deficit. Initial X-ray showed a fracture through a probable enchondroma in the distal phalanx of the right ring finger (Fig. 1).
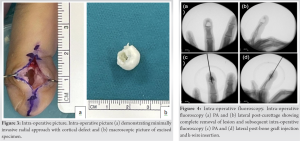
The fracture was initially managed nonoperatively with a splint. Serial X-rays were taken following the initial injury. There was no radiographic evidence of fracture union, instead the X-rays suggested that the suspected enchondroma was enlarging. Operative management was agreed and a pre-operative MRI was performed, which showed a 9.5 × 11.5 × 9.6 mm well defined mass lesion with expansion through the radial cortex. T2 fat sequences showed foci of hyperintensity within the lesion that may represent internal calcification, and these features were felt to be in keeping with an enchondroma (Fig. 2). Pre-operative quickDASH score was 13.6. Surgical intervention was carried out under general anesthetic, with local anesthetic infiltration. Tourniquet time was 48 min. A radial midlateral incision was performed under loupe magnification and the digital nerve branches were protected. Intra-operative examination revealed a capsule encased caseous lesion of the radial half of the distal phalanx, with extensive bony destruction. There was no radial or dorsal cortex, and a thin ulnar, and volar cortex.
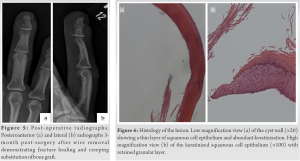
The capsule was removed (Fig. 3) and the distal phalanx was curetted and washed out. 2 cc of a synthetic injectable composite calcium sulfate and phosphate graft was utilized as a void filler. A 1.2 mm k-wire was inserted retrograde crossing the distal interphalangeal joint (Fig. 4) due to the significant bone defect. The wound was closed with 5/0 nylon and a zimmer splint was fitted. He was discharged with hand therapy follow-up. The transarticular wire was removed at 6 weeks. The wound healed well (Fig. 5) and at 6-week postoperatively, the DASH score was 0.
Tissue culture and gram staining was negative. Histology of the excised material revealed an epidermal cyst measuring 12 × 10 × 8 mm (Fig. 6). Macroscopically, it showed a white cystic piece of tissue measuring up to 12 mm in diameter. Microscopically, the sections showed a simple cyst lined by keratinizing squamous epithelium with retained granular layer. The epithelium ranged from a few cell layers to multiple layers. Features were diagnostic of an epidermal cyst.
There are a number of differential diagnoses to consider when confronted with an osteolytic lesion of the distal phalanx. When there is a cortical destruction, as was seen in this case, a malignant lesion must be ruled out. Primary malignancies in the distal phalanx are rare, and most malignant lesions are metastatic deposits, such as those arising from primary lung carcinomas. The most common benign bone lesions are enchondromas, but other benign tumors to consider are subungual exostoses and keratoacanthomas. In rare cases, soft-tissue tumors such as glomus tumors and schwannomas can cause bony erosion in the underlying bone, which can present as an osteolytic lesion. In addition, intraosseous epidermoid inclusion cysts, which are not true neoplasms, usually present as well-defined cystic cavities within the distal phalanx. Finally, there are a range of systemic conditions that can present as osteolytic lesions, including infections, sarcoidosis, tophaceous gout, and brown tumors secondary to hyperparathyroidism. We focused our literature review on differentiating between enchondromas and intraosseous epidermoid inclusion cysts. Clinically, both enchondromas and intraosseous epidermoid inclusion cysts present with swelling and tenderness of the affected phalanx, whilst maintaining full movement at the neighboring joints. Both lesions predispose the bone to fractures, and frequently the lesions are picked up as an incidental finding following a pathological fracture. Despite their similarities, there are a few features that assist in the clinical distinction between enchondromas and epidermoid inclusion cysts. First, in comparison to intraosseous epidermoid inclusion cysts, which are most common in the distal phalanges, enchondromas typically present in the proximal phalanx, and are least commonly found in the distal phalanx [3]. In addition, intraosseous epidermoid inclusion cysts are most common in young adult males, whereas enchondromas affect men and women equally [4, 5]. However, the prevalence of enchondromas is so much greater than that of intraosseous epidermoid inclusion cysts [6] that even a lesion in the distal phalanx of a man is more likely to be an enchondroma than an intraosseous epidermoid inclusion cyst. Although the pathogenesis of intraosseous epidermoid inclusion cysts is uncertain, the dominant hypothesis is that the cysts are caused by trauma, and patients classically report preceding mild trauma to the nailbed or phalanx [4]. In 2009, Momeni et al. [7] presented a series of seven cases of distal phalangeal bone