Better understanding and management of the posterior column in complex intra-articular tibial plateau fracture is needed for improved functional outcome.
Dr. M Mohamed Sameer, Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai - 113, Tamil Nadu, India E-mail: samsortho@gmail.com
Aim: The aim of this study was to study the functional and radiological outcome after surgical fixation of complex intra-articular tibial plateau fractures managed by three-column concept.
Materials and Methods: Ten patients with complex intra-articular tibial plateau fractures were included in this study. They were classified according to the three-column concept based on X-ray and computed tomography. All of them underwent osteosynthesis after meticulous planning and the columns were addressed using combined approaches. Results: We obtained good to excellent radiological and functional outcomes with the column-based fixation of the intra-articular tibial plateau fractures. About 90% of the patients were able to return to pre-injury level of activity without complications.
Conclusion: The posterior column is a vital component of the tibial plateau and needs to be separately addressed. Three-column concept is a beneficial adjunct, especially in complex and biplanar intra-articular tibial plateau fractures, both as a diagnostic and a pre-operative planning tool.
Keywords: Tibial plateau, three-column concept, osteosynthesis, intra-articular.
Classification of intra-articular tibial plateau fractures not only helps in estimating the severity of the injury but also planning the management and predicting the prognosis after osteosynthesis. Many such classifications exist for proximal tibial intra-articular fractures [1, 2, 3, 4, 5], but Schatzker classification is still widely used. Complex intra-articular tibial plateau fractures defined as fractures running in both sagittal and coronal planes are usually categorized as Type V and VI in Schatzker classification and type C fracture in the AO/OTA classification. Most traditional classification do not lay any emphasis on the involvement of the posterior column and fractures in coronal plane since it was considered uncommon [5]. With the routine usage of computed tomography (CT) and three-dimensional (3D) reconstruction in evaluating these complex fractures, the involvement of posterior column is found to have an incidence of 28.8% [6]. Management of these fractures, especially involving the posterior column, are daunting due to difficulty in access, reduction, and maintaining stability.
Newer classifications systems describing multiple columns in proximal tibia based on the multiplanar fractures topography using helical CT scanning and 3D reconstruction were introduced to aid in better planning of osteosynthesis, choice of surgical approaches, and anatomical restoration of these complex fractures [7, 8, 9].
In this study, we report the functional outcome of using “three-column concept” philosophy for complex intra-articular tibial plateau fractures and their management through combined approaches based on the three-column fixation.
Ten consecutive patients with complex intra-articular tibial plateau fractures were analyzed in this study. All the fractures were evaluated and categorized based on the “three-column fracture concept,” having at least an individual fragment present in lateral, medial, and posterior columns of proximal tibia, as proposed by Luo et al. [7]. We have subdivided posterior column fractures into posteromedial and posterolateral sections to aid in our surgical planning and management. All the patients had fractures involving at least two columns. The columns involved and the exposures used are enumerated in (Table 1).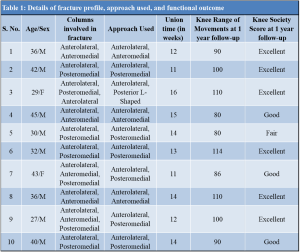
On admission, all patients were resuscitated from the trauma and compartment syndrome was ruled out. They were initially treated with ice packs and immobilized on custom-made posterior knee splint, occasionally with calcaneal pin traction, to reduce soft-tissue swelling.
Subsequently, all of them underwent a standard radiologic protocol of X-rays and CT with 3D reconstruction. We classified fractures based on the “three-column” concept as enumerated by Luo et al. [7, 8]. Whenever there is an independent articular depression associated with a break of the column wall, it was defined as a fracture of the relevant column. An isolated articular depression with intact wall is not considered as a column fracture. An anterolateral fracture combined with a separate fracture of lateral aspect of posterior column and an anteromedial fracture combined with a separate fracture of medial aspect of posterior column were considered as rare and uncharacteristic two-column involvement.
Once the soft tissue was deemed fit for surgical incision, the patients were taken up for surgical fixation. All the columns were individually managed using combined approaches. Operative approaches were planned according to the fracture pattern: Anterolateral approach for fractures involving lateral column and indirect reduction of medial column, posteromedial approach for fractures involving medial column, and medial part of posterior column. Lateral part of posterior column was approached by reverse L-shaped posterior approach in prone position, using the plane between biceps femoris and lateral head of gastrocnemius.
