rTSA is a valuable option in young patients with comminuted fracture-dislocation of the humeral head whenever associated with poor bone stock.
Dr. Giulia Bettinelli, Orthopaedic and Traumatology Resident, Università Vita-Salute San Raffaele, Via Olgettina 60, 20132 Milano. E-mail: bettinelli.giulia@hsr.it
Introduction: Bilateral posterior fracture-dislocations of the shoulders occur quite rarely. To the best of our knowledge, this is the first case happening to a young man subjected with bilateral reverse shoulder replacement surgery in a one-step procedure.
Case Report: The authors present the case of a Caucasian, 49, alcoholic, male affected by bilateral proximal humeral fracture with posterior dislocation, provoked by an epileptic seizure, and admitted to our hospital. The patient underwent one-step bilateral reverse total shoulder replacement surgery, due the comminution of the fracture and osteopenic pattern. He carried bilateral slings for 1 month after surgery, and after the post-operative radiological evaluation at 1 month, he started with progressive active physiotherapy.
Conclusion: Opting for a total replacement instead of osteosynthesis is a valuable option in patients presenting with dislocation-comminuted fractures and alcohol intake induced osteoporosis, even if young.
Keywords: Bilateral fracture-dislocation, posterior shoulder fracture-dislocation, reverse arthroplasty
Bilateral posterior fracture with simultaneous dislocation of the shoulder occurs unfrequently [1, 2]. Roughly half of bilateral posterior dislocations are results of a convulsive seizure, in presence of an associated fracture this percentage raises to 90% [3].
Based on the fracture pattern, there are different possible therapeutical options for proximal humeral fractures: conservative treatment; with open reduction and internal fixation, closed reduction and percutaneous pinning, intramedullary nailing; with hemiarthroplasty, anatomic total shoulder arthroplasty, or reverse total shoulder arthroplasty (rTSA) [4]. The following case involves a patient with bilateral fracture-dislocation of the shoulders happened while having an epileptic seizure caused by days of ethanol withdrawal; he was then treated in a one-step procedure with bilateral rTSA.
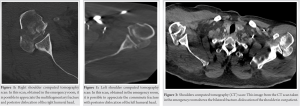
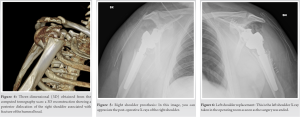
We present the case of an alcoholic Caucasian, 49, male admitted to the emergency room of San Raffaele Hospital, Milan, for an epileptic seizure. His medical history revealed that he suffered from untreated hypertension; he stated to be an alcohol abuser who had abruptly quit drinking a few days before. His weight was 100 kg by 170 cm height. After being examined by the internal medicine doctor, neurologist, and psychiatrist, and once metabolically stable, an orthopedic consult was asked because he complained of shoulder pain. On orthopedic examination, he had bilateral localized swelling, severely restricted shoulder range of movement, pain on mobilization, and no sensorimotor deficit. Shoulder X-rays and computed tomography scan (Fig. 1, 2, 3, 4) were performed, which confirmed the diagnosis of bilateral proximal humeral fracture (AO 11C3) associated with posterior dislocation.
He was taken over by the orthopedic department to schedule surgery.
Since the fracture pattern was comminuted, with a defect of the articular surface >50% and lack of structural support to maintain a reduction, it was chosen to perform a double shoulder replacement [5]. Furthermore, considering his secondary osteoporosis, we opted against osteosynthesis as there would be a high risk of avascular necrosis in the early-mid period after surgery, with subsequent need for a second corrective surgery. This was secondary to the fact that the patient is an alcohol abuser, so his bone stock was expected to be impaired. Considering his overall clinical situation, we evaluated that the patient would have been better off receiving a prosthesis. Surgery was performed in a beach chair position and took place under general anesthesia. Since the patient is right-handed, it was decided to begin with the dominant side. Using a deltopectoral approach, a cementless reverse shoulder prosthesis LIMA was implanted. A new sterile surgery field was draped on the left side as soon as the right surgical wound had been sutured. The same procedure was then performed for the left limb (Fig. 5, 6).
A bilateral protective sling was positioned before the patient woke up from anesthesia, to avoid excessive motion and rotation of the upper limbs. The surgery lasted 2 h with a successful outcome, and an uneventful post-operative recovery. Stitches have been removed 21 days post-surgery, and he started passive assisted physiotherapy. During an outpatient visit 50-days after surgery, it was decided to start with active mobilization. At 3 months after surgery, he had an outpatient control where it was highlighted a subjective improvement of the range of motion with no pain, and a significant recovery of strength. Scapula-humeral active range of motion was 0–160°, and passive 0–170°.
