Inflammation or infarction of intra-articular tenosynovial giant cell tumors can trigger irritable hip findings that resembles septic arthritis in children.
Dr. Mehmet Salih Söylemez, Yaprak Street, Acibadem District, No 32, D:12, Uskudar/Istanbul. E-mail: slhsylmz@gmail.com
Introduction: Intra-articular tenosynovial giant cell tumor (IATGCT) is a type of tenosynovial giant cell tumor that typically occurs in the synovial tissues of large joints. It is also known as pigmented villonodular synovitis. Acute onset of the pain with irritable hip symptoms is very rare. In this paper, we presented two adolescents with acute onset of hip pain mimicking septic arthritis diagnosed with intra-articular tenosynovial giant cell tumor.
Case Report: Healthy two adolescents, one male (14-year-old) and the other girl (15-year-old) with no history of the previous trauma or significant comorbidities were presented complaining of acute onset of hip pain to our emergency room. Although initial possible diagnosis was septic arthritis for both cases, laboratory findings were unequivocal for septic arthritis and magnetic resonance imaging (MRI) showed an intra-articular nodular mass. An open resection was performed and pathological evaluation revealed the masses to be intra-articular tenosynovial giant cell tumor. After 26 and 17 months follow-up there was no pain neither with activity nor in rest, hip range of motion was within normal ranges. There was no recurrence, avascular necrosis or destruction detected on control MRI for both patients.
Conclusion: IATGCT is a rare disease of the pediatric population involving the hip. Inflammation or infarction of the lesion can trigger irritable hip findings in children. This diagnosis should be kept in mind mainly in cases with serohemorrhagic aspirate and unequivocal laboratory findings.
Keywords: Pigmented villonodular synovitis, intra-articular giant cell tumor, hip, septic arthritis, differential diagnosis.
Intra-articular tenosynovial giant cell tumor is a type of tenosynovial giant cell tumor that typically occurs in the synovial tissues of large joints. It is also known as pigmented villonodular synovitis (PVNS). PVNS have localized (nodular) and diffuse variants, classified on the basis of the extent of synovial or tenosynovial involvement [1]. The localized (nodular) and diffuse forms are both identical histologically. However, in 2007, Rubin had recommended the use of the term tenosynovial giant cell tumor for nodular lesions [2]. Although tenosynovial giant cell tumors are extra-articular lesions and mostly arise from tendon sheets, intra-articular nodular lesions arising from joint synovium have similar histological characteristics. Thus these intra-articular lesions are termed as Intra-articular tenosynovial giant cell tumors.
PVNS has bimodal distribution. They mostly seen in second and fifth decade of life and has an estimated incidence of 0.0002–0.0008% [3]. Most common location for PVNS in children is the knee, ankle is the second and the hip comes later [4]. Insidious onset of pain, swelling of the joint and limitation of ROM are common clinical findings in children as well. However, plain radiographs are unremarkable in most children and acute onset of the pain with irritable hip symptoms is very rare. In this paper, we presented two adolescents with acute onset of hip pain mimicking septic arthritis diagnosed with intra-articular tenosynovial giant cell tumor.
Case 1
A 14-year-old male patient with no history of previous medical disease or previous trauma was presented to our emergency department complaining of the left hip pain and inability of weight bearing. Detailed history revealed that these complaints started 5 days ago and worsened by time. There was severe pain in the hip during the examination. Patient was afebrile and initial X-rays did not reveal any specific pathology. A primary laboratory survey showed elevated C-reactive protein levels (CRPs) (4.5 mg/dl [normal ranges 0.0–0.5 mg/dl]) normal complete blood count (white blood cell [WBC]: 5.91 × 103/uL), and a very low increase in sedimentation (18 mm/h [normal ranges 0–15 mm/h]). Although findings were not perfectly consistent with septic arthritis, the presence of limitation in weight bearing and increase in CRP levels increased the suspicion for septic arthritis of the hip. Thus, an aspiration under fluoroscopy guidance was performed at the 2nd h after first admission. The aspirate had a serohemorrhagic nature. Joint aspirate revealed 12.000 red blood cells (RBC)/mL, 37.170 WBC/mL with 85% neutrophils, and a negative Gram stain which enabled us exclude septic arthritis from differential diagnosis.