Submeniscal arthrotomy was additionally used when deemed necessary to ensure articular congruency of the lateral plateau. Femoral distractor, large periarticular reduction clamps, and collinear reduction device were used to aid in reduction of the fracture fragments. Depressed fragments were elevated using bone punch from below the fracture in the metaphyseal region. K-wires were used liberally to provisionally fix the fracture fragments. The fractures were stabilized using small fragment plates, reconstruction plates, or anatomic posteromedial plate posteriorly and column-specific anatomical locking plates medially and laterally. Synthetic bone graft substitutes (Hydroxyapatite blocks measuring 1.5 cm/2 cm) were used in situations, where metaphyseal bony defect was noted intraoperatively.
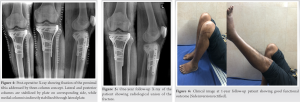
Low molecular weight heparin was started postoperatively until as deemed necessary according to risk of deep vein thrombosis. Passive knee mobilization was started after removal of drain tube. According to the fracture pattern and associated ligamentous injury, patients were gradually allowed to walk with walker frame and knee brace as tolerated after 4 weeks. Active- and active-assisted flexion was gradually increased on individual case basis. Anteroposterior and lateral radiographs were taken at 6th week, 12th week, and every 8 weeks thereafter until radiological union. All discharged patients were followed-up at 3 month intervals for 1 year. The radiological and functional outcome was evaluated based on the Knee Society Score at 1-year follow-up. An illustrative case involving complex intra-articular three-column fracture of left tibial plateau is demonstrated in (Fig. 1-6).
The average time period between injury and surgical fixation was 7 days (ranging 4–16 days). Apart from routine radiographs, CT with 3D reconstruction and magnetic resonance imaging were done for all patients. Without delaying the surgical treatment. The surgical timing, type of construct, and fixation were determined by the surgeon according to the type of fracture, number of major fragments localization, Comminution, and soft-tissue condition.
All the patients were reviewed for clinical and radiological evaluation. No patients were lost at follow-up. At final follow-up, clinical examination, radiological, and functional outcome was documented. Functional outcome was assessed based on Knee Society Score criteria at 1-year follow-up. Radiological outcome was assessed based on initial, post-operative, and final follow-up knee X-rays.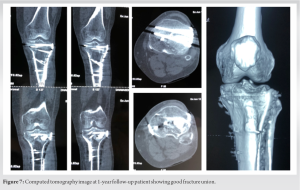
Among the ten patients with complex intra-articular tibial plateau fractures, eight were male and two were female. The mean age was 36 years old. All were closed fractures. Average delay to surgical fixation was 7 days (range 4–16 days). There was no complete ligamentous avulsion in our study necessitating repair.
All the patients were followed-up for an average of 11 months (range 9–16 months). In the immediate post-operative period, supine anteroposterior and lateral views of the knee were taken to assess the step off or gap. Five patients had post-operative anatomic reduction (0 mm step-off), while three had acceptable reduction (<2 mm step-off). The average time for radiographic bony union was 13.2 weeks (range 11–16 weeks) with no secondary displacement.
None of the patients had infection. There were no cases of intraoperative neurovascular injuries, failed internal fixation or knee varus/valgus deformity. No revision surgery was performed. However, mediolateral instability was noted in two patients and was managed conservatively with hinged knee brace in the post-operative period.
The functional outcome was evaluated based on the Knee Society Score criteria. The Knee Society Score was excellent in six, good in three, and fair in one patient. Referencing the Knee Society Score, excellent to good rate was achieved in 90% of our study. About 90% of our patients returned to their pre-injury level of activity and employment. They resumed full weight-bearing at an average of 16 weeks (range 14–22 weeks). Mean flexion at operated knee at 12 months follow-up was 96° (range 80–114°). None of the patients had extensor lag. One patient (10%) had secondary varus deformity.
