Timely diagnosis and treatment of coccidioidomycosis osteomyelitis are challenging. The correct combination of curettage and antifungal therapy is necessary to avoid further bone destruction.
Dr. Rubén Daniel Arellano Pérez Vertti, Department of Orthopaedic Surgery, Universidad Autónoma de Coahuila, Facultad de Medicina Torreón, Avenida Morelos 900 Oriente, Zip Code 27000, Torreón Coahuila, Mexico. E-mail: arellanodaniel1969@gmail.com
Introduction: Coccidioides immitis is a fungus that develops in endemic areas characterized by dry climates, with little rainfall and easy aerial dissemination. The most common form of infection is pulmonary coccidioidomycosis, although it is often asymptomatic. There are non-respiratory forms of this disease. Osteomyelitis is an extrapulmonary manifestation of C. immitis infection. Symptoms are usually nonspecific and radiographic findings are often confused with bone tumors. Treatment of coccidioidal osteomyelitis is often challenging.
Case Presentation: We report a case of a 3-year-old preschool girl from an endemic area for coccidioidomycosis who presented with pain and swelling on her left ankle. Initially, antibiotic treatment is administered for a suspected insect bite. However, her symptoms worsened and X-rays showed a lytic-like lesión. She was admitted to the hospital for biopsy and drainage surgery. The histopathological study confirms coccidioidomycosis osteomyelitis. She was started on long-term anti-fungal treatment. At 6-month follow-up, symptoms and signs of infection have been solved and X-ray image shows evidence of bone healing.
Conclusion: It is important to take into account aspects related to exposure to this fungus, such as the patient’s place of residence and recent trips so that the diagnostic and therapeutic approach is appropriate. Coccidioidal osteomyelitis is an infrequent pathology, especially in patients without other comorbidities. Treatment is complex and often requires not only antifungal drugs but also surgical debridement.
Keywords: Osteomyelitis, Coccidioides immitis, tibial.
Coccidioides immitis is the fungus responsible for causing coccidioidomycosis whose geographical distribution is endemic in various regions of Mexico and the world. It develops in desert areas, with dry soils, little rainfall, and where dust storms are frequently caused, which favors the distribution and inhalation of spores [1, 2]. Thus, the inhalation of the spores can cause variable degrees of respiratory disease, although a significant percentage of patients are asymptomatic. In addition to the respiratory condition, coccidioidomycosis can affect other organs, such as the central nervous system and the musculoskeletal system among others. Pérez et al. reported the first case of coccidioidal osteomyelitis in the city of Torreón Coahuila, which is a region located north of Mexico, with climatic and soil characteristics that allow the development and dissemination of C. immitis [3]. The symptomatology of coccidioidal osteomyelitis is often nonspecific and the most frequent radiological characteristic of coccidioidal osteomyelitis is the presence of a lytic lesion, which is mainly observed in the metaphyseal areas; these lesions are similar to skeletal tumors, so other imaging and laboratory studies are necessary to obtain the correct diagnosis, the timely treatment and evaluate the existence of extension to other tissues [4].
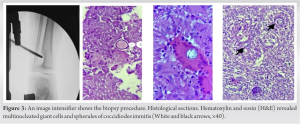
A 3-year-old Hispanic female, from Francisco I. Madero, Coahuila, Mexico, presented to pediatric orthopedic service at Hospital Los Angeles, with a 2-month history of pain and swelling in her left ankle. Her parents reported a history of the upper respiratory tract infections and fever; no recent trauma was reported. Before admission to this medical unit, the patient was treated for a suspected insect bite in her left ankle; she was prescribed antibiotics, anti-inflammatories, and abscess drainage, but pain, swelling, and redness increased. On hospital admission, she complained of localized pain and increased volume and redness in the lateral malleolus of the left ankle. At that time, there was no evidence of pus or abnormal discharge in that region. She was afebrile with stable vital signs (Fig. 1). Imaging studies were indicated in which a well-defined lesion with a lytic appearance was observed in the distal metaphyseal region of the left tibia (Fig. 2). Given the possibility of a tumor disease, a magnetic resonance image was carried out, and a hyperintense metaphyseal mass was reported magnetic resonance imaging with extension to the growth physis, suggestive of osteomyelitis (Fig. 2).
Laboratory tests reported an increase in white blood cell count, erythrocyte sedimentation rate, and C-reactive protein (CRP) rate (11,600 cells/µl, 100 mm/h, and 130 mg/L, respectively). In addition, serum antibodies specific for C. immitis were reported with increased IgM (0.338) and IgG (1.608) titers. Fluconazole therapy was then started at a dose of 7 mg/kg/day (100 mg/day) and surgery for biopsy was scheduled. No growth of C. immitis was observed after the culture of samples. However, the histopathological study revealed the presence of multinucleated giant cells, one of which has a spherule of coccidioidomycosis inside (Fig. 3).