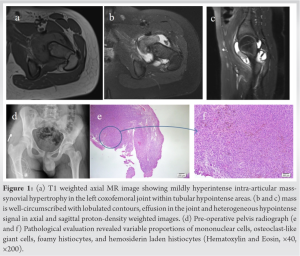
An magnetic resonance imaging (MRI) with IV contrast obtained after 24 h from first admission showed a 3 × 4 cm localized synovial nodule with mild heterogeneous synovial contrast enhancements and without bony invasion (Fig. 1a, b, c). The patient was diagnosed to have a nodular form of PVNS and was operated through an anterior approach. The lesion was located in antero-inferior recess, had connections with synovium only at that point, was pink-brown and lobulated. Histomorphological findings were evaluated as intra-articular tenosynovial giant cell tumor-like proliferation, since it did not form a complete mass formation and was interpreted as reactive changes (Fig. 1d and e).
Last follow-up was at postoperative 26th months. There was no pain neither with activity nor in rest, hip range of motion (ROM) was within normal ranges. An MRI performed at post-operative 18th month revealed that there was no recurrence, avascular necrosis or destruction.
Case 2
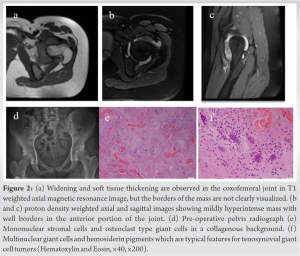
A healthy 15-year-old female patient was presented complaining of left hip pain and inability of weight bearing starting 16 h ago. Detailed history did not reveal any traumatic or significant previous medical event. Patient could not walk or sit and the hip was very painful during examination. X-rays did not reveal any pathological sign. Patient was afebrile and primary septic workup showed normal CRP levels (0.2 mg/dl [normal ranges 0.0–0.5 mg/dl]) increased WBC (15.0 × 103/uL), and a very low increase in sedimentation (16 mm/h [normal ranges 0–15mm/h]). Although findings were not perfectly consistent with septic arthritis, the presence of limitation in weight bearing and increase in WBC levels prevented us from excluding septic arthritis from differential diagnosis. Thus, an aspiration under fluoroscopic guidance was performed at the 3rd h after first admission. The aspirate had a haemopurulent nature. The aspirated fluid revealed 1.181.000 RBC/mL and 64.580 leukocytes/mL with 95% neutrophils. Moreover, Gram-negative bacteria were detected in Gram staining. However, positive Gram staining was supposed to be contamination as Gram-negative bacteria are not common causatives for septic arthritis for this age. An urgent MRI was supposed to evaluate the hip for possible pelvic pathologies including metaphyseal or pelvic osteomyelitis. MRI obtained at the 5th h after submission revealed a localized synovial nodule without any bony invasion (Fig. 2a, b, c). As the aspirate was haemopurulent, WBC levels had increased, there was severe pain in examination and the gram staining showed gram negative bacteria, patient was suspected to have an infected intra-articular tenosynovial giant cell tumor and an urgent surgery was planned.
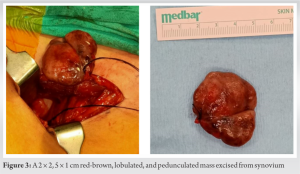
Patient was operated via an anterior approach. The lesion was located in anterior recess, had only one pediculum connecting with synovium, other parts of capsule was healthy and white. There was only a small amount of dark haemopurulent fluid in the joint. In addition, the lesion was dark brown macroscopically, as seen in necrotic tissues, and its pedicle was black, probably due to torsion or venous occlusion (Fig. 3). Although, Gram-negative bacteria were seen in Gram staining later cultures did not yield a positive result. Nevertheless, patients took septic-arthritis treatment including 3 weeks of intravenous and 3 weeks of oral antibiotics postoperatively.
Histomorphological evaluations revealed mononuclear stromal cells and osteoclast type giant cells in collagenous background, multinuclear giant cells, and hemosiderin pigments which are typical features for tenosynovial giant cell tumor (Fig. 2d and e) Last follow-up was at postoperative 17th months. There was no pain neither with activity nor in rest, hip ROM was within normal ranges. An MRI performed at post-operative 12th month revealed that there was no recurrence, avascular necrosis, or destruction.