Three-column classification is a relatively new concept in the operative management of complex intra-articular tibial plateau fractures. It is especially useful for multiplanar fractures involving the posterior column [7, 8]. Posterior column fracture is often the aftermath of valgus-varus stress shear [9]. It is mostly noted in a partially to completely flexed knee, when the posterior half of tibia plateau is impacted by the femoral condyles [10, 11]. It has been increasingly observed to be having a higher presentation in complex tibial fractures and often missed as this fracture pattern is often difficult to visualize on plain radiographs alone [12]. This special injury pattern has not deserved worthful notification in the AO/OTA or Schatzker classification systems. Often, the lateral posterior condyle sustains compression, while the medial posterior condyle endures split [12].
The CT with 3D reconstruction aides in better recognition of the various fragments of proximal tibial fracture, classification into columns, and subsequent surgical planning. Bicondylar and complex fracture patterns necessitate combined anterolateral and posteromedial approaches, as they provide both biomechanical and clinical benefits. The most complicated ones are the three-column fractures which include the medial, lateral, and posterior columns and they require a combination of a reversed L-shaped posterior approach and anterolateral approach for optimal fixation.
Conventionally, anterolateral approach was used for the simple tibial plateau fractures, corresponding to exclusive lateral column of the plateau such as Schatzker type I, II, and III [13, 14]. However, a combined approach is required when the fracture line ramifies, resulting in a complex pattern. Posterior column fractures are challenging and are often difficult to achieve adequate reduction and stabilization by traditional techniques and approaches. A modified posterior approach is an ideal approach for such injuries according to different fracture patterns [15]. Tao et al. advocated modified posterolateral approach in treating posterolateral shearing tibial plateau fractures [11]. Luo et al. advocated management of posterolateral fractures by inverted L-shaped posterior approach but encountered difficulties in exposure due to the need for splitting gastrocnemius [7]. Fernandez DL advocated percutaneous reduction through anterolateral approach to treat posterolateral fracture but encountered secondary loss of anatomic reduction [16]. Yu et al. reported partial or total excision of fibular head to aid in reduction and fixation of posterior and lateral column [17]. This technique ruins the normal lateral stability of the knee at the expense of providing better exposure for reduction. Bhattacharyya described posteromedial popliteal approach, requiring large skin flap and extensive soft tissue dissection with close proximity to neurovascular structures [6]. We used anterolateral approach for lateral and medial columns; posteromedial approach for medial; and medial aspect of posterior columns and posterolateral approach for lateral aspect of posterior column. Intraoperative neurovascular injury, difficult surgical exposure requiring change of patient and limb positioning and the need of combined approaches for complex fractures, must be borne in mind during posterior column stabilization.
Chen et al. advocated use of screws, reconstruction plates or T-shaped plate, based on fracture morphology [9]. Zeng et al. [18] propagated the use of posterior T-shaped anti-glide plate for split fractures, which offered better biomechanical stability. Newer anatomical locking plates for the posterior column help in preventing bony collapse and secondary loss of reduction. Three-column concept is a beneficial adjunct in multiplanar intra-articular tibial plateau fractures especially if it involves the posterior column. It serves as both an efficient diagnostic tool and for meticulous pre-operative planning. We used column-based anatomical locking plate for medial and lateral column. Recon plates, distal radius plates, small fragment plates, and screws were used to stabilize the posterior column, depending on the complexity of the fracture.
With our column-based operative management and early rehabilitation, we were able to achieve six excellent and three good results (overall 90% acceptable result). We did not encounter any major complications apart from one case (10%) of secondary varus deformity and two cases of mediolateral instability (20%). Our results were comparable with Chang et al., who reported 87.5% acceptable results and encountered one case of wound dehiscence [19].
Three-column classification is a novel fixation concept in the management of complex intra-articular tibial plateau fractures. CT scan with 3D reconstruction of injured knee helps in determining fracture tomography, pre-operative planning, fixation technique, and initiation of adequate post-operative mobilization. Individually, addressing each column of tibial plateau in these complex fracture scenarios helps to achieve anatomical reduction and rigid fixation. This, in turn, can facilitate early rehabilitation resulting in good radiological and functional outcome and prevent complications associated with these complex injuries.
Although the tibia plateau fractures have been described under numerous classification systems, the posterior column/coronal split is scarcely addressed. It is a vital component of the complex intra-articular tibial plateau fracture which needs better understanding and addressing to improve functional outcome.