cysts; four of which were enchondromas and three intraosseous inclusion epidermoid cysts. All four patients with epidermoid cysts had a history of trauma up to 8 years before presentation, whereas just one patient with an enchondroma had a history of injury. In our case, the patient denied a previous traumatic event; however, his occupation as a hairdresser may have predisposed him to some minor trauma, leading to the formation of an intraosseous epidermoid inclusion cyst. Radiologically, both lesions have a similar appearance. On X-ray, the lesions present as well-defined, osteolytic lesions of the phalanx with bone expansion and cortical thinning which may be associated with a breach in the cortical surface. In both lesions, MRI shows a well-circumscribed lesion of fluid signal. Subtle radiological differences can occur: Enchondromas typically involve the proximal aspect of the distal phalanx, whereas intraosseous inclusion cysts are classically found in a subungal location [4]. In our case, the location of the intraosseous inclusion cyst was atypical, as the cyst was located in the proximal part of the distal phalanx. Thus, the lesion masqueraded as an enchondroma. In addition, enchondromas may show spotty, stippled calcifications within the body of the lesion on plain radiograph, which is not seen in intraosseous epidermoid inclusion cysts [8]. Intraoperatively, enchondromas appear as cartilaginous lesions, whereas intraosseous epidermoid cysts contain a whitish-yellow cheese-like substance. Ultimately, however, the definitive diagnosis of both lesions is histological. On histological examination, enchondromas appear as lobules of hyaline cartilage encased by bone and covered by perichondrium. In comparison, histological examination of intraosseous inclusion epidermoid cysts shows a cyst wall composed of keratinized stratified squamous epithelium with keratin debris. In the case of management, both enchondromas and intraosseous epidermoid cysts are managed by marginal excision with local curettage. Synthetic bone grafting is advised to reduce the risk of pathological fractures, particularly in physically active patients [9] and to avoid any donor-site morbidity. However, despite their similar management, there may be a higher recurrence rate following curettage and bone grafting for intraosseous epidermoid cysts than for enchondromas [10].
In conclusion, it is important to consider intraosseous epidermoid cysts in the differential of cystic lesions of the distal phalanx. Factors that increase the probability that the lesion is an intraosseous epidermoid cyst are when the patients are young males, with the previous trauma at the site of the lesion. Radiographic appearances of intraosseous epidermoid cysts include the absence of calcification within the lesion and the location of the lesion in the subungal part of the distal phalanx.
It is sometimes difficult to pre-operatively differentiate between cystic lesions in the distal phalanx. It is imperative to consider salient features which, if present, should alert treating clinicians the possibility of an intraosseous epidermoid inclusion cyst.
References
- 1.Ruchelsman D, Laino D, Chhor K, Steiner GC, Kenan S. Digital intraosseous epidermoid inclusion cyst of the distal phalanx. J Hand Microsurg 2010;2:24-7. [Google Scholar]
- 2.Roth, SI. Squamous cysts involving the skull and distal phalanges. J Bone Joint Surg Am 1964;46:1442-50. [Google Scholar]
- 3.Schajowicz F, Aiello CL, Slullitel I. Cystic and pseudocystic lesions of the terminal phalanx with special reference to epidermoid cysts. Clin Orthop Relat Res 1970;68:84-92. [Google Scholar]
- 4.Simon K, Leithner A, Bodo K, Windhager R. Intraosseous epidermoid cysts of the hand skeleton: a series of eight patients. J Hand Surg Eur Vol 2011;36:376-8. [Google Scholar]
- 5.Miwa S, Okamoto H, Yamada S, Kawaguchi Y, Endo K, Aiba H, et al. Distribution of solitary and multiple enchondromas of the hand. In Vivo 2019;33:2235-40. [Google Scholar]
- 6.Lubahn J, Bachoura A. Enchondroma of the hand: Evaluation and management. J Am Acad Orthop Surg 2016;24:625-33. [Google Scholar]
- 7.Momeni A, Iblher N, Herget G, Bley T, Stark GB, Bannasch H. Distal phalangeal bone cysts: differentiation of enchondromata and epidermal cysts. J Hand Surg Eur Vol 2010;35:144-5. [Google Scholar]
- 8.Larbi A, Viala P, Omoumi P, Lecouvet F, Malghem J, Cyteval C, et al. Cartilaginous tumours and calcified lesions of the hand: A pictorial review. Diag and Intervent Imaging 2013;94:395-409. [Google Scholar]
- 9.Sasaki H, Nagano S, Shimada H, Nakashima T, Yokouchi M, Ishidou Y, et al. Intraosseous epidermoid cyst of the distal phalanx reconstructed with synthetic bone graft: A report of two cases. J Orthop Surg (Hong Kong) 2017;25:2309499016684096. [Google Scholar]
- 10.Lincoski C, Bush D, Millon S. Epidermoid cysts in the hand. J Hand Surg Eur Vol 2009;34:792-6. [Google Scholar]