As previously stated, posterior shoulder dislocations are seldom events and due to the paucity of symptoms, it can be easily misdiagnosed and late diagnosed; if associated with a humeral head fracture symptoms can be more evident, however, when happening after a convulsive seizure, it can be overlooked due to the emergency scenario [6]. To the best of our knowledge, there is only one previous case in the literature of bilateral humeral fracture with posterior displacement who underwent one-step rTSA, described by Ali Azad; however, their case was about a 64-year-old man [7]. Other articles report the case of a bilateral fracture-dislocation of the shoulders treated in a staged fashion with rTSA [4], and the case of a simultaneous surgery with rTSA for a similar episode [8].
As a matter of fact, there are three possible timing options for scheduling the surgery: Staged, sequential, or simultaneous [9]. Ethanol effects on bone are well documented among which the two most relevant for this case are decreased bone marrow density in both cortical and trabecular bone, and the inhibition of the bone formation process. These lead to alcoholism being one of the main causes of secondary osteoporosis in men as well as an increased percentage fracture risk [10]. Plating complex proximal humerus fractures bring some risks in the setting osteoporotic bone. Among the common complications, the more relevant are: Avascular necrosis, non-union, loss of fixation, screw cutout, and tuberosity displacement [1, 11]. Patient age, comorbidities, bone quality, fracture morphology, and rotator cuff integrity must be considered to determine the likelihood of each of these complications to determine if locked plating is appropriate [7]. The choice between hemiarthroplasty and shoulder arthroplasty is influenced by the patient’s age, bone density, and fracture’s pattern. A study comparing hemiarthroplasty and total shoulder arthroplasty at 15 years follow-up in patients below 50 years old showed that glenoid erosion was present in 72% of hemiarthroplasties, resulting in high revision rates secondary to painful glenoid arthritis [7]. The choice between anatomical or reverse arthroplasty depends on the condition of the rotator cuff. It might be wise to have both options at disposal in the operating room [12].
When facing a comminuted humeral head fracture-dislocation, pros and cons of each surgical option should be evaluated and discussed with the patient; shoulder replacement can be a viable option in comminuted fractures-dislocation whenever associated with poor bone stock.
A convulsive seizure followed by shoulder pain should always raise suspicion for posterior shoulder fracture and dislocation. rTSA is a valuable therapeutical approach for young patients with comminuted fracture-dislocation of the humeral head whenever associated with poor bone stock.
References
- 1.Jansen H, Frey SP, Doht S, Meffert RH. Simultaneous posterior fracture dislocation of the shoulder following epileptic convulsion. J Surg Case Rep 2012;2012:rjs017. [Google Scholar]
- 2.Wendling A, Vopat ML, Yang SY, Saunders B. Near-simultaneous bilateral reverse total shoulder arthroplasty for the treatment of bilateral fracture dislocations of the shoulder. BMJ Case Rep 2019;12:e230212. [Google Scholar]
- 3.Claro R, Sousa R, Massada M, Ramos J, Lourenço JM. Bilateral posterior fracture-dislocation of the shoulder: Report of two cases. Int J Shoulder Surg 2009;3:41-5. [Google Scholar]
- 4.Murphy JD, Braunlich PR, Bansal M, Edge L, Harker JN. Bilateral posterior four-part fracture-dislocation of the proximal humerus after first-time seizure. Cureus. 2021;13:e17688. [Google Scholar]
- 5.Cicak N. Posterior dislocation of the shoulder. J Bone Joint Surg Br 2004;86:324-32. [Google Scholar]
- 6.Yigit M, Yaman A, Yigit E, Turkdogan KA. The overlooked side of convulsion: Bilateral posterior fracture and dislocation of proximal humerus. J Pak Med Assoc 2016;66:621-2. [Google Scholar]
- 7.Azad A, Antonios JK, Kang HP, Omid R. Single-stage bilateral reverse total shoulder arthroplasty for bilateral posterior shoulder fracture-dislocation following seizure: A case report. Int J Surg Case Rep 2020;73:298-302. [Google Scholar]
- 8.El Rassi G, Dib N, Maalouly J, Moukarzel R, Aouad D. Bilateral reverse total shoulder arthroplasty with soft tissue release for bilateral posterior fracture dislocation after status epilepticus. Case Rep Orthop 2021;2021:5525316. [Google Scholar]
- 9.Allende C, Bustos D, Bruno P, Galera H. Two-team simultaneous open surgical treatment in bilateral shoulder fracture dislocation. Tech Hand Up Extrem Surg 2012;16:210-4. [Google Scholar]
- 10.Maurel DB, Boisseau N, Benhamou CL, Jaffre C. Alcohol and bone: Review of dose effects and mechanisms. Osteoporos Int 2012;23:1-16. [Google Scholar]
- 11.Thati B, Bodanki C, Badam VK, Reddy MV, Reddy AV. Custom 3D printed jigs in salvage reverse shoulder arthroplasty for failed four-part proximal humerus fracture fixation: A case report. J Orthop Case Rep 2020;10:25-8. [Google Scholar]
- 12.Mansat P, Bonnevialle N. Treatment of fracture sequelae of the proximal humerus: Anatomical vs reverse shoulder prosthesis. Int Orthop 2015;39:349-54. [Google Scholar]