The differential diagnosis of acute onset of hip pain in a child with uncertain laboratory findings include; septic arthritis, periarticular infections, transient synovitis, Legg-Calve-Perthes disease, synovial chondromatosis, and juvenile idiopathic arthritis [5]. No current data exist about the incidence of PVNS in children, but it is estimated to be substantially lower than in the general population [3]. Hip involvement is rare both in adults and children. Tenosynovial giant cell tumor is usually presented with insidious joint pain, swelling, limited joint function and soft tissue mass [6]. The mean duration of symptoms before presentation for PVNS in a study of 166 cases have been reported to be 10 months for nodular intra-articular disease, and no patients in that group had presented with acute symptoms [7]. Our literature review revealed nine cases from four case reports and one case series reporting hip involvement in children [1, 4, 5, 8, 9]. Of these, only four cases had intra-articular tenosynovial giant cell tumor hip involvement presenting with acute irritable hip symptoms (Table 1).
Regarding the radiological investigations, MRI plays an important role in diagnosis, staging, preoperative planning and clinical follow-up of synovium based lesions. PVNS is observed as a mass or mass-like synovial proliferation on MRI. T1 and T2 signals of lesions vary low to intermediate (according to concentration of hemosiderin) and predominantly high-signal is seen in short tau inversion recovery sequence. Differential diagnosis includes rheumatoid arthritis, hemophilic arthropathy, septic arthritis, tuberculosis, and synovium based neoplastic processes. Gradient echo images (GRE) can be very useful to differentiate these entities when combined with laboratory surveys. IATGCT lesions show typically low signal in GRE sequence and magnetic susceptibility (blooming) artifacts can be seen due to hemosiderin depositions [6].
The reason for acute inflammation and irritable hip symptoms is unknown. Saadat et al. [8] had hypothesized that the trauma may have caused the torsion/bleeding and/or infarction of the nodular lesion which may be the reason for hemarthrosis in their case. Early coagulative necrosis (infarction) after torsion may also have played a role in neutrophil chemotaxis. Thus, the neutrophil recruitment may have contributed to the fever, acute pain, and other clinical features of a septic hip. However, for our cases, there was no trauma, In case 1, the joint aspirate was of light serohemorrhagic character, like the fluids aspirated in knee PVNS cases. The fact that the patient’s complaints developed gradually within 5 days suggests that neutrophil attack may have caused inflammation of the lesion, and therefore an increase in joint fluid, leading to acute irritable hip findings. In case 2, the joint aspirate was of dark haemopurulent character because aspiration was done under fluoroscopy but not ultrasound, we may have aspirate from the center of the lesion. In addition, the pedicle of the lesion was so thin (1 mm wide and 3 cm long) that it could be torsioned with a very simple movement. In a lesion with such a thin pedicle, venous stasis and infarct can easily develop not only with torsion but also with mild inflammation. Similar to the pathophysiological processes that cause the development of osteomyelitis in the metaphyseal region of the bones in children, venous stasis may lead to development of a suitable breeding environment for bacteria and septic arthritis. 64,000 leukocytes, 95% of which are neutrophils, in the aspirate of the second case supports this theory. Causative bacteria can be detected in cultures in approximately 30-50% of patients in septic arthritis cases [10]. In the second case, although Gram-negative bacteria were observed in gram staining, it was considered as contamination since it was not a typical organism in adolescence and there was no growth in the culture. However, since recent studies have shown that gram-negative bacteria (especially kingella kingae) is the most common cause of septic arthritis under 4 years of age [10], this case was evaluated and treated as an infected intra-articular tenosynovial giant cell tumor in which the causative organism could not be identified.