Surgical debridement and curettage of the granuloma in the distal tibia were performed and an advancement flap was made to cover the skin defect (Fig. 4). The patient continued with medical treatment based on anti-inflammatory drugs (ibuprofen 30 mg/kg/day) and antifungal medication at the dose indicated above (fluconazole). She was discharged from the hospital 24 h after the procedure in a non-weight-bearing limb-protecting splint. Three weeks after surgery, the surgical wound showed complete healing, no infection signs and flap integration were observed. Six weeks after surgery, the splint was removed and the patient was instructed to start partial weight-bearing. Antifungal treatment with fluconazole was continued at the specified dose. Eight weeks after surgery, the patient had full weight bearing on her limb. She had no pain and the surgical area showed signs of complete healing, with no signs of infection recurrence. Finally, after 6 months of follow-up, all symptoms and signs of infection resolved and radiologic studies showed evidence of bone healing (Fig. 5). The patient continues long-term therapy with fluconazole at the dose previously described.
We present this case of a preschool female from Francisco I. Madero, Coahuila, Mexico, a city located in the Comarca Lagunera which is a large desert area whose characteristics are conducive to the development and spread of C. immitis [3]. In Mexico, the prevalence of C. immitis infection is highly variable. Thus, rates of 10% have been described in regions of Tijuana and up to 93% in some communities of the state of Coahuila [5]. Although inhalation of the spores is usually asymptomatic, most commonly causes pulmonary symptoms which range from flu-like symptoms to severe pneumonia and extrapulmonary dissemination [6]. The symptoms of coccidioidal osteomyelitis are usually non-specific and sometimes, there are no previous manifestations of lung disease; so it is important to highlight the index of suspicion, especially in reported endemic areas. Thus, the complementary tests will allow an early and accurate diagnosis. Indeed, laboratory testing may reveal elevated inflammatory markers (erythrocyte sedimentation rate, CRP) although definitive diagnosis is confirmed with antibody testing, tissue culture, and histologic staining [7]. Torres-Nájera et al. observed that active lung disease due to coccidioidomycosis could be demonstrated in only 11% of the subjects included in their study [8]. Treatment of coccidioidal osteomyelitis is often difficult and relies on the administration of antifungal medications as well as debridement and curettage. Azoles are the recommended antifungal drugs (i.e., fluconazole). Amphotericin B is no longer recommended due to adverse effects and toxicity related to this drug [9]. The efficacy of treatment should be monitored through close follow-up of patients, although serial radiographs and Coccidioides antibody titers may also be helpful [10].
Given that up to 40% of cases of pulmonary coccidioidomycosis may be asymptomatic and the skeletal manifestations non-specific, it is important to take into account aspects related to exposure to this fungus, such as the patient’s place of residence and recent trips so that the diagnostic and therapeutic approach is appropriate. Coccidioidal osteomyelitis is an infrequent pathology, especially in patients without other comorbidities. Treatment is complex and often requires not only antifungal drugs but also surgical debridement.
Coccidioidal osteomyelitis should be considered for the diagnostic and therapeutic approach of patients living in endemic areas, with or without respiratory symptoms, as well as pain, discharge, and bone lesion with a lytic appearance in imaging studies.
References
- 1.Hirschmann JV. The early history of coccidioidomycosis: 1892-1945. Clin Infect Dis 2007;44:1202-7. [Google Scholar]
- 2.Hector RF, Laniado-Laborin R. Coccidioidomycosis a fungal disease of the Americas. PLoS Med 2005;2:e2. [Google Scholar]
- 3.Verduzco E, Portales A, Monjardín S. Características clínicas y epidemiológicas de la coccidioidomicosis en la Comarca Lagunera. Salud Pública Méx 1965;7:397-402. [Google Scholar]
- 4.Ellerbrook L, Laks S. Coccidioidomycosis osteomyelitis of the knee in a 23-year-old diabetic patient. Radiol Case Rep 2015;10:1034. [Google Scholar]
- 5.Mondragón-González R, Méndez-Tovar LJ, Bernal-Vázquez E, Hernández-Hernández F, López-Martínez R, Ríos-Rosas C, et al. Detección de infección por Coccidioides immitis en zonas del estado de Coahuila, México. Rev Argent Microbiol 2005;37:135-8. [Google Scholar]
- 6.Chiller TM, Galgiani JN, Stevens DA. Coccidioidomycosis. Infect Dis Clin North Am 2003;17:41-57. [Google Scholar]
- 7.Blair JE. State-of-the-art treatment of coccidioidomycosis skeletal infections. Ann N Y Acad Sci 2007;1111:422-33. [Google Scholar]
- 8.Torres-Nájera M, De la Garza-Galván, S, Cerda-Flores RM, Nocedal-Rustrián FC, Calderón-Garcidueñas AL. Coccidioidomicosis osteoarticular: Estudio clinicopatológico de una serie de 36 pacientes mexicanos. Rev Invest Clín 2006;58:211-26. [Google Scholar]
- 9.Berli JU, Campbell WN, Katz RD. Coccidioidomycosis causing osteomyelitis of the hand in an immunocompetent patient. Hand (N Y) 2015;10:562-4. [Google Scholar]
- 10.Galgiani JN, Ampel NM, Blair JE, Catanzaro A, Geertsma F, Hoover SE, et al. 2016 Infectious diseases society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis 2016;63:e112-46. [Google Scholar]