References
- 1.Schatzker J, McBroom R, Bruce D. The tibial plateau fractures. The Toronto experience 1968--1975. Clin Orthop Relat Res 1979;138:94-104. [Google Scholar]
- 2.Moore TM. Fracture--dislocation of the knee. Clin Orthop Relat Res 1981;156:128-40. [Google Scholar]
- 3.Wahlquist M, Iaguilli N, Ebraheim N, Levine J. Medial tibial plateau fractures: A new classification system. J Trauma 2007;63:1418-21. [Google Scholar]
- 4.Khan RM, Khan SH, Ahmad AJ, Umar M. Tibial plateau fractures. A new classification schemes. Clin Orthop Relat Res 2000;375:231-42. [Google Scholar]
- 5.Maripuri SN, Rao P, Manoj-Thomas A, Mohanty K. The classification systems for tibial plateau fractures: How reliable are they? Injury 2008;39:1216-21. [Google Scholar]
- 6.Bhattacharyya T, McCarty LP, Harris MB, Morrison SM, Wixted JJ, Vrahas MS, et al. The posterior shearing tibial plateau fracture: Treatment and results via a posterior approach. J Orthop Trauma 2005;19:305-10. [Google Scholar]
- 7.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 2010;24:683-92. [Google Scholar]
- 8.Zhu Y, Yang G, Luo CF, Smith WR, Hu CF, Gao H, et al. Computed tomography-based three-column classification in tibial plateau fractures: Introduction of its utility and assessment of its reproducibility. J Trauma Acute Care Surg 2012;73:731-7. [Google Scholar]
- 9.Chen HW, Chen CQ, Yi XH. Posterior tibial plateau fracture: A new treatment-oriented classification and surgical management. Int J Clin Exp Med 2015;8:472-9. [Google Scholar]
- 10.Chang SM, Zheng HP, Li HF, Jia YW, Huang YG, Wang X, et al. Treatment of isolated posterior coronal fracture of the lateral tibial plateau through posterolateral approach for direct exposure and buttress plate fixation. Arch Orthop Trauma Surg 2009;129:955-62. [Google Scholar]
- 11.Tao J, Hang DH, Wang QG, Gao W, Zhu LB, Wu XF, et al. The posterolateral shearing tibial plateau fracture: Treatment and results via a modified posterolateral approach. Knee 2008;15:473-9. [Google Scholar]
- 12.Yang G, Zhai Q, Zhu Y, Sun H, Putnis S, Luo C. The incidence of posterior tibial plateau fracture: An investigation of 525 fractures by using a CT-based classification system. Arch Orthop Trauma Surg 2013;133:929-34. [Google Scholar]
- 13.Georgiadis GM. Combined anterior and posterior approaches for complex tibial plateau fractures. J Bone Joint Surg Br 1994;76:285-9. [Google Scholar]
- 14.Hoppenfeld S, De Boer P. Surgical Exposures in Orthopaedics. Philadelphia: JB Lippin-cott; 1984. [Google Scholar]
- 15.Kenneth AE. Split depression posterolateral tibial plateau fracture: Direct open reduction and internal fixation. Tech Knee Surg 2005;4:257-63. [Google Scholar]
- 16.Fernandez DL. Anterior approach to the knee with osteotomy of the tibial tubercle for bicondylar tibial fractures. J Bone Joint Surg Am 1988;70:208-19. [Google Scholar]
- 17.Yu B, Han K, Zhan C, Zhang C, Ma H, Su J. Fibular head osteotomy: A new approach for the treatment of lateral or posterolateral tibial plateau fractures. Knee 2010;17:313-8. [Google Scholar]
- 18.Zeng ZM, Luo CF, Putnis S, Zeng BF. Biomechanical analysis of posteromedial tibial plateau split fracture fixation. Knee 2011;18:51-4. [Google Scholar]
- 19.Chang SM, Hu SJ, Zhang YQ, Yao MW, Ma Z, Wang X, et al. A surgical protocol for bicondylar four-quadrant tibial plateau fractures. Int Orthop 2014;38:2559-64. [Google Scholar]