The differentiation of diffuse and nodular forms is important as nodular and diffuse forms of the condition behave and appear differently. Diffuse form develops more insidious complaints probably leading to late diagnosis of the disease, behaves more aggressive and has a more tendency of recurrence. Late diagnosis, recurrence after resection and aggressive behavior of the diffuse form causes early articular degeneration and joint narrowing [3]. Thus, open or arthroscopic subtotal resection of the synovium remains the treatment of choice for diffuse form. Although some authors had performed arthroscopy to resect these lesions because of less invasive nature of arthroscopic technique and better visualization of the particularly hip joint, the efficacy of arthroscopic synovectomy has only been shown for the knee joint [11]. Contrary to diffuse form, TGCT have a tendency to cause episodic effusions and behave less aggressively and previous literature had showed that arthroscopic excision is effective for IATGCT for shoulder, hip knee, and ankle joints [11, 12]. Of the five cases that had been reported to present with hip symptoms, two had operated through an open approach, six had operated with arthroscopy, and one had followed by conservative means [1, 4, 5, 8, 9]. Only resection of the lesion had performed in operated cases as authors had reported that the lesions to be connected to the synovium with relatively narrow pedicles which enabled the resection of the lesion. We preferred an anterior open approach as this approach enables easy resection of the anteriorly localized lesions, debridement, and irrigation of the joint. However, for a posterior or medial localized IATGCT arthroscopic resection is recommended treatment modality [11].
Although intra-articular tenosynovial giant cell tumor is a rare disease of the pediatric population involving the hip and the acute presentation is very rare to be seen, this diagnosis should be kept in mind mainly in cases with serohemorrhagic aspirate and unequivocal laboratory findings.
Intra-articular giant cell tumor should be kept in mind in the differential diagnosis of adolescence patients presenting with irritable hip symptoms and ambiguous laboratory survey results.
References
- 1.Patel AM, Brown AG, Galambos C, Hirsch R. Pediatric pigmented villonodular synovitis mimicking a septic hip. J Clin Rheumatol 2010;16:71-3. [Google Scholar]
- 2.Rubin BP. Tenosynovial giant cell tumor and pigmented villonodular synovitis: A proposal for unification of these clinically distinct but histologically and genetically identical lesions. Skeletal Radiol 2007;36:267-8. [Google Scholar]
- 3.Stephan SR, Shallop B, Lackman R, Kim TW, Mulcahey MK. Pigmented villonodular synovitis: A comprehensive review and proposed treatment algorithm. JBJS Rev 2016;4:e3. [Google Scholar]
- 4.Higuchi C, Ohno I, Yoshikawa H. Hip joint pigmented villonodular synovitis in a young girl: A case report. J Pediatr Orthop B 2012;21:335-8. [Google Scholar]
- 5.Marshall AS, Molina AL, Reiff D, Sheets R, Conklin M. Pigmented villonodular synovitis mimicking an acute septic hip in an eight-year-old male. Cureus 2020;12:e9895. [Google Scholar]
- 6.Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: Radiologic-pathologic correlation. Radiographics 2008;28:1493-518. [Google Scholar]
- 7.Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980;59:223-38. [Google Scholar]
- 8.Saadat E, Vargas SO, Anderson M, Glotzbecker M. Pediatric intra-articular localized tenosynovial giant cell tumor presenting as an acutely irritable hip: A case report. JBJS Case Connect 2016;6:e60. [Google Scholar]
- 9.Willimon SC, Schrader T, Perkins CA. Arthroscopic management of pigmented villonodular synovitis of the hip in children and adolescents. Orthop J Sports Med 2018;6:2325967118763118. [Google Scholar]
- 10.Thomas M, Bonacorsi S, Simon AL, Mallet C, Lorrot M, Faye A, et al. Acute monoarthritis in young children: Comparing the characteristics of patients with juvenile idiopathic arthritis versus septic and undifferentiated arthritis. Sci Rep 2021;11:3422. [Google Scholar]
- 11.Noailles T, Brulefert K, Briand S, Longis PM, Andrieu K, Chalopin A, et al. Giant cell tumor of tendon sheath: Open surgery or arthroscopic synovectomy? A systematic review of the literature. Orthop Traumatol Surg Res 2017;103:809-14. [Google Scholar]
- 12.Karami M, Soleimani M, Shiari R. Pigmented villonodular synovitis in pediatric population: Review of literature and a case report. Pediatr Rheumatol Online J 2018;16:6. [Google Scholar]